Jeffrey Litt, DO, is an Assistant Professor of Surgery and Medical Director of the Burn and Wound Programat University Hospital’s Frank L. Mitchell Jr., MD, Trauma Center. He joined MU’s Hugh E. Stephenson Jr., MD,Department of Surgery in July 2014. Born in Iowa but raised in Philadelphia, Dr. Litt completedundergraduate and medical school in Pennsylvania. He and his wife have two children.
Litt_Current Dialogues in Wound Management_2017_Volume 3_Issue 2
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
Sir William Osler once wrote, “The good physician treats the disease; the great physician treats the patient who has the disease”2. This is no less true of a competent wound care practitioner than a “Father of Modern Medicine”.
Chronic wounds are sometimes described as a “silent epidemic” in the American Health System. Often accompanied by co-morbid conditions, they pose a major threat to public health and are a major financial burden on the United States economy.3 In 2009, it was estimated that 6.5 million patients developed chronic wounds in the United States, with an estimated cost of treatment exceeding $25 billion dollars3. This care is increasingly complex and has led to the development of wound care specialist physicians, nurses, and other allied health professionals who, through experience, judicious use of technology and medical care, and clinical acumen attempt to change the disordered and altered wound bed to enable healing. Unfortunately, in spite of sometimes heroic efforts, some wounds may still remain unhealed. When this happens, it often helps to evaluate more than just the wound and its wound bed/surrounding tissues, but also evaluate the entire patient in a “holistic” sense.
Holistic wound care, or, more appropriately perhaps, holistic care of patients with wounds (acute or chronic) demands a systematic and logical assessment of the patient AND their wound. Understanding the patient in their living conditions, understanding their medical co-morbidities, their nutrition, sleep patterns, level of activity, even their psychosocial/family interactions helps wound care clinicians and specialists develop a comprehensive and more effective wound care plan.
Numerous factors affect wound healing, often divided into intrinsic, extrinsic, and iatrogenic factors. Sometimes these causes overlap but are best organized separately for a deeper and more complete understanding of everything that can lead to chronic wound conditions. Intrinsic factors can include patient age, medical co-morbidities and chronic conditions, all of which potentially have effects on tissue perfusion, oxygenation, and immune status and function. Wound age and size are also intrinsic to the patient and their wound history. Extrinsic factors include medications the patient takes, their nutritional status, any history of localized irradiation or systemic chemotherapy, or current cancer diagnosis, and patient habits, such as tobacco, alcohol, or recreational drug usage. Current psychologic or environmental stressors, including sleep patterns are of importance as well. Additionally, iatrogenic elements- including the wound age and size, as well as the current care treatment regimen- affect the environment of the wound and its subsequent healing potential.
Aging, the presence of chronic disease, and wound development often go together, as aging delays both localized and systemic repair processes, delaying cellular response to injury, impairing collagen and tissue deposition, and reducing the strength of the repaired tissues4. This occurs both locally in the open wound as well as systemically in the microcirculatory system. Increasing age, therefore, is often thought of as a marker for the development of wounds and their subsequent delayed healing. Research, however, has shown that healthy older adults without chronic diseases experience only a slight delay in wound healing compared to younger, healthy adults4. Only in the elderly population of adults, those older than 85 years old, do we see an absolute increased risk of skin breakdown4. In one study, patients 85 or older had an approximate 30% risk of developing pressure ulcers.
Chronic disease conditions, such as diabetes mellitus, peripheral vascular disease, malnutrition, spinal cord injury, and cancer, amongst others, all can lead to chronic wound development and are all critical to diagnose. These differing disease states affect wound healing in varied ways, but all have a negative impact, whether by reducing tissue perfusion, decreasing immune healing response, increasing likelihood of wound development through reduced sensation, or decreasing the ability of the body to fight infection. It should also be noted that the presence of wounds, may lead to stress in the patient. Anatomically and physiologically, there is a close interaction between the endocrine, nervous, and immune systems, studies of which comprise the field of psychoneuroimmunology. This nascent field ties together some of these processes by seeking to understand mind and body interactions, stress-related illness, and, of course, wound healing. For instance, it’s well known that stress, fear, pain, or depression can cause the release of “stress hormones” through the pituitary-adrenal axis. Cortisol is released, along with norepinephrine, causing further release of pro-inflammatory cytokines. In the susceptible patient, these inflammatory mediators suppress neutrophil migration and de-margination and inhibit release of Interleukins-1 and 6, which can impair metal metalloprotease enzymes, ultimately decreasing fibroblast proliferation and impairing wound healing4. These processes are only magnified in the chronically ill patient already prone to developing a chronic wound.
Evaluating the patient with a chronic wound involves evaluating the wound first. Assessing the wound attributes and the condition of the surrounding skin may give numerous clues to its etiology. Wound location may also help determine etiology, for instance cutaneous ulcerations due to arterial insufficiency are frequently located on the phalangeal heads or the lateral malleolus of the ankle. However, diagnosing the root cause(s) of the wound, which may be multifactorial, often involves further global patient evaluation and may include evaluating blood work to determine glycemic control, nutritional status, or presence of severe inflammatory markers, radiographic studies to assess arterial or venous insufficiency or presence of underlying bony involvement of infection, and possibly cushion or mattress pressure evaluation or mapping to determine offloading needs on areas of bony prominences. Inquiring as to the patient’s cardiopulmonary status, and directing efforts at maximizing that status could likewise be helpful. For instance, patients in decompensated heart failure, are unable to deliver oxygen and nutrients to distal areas of the body. Patients with primary or acquired lung conditions like obstructive pulmonary conditions, or even untreated sleep apnea are occasionally unable to oxygenate their tissues due to their reduced ability to oxygenate hemoglobin. Identifying and treating these conditions can frequently contribute to faster wound healing. In summary, wound care is patient care. By identifying and treating both the root causes of issues that either lend themselves to wound development or prevent wounds from healing in the normal, orderly fashion they are meant to, as well as applying appropriate local wound care, success is much more likely.
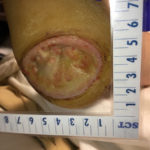
As an example, we report on the case of a 56 year old male with neuropathic foot ulcers. The patient’s past history is significant for morbid obesity with a body-mass index measurement of 45, neuropathy, likely secondary to multiple back surgical instrumentation attempts for severe spinal stenoses, and hypertension. On initial exam, the patient was noted to have bilateral plantar ulcerations on bilateral heels and first toe pads, heel wounds measuring 5 x 7 x 0.8 cm on the right, and 2 x 3.5 x 0.5 cm on the left. The toe wounds were both significantly smaller (see Fig 1, 2, and 3). Treatment ensued with a vascular
 Figure 1: Patient’s initial presentation with bilateral plantar ulcerations
Figure 1: Patient’s initial presentation with bilateral plantar ulcerations
workup, revealing no arterial or venous insufficiency. A tissue culture and biopsy were obtained in which the cultures revealed intermediate sensitive S Aureus, sensitive to Clindamycin. A biopsy showed inflammatory tissue without malignancy. At this stage, we recommended oral antibiotics and local wound care, initially with sharp debridement of hypertrophic callus and silver-based foam dressings were utilized. When the wounds failed to respond appropriately (i.e. with marked -approximate 50%- reduction in size in 4 weeks), numerous wound modalities were attempted, including negative pressure wound therapy, Total-Contact Cast (TCC) Offloading, amniotic membrane placement and repeated short courses of antibiotics. Nonetheless, the wounds failed to respond appropriately over the next 12 weeks and further global evaluation led to a diagnosis of obstructive sleep apnea, with resolution of hypopneic and apneic episodes observed at a continuous positive airway pressure (CPAP) measured at 10 mmHg.
Figures 2 and 3: Heel wounds measuring 5 x 7 x 0.8 cm on the right, and 2 x 3.5 x 0.5 cm on the left
This was initiated as home, nighttime therapy. Approximately 4 weeks later, the stalled wounds, being treated with TCC and silver-impregnated foam reduced in size by >50%. At the time of this article (7 months after initial evaluation), the left heel wound is nearly closed (2 x 2 mm) and the right wound measures 1 x 1.5 cm, with no appreciable depth (Fig 4 and 5).
Figures 4 and 5: 7 months after initial evaluation, the left heel wound is nearly closed (2 x 2 mm) and the right wound measures 1 x 1.5 cm
Until we evaluated this patient’s baseline pulmonary condition, we were completely unsuccessful in our ability to help heal his foot wounds. Once his sleep apnea was identified and treated, with little difference in wound care regimen, his wounds improved nearly to the point of full healing. In addition, with his apnea and daytime somnolence appropriately treated, the patient relates his energy level has increased markedly, leading to an ability to exercise which, in turn, has lead to weight loss, and improvement in his obesity—elements which are of clear importance in our holistic treatment plan.
In summary, wound care is patient care. Treating “the hole in the patient” without addressing the patient and their comorbidities can lead to stalled or even worsening of wounds which frustrates the patient, their family, as well as the wound care specialist. When a wound has stalled in its healing trajectory, seemingly in spite of maximal and appropriate wound care efforts, stepping back and re-evaluating “the whole patient” can lead to a better and deeper understanding of the wounded patient and their ultimate pathophysiology, potentially indicating further, previously unconsidered treatment approaches that address and treat the underlying cause of the wound.
References
1.Original Author and Source never clearly identified; Article author first encountered the saying at the American College of Surgeons Clinical Congress session, “Wound Care: Mentoring the Mentors”, Lantis, JC Course Director, 2016; Washington DC
2.Centor, RM. To Be A Great Physician You Must Understand the Whole Story. MedGenMed. 2007; 9(1): 59
3.Sen C, Gordillo G, Sashwati R, Kirsner R, Lambert L, Hunt T, Gottrup F, Gurtner G, Longaker M. Human Skin Wounds: A Major and Snowballing Threat to Public Health and the Economy. Wound Repair Regen. 2009; 17(6): 763–771
4.Sussman, C. (2012). Assessment of the Patient, Skin, and Wound. In Sussman, C., and Bates-Jensen, Barbara (Eds.), Wound Care A Collaborative Practice Manual for Health Professionals. (4th ed). P. 54 Lippincott Williams & Wilkins
5.Tatsioni, A., Balk, E, O’Donnell, T., Lau, J. Usual Care in the Management of Chronic Wounds: A Review of the Recent Literature. J Amer Coll Surg. 2007; 205(4): 617-23