
Ralph J. Napolitano, Jr, DPM, CWSP, FACFAS is a double board-certified podiatrist and wound care specialist physician with OrthoNeuro, a multispecialty group based in central Ohio. He specializes in medicine, surgery and wound care of the foot, ankle and lower leg. He was the first podiatrist in the state of Ohio to earn the board certification Certified Wound Specialist Physician (CWSP). Areas of special clinical interest, research and publications include general wound care and healing, diabetic foot wounds, lower limb surgical salvage and management of surgical wound complications.
Dr. Napolitano is a fellow of the American College of Foot and Ankle Surgeons and a diplomate of the American Board of Foot and Ankle Surgery and American Board of Wound Management. He holds clinical privileges at numerous area hospitals, surgery centers, and wound care centers. He is an Adjunct Clinical Assistant Professor in the Department of Specialty Medicine at Ohio University Heritage College of Osteopathic Medicine. He is also part of the clinical faculty for the Grant Medical Center Podiatric Medicine and Surgery Program. Dr. Napolitano was one of the physician founders that helped establish the Licking Memorial Hospital Wound Care Clinic over 15 years ago. Current consulting affiliations include 3M + KCI, Organogenesis, Ortho Dermatologics and Flower Orthopedics. He remains active publishing and lecturing locally and nationally on wound care and healing. In 2018, Dr. Napolitano was the only podiatrist in the world to have an article accepted into the Cureus Journal of Medical Science’s publishing competition on negative pressure wound therapy with instillation and dwell utilizing novel dressings. In 2019, during a limited commercial release, he was the first clinician in North America to trial DERMATAC™, a new single-use, proprietary silicone-acrylic hybrid drape that is used as an accessory to NPWT systems. Dr. Napolitano is a paid consultant for Solventum.
Napolitano_Current-Dialogues-in-Wound-Management_2025_Article-1
INTRODUCTION
Negative pressure wound therapy (NPWT) has been used to treat wounds since ancient times. First known as “cupping,” this technique was described in the Ebers Papyrus around 1500 BC. It was used to treat wounds by creating suction with glass cups, heated copper bowls, or animal horns.1 Over many decades, NPWT has undergone numerous refinements. Argenta and Morykwas pioneered the use of open pore polyurethane dressings coupled with sub atmospheric pressure at -125 mmHg below ambient pressure, which forms the basis of today’s contemporary NPWT devices.2 Modern NPWT, now in its third decade of use, has been an integral part of wound management across the care continuum and continues to evolve. NPWT with instillation and dwell (3M™ Veraflo™ Therapy) is one example of such an advancement. This iteration has been commercially available for over 10 years and allows for the instillation of various fluids into the wound bed to aid in wound cleansing and removal of infectious materials.3 Fluid instillation is allowed to dwell in the wound bed to help dilute and solubilize infectious material. This step is then followed by a negative pressure cycle to remove the solubilized debris, exudate, and infectious materials. The following case demonstrates this specific technique.
CASE STUDY
An 83-year-old male, living alone and independently, presented to the hospital wound clinic for specialty care. Less than a week prior, he stated to his family that “I fell into a bar stool at home.” Upon further exploration, the family felt that he fell asleep in his power recliner resulting in his right leg being lodged in the hinge portion of the footrest. Initial presentation as related by the patient and family included a hematoma on the medial portion
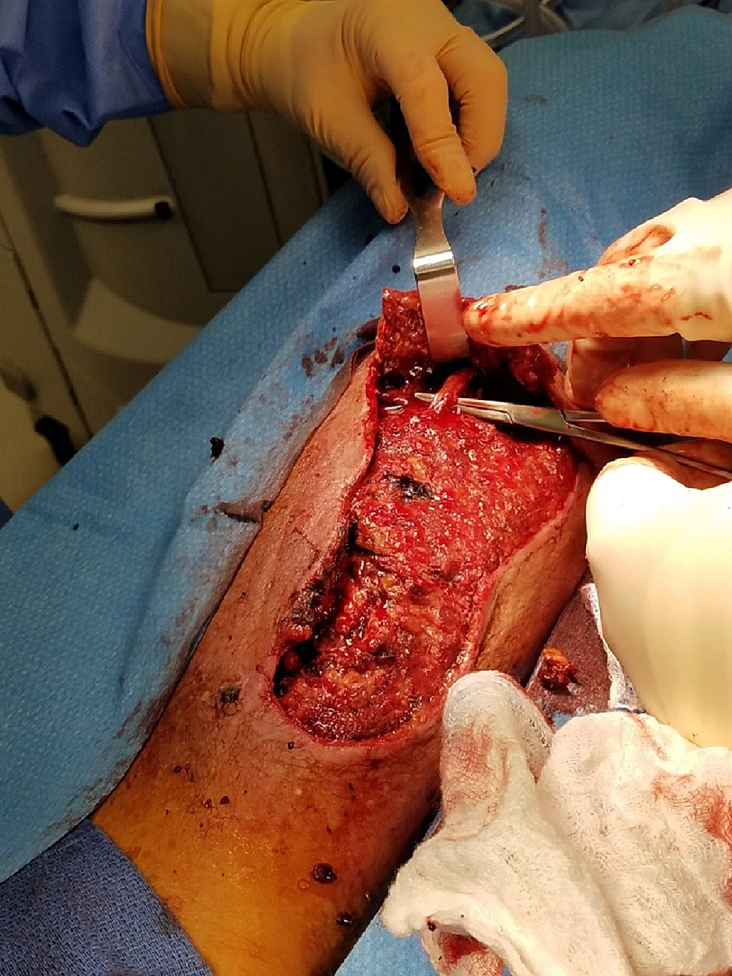
of the right calf, a tingling sensation in the right leg and foot, and some weakness of the involved extremity. Watchful waiting was employed by the patient and family. Over the next 24-48 hours, the patient and family reported that the hematoma increased in size and severity resulting in significant wound involvement and tissue necrosis (Figure 1). This increase in the severity of symptoms prompted their second visit to the wound clinic.The initial exam revealed extensive soft tissue damage with muscle necrosis and old gelatinous hematoma involvement. The neurologic exam demonstrated intact deep tendon reflexes, no sensation loss, but some mild subjective parasthesias. Vascular and orthopedic exams showed no gross deformity, an adequate range of motion with some guarding, and intact peripheral pulses with spongy edema. The patient was promptly admitted to the hospital for an appropriate medical workup in preparation for surgical debridement. Plain x-rays failed to reveal any fractures, and the full-body exam was without remark. Surgery included evacuation of the residual hematoma, extensive surgical debridement of necrotic tissues including muscle, mechanical cleansing with pulsed lavage, and deep tissue cultures (Figure 2).Once the surgery was completed, Veraflo Therapy was initiated in the operating room. 3M™ Veraflo Cleanse Choice™ Dressing was utilized. Veraflo Therapy was initiated by instilling 30 mL normal saline into the wound bed with an 8-minute dwell, followed by 3.5 hours of continuous -125 mmHg negative pressure. The patient received this therapy during his hospital stay of 6 days. An interval dressing change was performed after 48 hours of therapy. At dressing change, significant granulation tissue development was observed in the wound bed (Figure 3). Surgical wound cultures were negative other than skin flora. Initial parenteral antibiotics were changed to oral antibiotics before hospital discharge. After six days of Veraflo Therapy using Veraflo Cleanse Choice Dressing, the patient was transferred to a skilled nursing facility and he continued to receive traditional 3M™ V.A.C.® Therapy. The pressure was maintained at continuous -125 mmHg with dressing changes performed every 48-72 hours. Overall improvement in wound size and disposition was noted over the next month of care (Figure 4). Leg parasthesias improved gradually and completely resolved within the first postoperative month. Limb pain resolved within this time period as well. Approximately 6 weeks after surgery, the wound bed was noted to be entirely granular with no depth. V.A.C.® Therapy was discontinued and the patient was offered a traditional split-thickness skin graft or automated epidermal harvesting and grafting using the 3M™ Cellutome™ Epidermal Harvesting System. Risks and benefits of both techniques were discussed with the patient. He opted for the minimally invasive automated epidermal harvesting technique (Figure 5). At the 6-month follow-up, his wound had healed uneventfully with no sequalae (Figure 6).
CONCLUSION
This case highlights the successful use of the Veraflo Therapy with Veraflo Cleanse Choice Dressing along with V.A.C.® Therapy and the Cellutome Epidermal Harvesting System to achieve wound healing. While Veraflo Therapy was once thought of as a technique of last resort, it is now considered as a first-line treatment for limb preservation. When given the opportunity, clinicians should consider this powerful and cost-effective technique.4





References
- Shiffman, M.A. (2017). History of Negative-Pressure Wound Therapy (NPWT). In: Shiffman, M., Low, M. (eds) Pressure Injury, Diabetes and Negative Pressure Wound Therapy. Recent Clinical Techniques, Results, and Research in Wounds, vol 3. Springer, Cham. https://doi.org/10.1007/15695_2017_50
- Orgill DP, Bayer LR: Negative pressure wound therapy: past, present and future. Int Wound J. 2013;10 Suppl 1(Suppl 1):15-19. doi:10.1111/iwj.12170
- Kim PJ, Attinger CE, Constantine T, Crist BD, Faust E, Hirche CR, et al. Negative pressure wound therapy with instillation: International consensus guidelines update. Int Wound J. 2020;17(1):174-186. doi: 10.1111/iwj.13254
- Diehm YF, Loew J, Will PA, Fischer S, Hundeshagen G, Ziegler B, et al. Negative pressure wound therapy with instillation and dwell time (NPWTi-d) with V. A. C. VeraFlo in traumatic, surgical, and chronic wounds-A helpful tool for decontamination and to prepare successful reconstruction. Int Wound J. 2020;17(6):1740-1749. doi: 10.1111/iwj.13462

