
Professional Affairs, Global Medical Sciences, Acelity

Senior Manager, Biostatistics and Outcomes Research, Acelity

Medical Writer, Global Medical Sciences, Acelity
Grothues, Griffin, Carrizales and Martinez_Current Dialogues in Wound Management_2017_Volume 3_Issue 2
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
INTRODUCTION
Rising healthcare costs are shifting healthcare to a value-based care system, which will focus on improved patient care and outcomes while minimizing overall costs. Patient therapy in the home can bring uncertainty not only to patients and their physicians, but also to healthcare providers and payors. The World Health Organization has estimated that 50% of those living with chronic illness are non-adherent to their prescribed therapy.1 When patients are non-adherent to therapy, it can lead to unnecessary spending for excessive hospital readmissions and unnecessary emergency room visits.
Adherence to therapy in the home is a critical success factor in a patient’s care plan. Patient non-adherence leads to costly setbacks as analysis of 2005 Medicare discharge claims found that 76% of 30-day readmissions were potentially preventable.2 A 350-patient feasibility study even showed that patients with an open wound are found to be more than two times as likely to be readmitted and wound complications were the most common reason for the readmission.3 Hospitalizations are a major cost driver of chronic wounds, and it is imperative for health care providers to reduce costs by providing better management of patients with chronic conditions.
Recently, a proprietary remote therapy monitoring (RTM) system, iOn PROGRESS™ Remote Therapy Monitoring, has been developed for use with a negative pressure wound therapy (NPWT) unit for use on patients with wounds in the outpatient setting. To collect feedback on this new RTM system, a user evaluation was conducted to examine if RTM can provide information on patient NPWT adherence.
METHODS
iOn PROGRESS™ Remote Therapy Monitoring was used to monitor patient adherence beyond the hospital setting (Figure 1A). The RTM gathered therapy usage data (example data shown in Figure 1B), which was transmitted to a clinical care network. The team monitored patient therapy daily and contacted each patient when he or she fell below a therapy compliance threshold. Twenty-three patients were evaluated for all or part of length of therapy, and therapy usage was transmitted periodically. Non-adherent patients were defined as not receiving therapy for 16 hours in a day and were contacted by phone to discuss therapy usage. Patients and clinicians were asked to fill out a survey following the user evaluation to assess their perceived value of RTM.
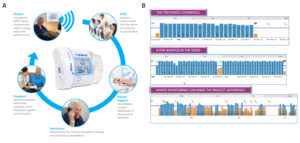 Figure 1: Remote Therapy Monitoring Continuum. A. Continuous At-Home Monitoring; B. Example output of RTM
Figure 1: Remote Therapy Monitoring Continuum. A. Continuous At-Home Monitoring; B. Example output of RTM
RESULTS
When non-adherent patients were successfully contacted, patients became adherent 81% of the time on the following day (Figure 2). Nineteen out of 22 patients (86%) maintained an average therapy use of 16 hours or more during the 30-day monitoring period. One patient was not included due to discontinuation of therapy before 24 hours.
Of 12 patient surveys received, 12/12 patients (100%) reported that they would want RTM if they needed NPWT again (Figure 3); 9/12 patients (75%) indicated that RTM provided peace of mind with their healing.Of 7 clinician surveys received, 7/7 clinicians (100%) agreed that earlier interaction through RTM may impact wound progression for patients who do not adhere to therapy usage (Figure 4).
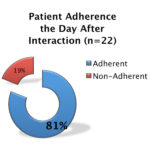 Figure 2: Patient adherence after interaction
Figure 2: Patient adherence after interaction
DISCUSSION
This user evaluation was the first to examine features of iOn PROGRESS™ Remote Therapy Monitoring. Preliminary findings revealed increased adherence for non-adherent patients who were contacted, a high rate of satisfaction for patients and clinicians, and confidence in providing care remotely. Clinicians surveyed in this user evaluation believed that iOn PROGRESS™ Remote Therapy Monitoring may help improve patient outcomes thus potentially reducing overall healthcare costs for the patient, provider, and payors. The overall goal of iOn PROGRESS™ Remote Therapy Monitoring was to change patient behavior through proactive engagement, reduce length of stay, and reduce readmissions and emergency room visits. While interactions were observed in our cohort, previous studies have evaluated RTM on patients with chronic diseases in the outpatient setting.
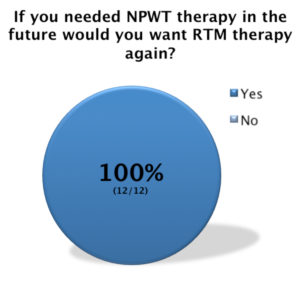 Figure 3: Patient reported value from RTM
Figure 3: Patient reported value from RTM
In a study by Broderick and Steinmetz, RTM combined with a 24/7 telehealth clinical call center demonstrated successful outcomes for patients with chronic disease such as congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), hypertension, and diabetes.4 This was evidenced by improved patient satisfaction, improved patient self-management skills, decreased use of hospital resources, and improved access to care for patients with limited mobility or transportation.5 In a randomized study of 200 COPD and CHF patients conducted by Snell, telehealth reduced rebound patients up to 70% in avoidable hospital readmissions.5 The study also showed an increased level of patient engagement for those in the telehealth group when compared to the control group, suggesting that there is potential for long-term improvements in health and the cost of care.
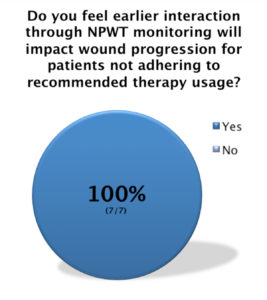 Figure 4: Clinician reported value from RTM
Figure 4: Clinician reported value from RTM
Previous studies, including the results of our clinical experience using RTM were promising. Although our sample size was low, our findings provide additional evidence for the use of telehealth in patient adherence to therapy. Larger patient populations evaluating the cost-effectiveness of RTM with NPWT are needed to support these early positive results. As such, iOn PROGRESS™ Remote Therapy Monitoring has the potential to change patient behavior through patient engagement, to increase data for healthcare providers, and to serve as a significant milestone in the value based care system.
References
1.Chisholm-Burns MA, Spivey CA. The ‘cost’ of medication non-adherence: Consequences we cannot afford to accept. J Am Pharm Assoc. 2012;52(6):8236. Cited by: Hurlow J, Hensley L. Achieving patient adherence in the wound care clinic. Today’s Wound Clinic. 2015;9(9):14-32.
2. MedPAC. Report to the Congress Promoting Greater Efficiency in Medicare Pay: Payment Policy for Inpatient Readmissions, Chapter 5. 2007:103-120.
3.Remote Patient Monitoring. Center for Connected Health Policy. Available at: http://cchpca.org/remote-patient-monitoring. Accessed July 20, 2016.
4.Broderick A, Steinmetz V. Centura health at home: home telehealth as the standard of care. The Commonwealth Fund 2013;1655(2):1-11.
5.Snell, A. The role of remote care management in population health. Health Affairs Blog. http://healthaffairs.org/blog/2014/04/04/the-role-of-remote-care-management-in-population-health. Published April 4, 2014. Accessed April 10, 2017.

