
Jeffrey Litt, DO, is an Assistant Professor of Surgery and Medical Director of the Burn and Wound Program at University Hospital’s Frank L. Mitchell Jr., MD, Trauma Center. He joined the University of Missouri’s Hugh E. Stephenson Jr., MD, Department of Surgery in July 2014. Born in Iowa but raised in Philadelphia, Dr. Litt completed undergraduate and medical school in Pennsylvania. He and his wife have two children. After a burn center experience as a third-year medical student, Dr. Litt entered general surgery training determined to become a burn surgeon. He then completed two years of training in burn surgery and surgical critical care training at Vanderbilt University Medical Center in Nashville, Tennessee. Dr. Litt is board-certified in general surgery. His interests include burn care and resuscitation.
Litt_Current Dialogues in Wound Management_2018_Volume 4_Issue 2
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.Patients who experience multi-system trauma frequently have injuries to their extremities. Occasionally, some of these limb injuries can be quite dramatic, drawing the attention of the medical team to the gruesome limb injury before them. It’s important to remember in these cases that Advanced Trauma Life Support (ATLS) principles dictate identifying and treating immediate life-threatening injuries as soon as they are identified1, no matter how grisly the injured limb may seem. In many cases of patients who suffer severe extremity trauma, an amputation has essentially already occurred prior to evaluation, i.e. a severed limb held on only by skin or minimal soft tissue. In
 Figure 1: Left open femur fracture with exposed intramedullary nail
Figure 1: Left open femur fracture with exposed intramedullary nail Figure 2: Trauma Bay anteroposterior x-ray of femur injury
Figure 2: Trauma Bay anteroposterior x-ray of femur injury
those cases, completion amputation is an easy choice. In other cases, a severely injured, or “mangled” extremity requires further evaluation to determine if salvage is possible and would allow for optimal patient recovery.
A 62-year-old man was brought into the trauma resuscitation area of our Level 1 Trauma facility after a severe motorcycle accident. Initial evaluation ensued, the patient was hemodynamically normal and awake and alert during his primary and secondary evaluations. Work-up revealed multi-system trauma, including pelvic fractures, facial fractures, an open left femur and acetabular fracture with exposed hardware (Figure 1,2) from a history of a previously repaired femur
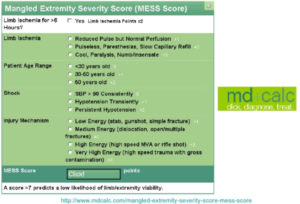 Figure 3: Mangled Extremity Score Calculator, phone application version MD+CALC
Figure 3: Mangled Extremity Score Calculator, phone application version MD+CALC
fracture, as well as an open left tibial fracture. A tourniquet, placed on scene, was in place and no further life threatening or hemorrhagic injuries were identified. When the tourniquet was taken down, a pulse with biphasic signals was identified through Doppler. The patient was brought to the operating room from the trauma bay for a femur washout and attempt at fixation. Unfortunately, on anesthetic induction the patient’s acutely decompensated, and, in a “life-or-limb” decision, the orthopedic trauma team performed a guillotine above-knee amputation. Prior to this sequence of events, discussions between the orthopedic and trauma teams resulted in the decision to attempt limb salvage. This was partially evaluating the patients “Mangled Extremity Severity Score” (MESS) quickly at the bedside.
The MESS (see Figure 3) is one of several scoring systems developed to prognosticate the potential success of limb salvage in a seriously injured extremity. Other common scoring systems include the Limb Salvage Index (LSI), the Predictive Salvage Index (PSI), and the Nerve Injury, Ischemia, Soft-Tissue Injury, Skeletal Injury, Shock, and Age of patient (NISSSA). These systems all attempt to evaluate the damaged limb in an objective way by evaluating evidence of tissue ischemia, severe neurovascular damage, patient hemodynamic condition (i.e., presence of shock), and extent of bony and soft tissue injury. In addition, patient factors such as age are frequently taken into account. Other patient factors, such as underlying comorbidities and lifestyle factors (i.e. tobacco or drug usage) are not typically part of the initial decision-tree but may ultimately impact the final outcome. Numerous studies have evaluated the accuracy of these “scores” in predicting their validity in determining “successful” limb salvage (i.e. “functional” patient recovery, with or without an amputated limb). Schiro et al conducted a systematic review of the scoring systems in 2015 and concluded that “scoring systems” alone shouldn’t be used as a sole criterion for the surgeon caring for the patient with a mangled extremity in deciding whether or not to amputate, nor were these same scoring systems accurately predictive of functional recovery in patients who underwent advanced salvage techniques
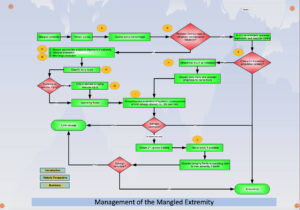 Figure 4: Western Trauma Association “Management of the Mangled Extremity” Critical Decisions in Trauma Algorithm http://www.westerntrauma.org/algorithms/WTAAlgorithms_files/svg_7.htm
Figure 4: Western Trauma Association “Management of the Mangled Extremity” Critical Decisions in Trauma Algorithm http://www.westerntrauma.org/algorithms/WTAAlgorithms_files/svg_7.htm
The Lower Extremity Assessment Project (LEAP), funded by the NIH, was a multi-institutional prospective study that evaluated long-term outcomes for adult patients who sustained “a high-energy traumatic injury below the distal femur”3. Five hundred forty-five patients, 149 of whom underwent an initial primary amputation post-injury, were followed over 2 years, and the type and number of complications were recorded at pre-determined time points up to 2 years, comparing patients who received initial amputations versus reconstructive efforts. Findings from this study include high rates of complications in all groups. The most common complication seen in all patients sustaining severe lower extremity injury was, not surprisingly, the development of wound infections. Nearly 28% (154/545) of patients experienced a clinically significant wound infection, three-quarters of whom required operative interventions3. Differentiating between the salvage vs amputation groups, nonunion was a common finding/complication (23.7%) in limb salvaged patients, usually diagnosed late in the patients’ course–6 or more months from injury3. Other complications in patients with salvaged limbs included: infection, osteomyelitis, arthritis and incapacitating nerve pain, malunion, and development of venous thromboembolism3. The primary amputation group also experienced significant complications, including: infection, stump dehiscence, and phantom limb pain/late stump complication development. Nearly 30% of these patients required re-hospitalization during the study period. Ultimately, the LEAP group investigators were in agreement with the majority of studies evaluating these patients in that those who underwent reconstructive procedures encounter a greater number of complications as well as more operative interventions than those who undergo a primary amputation3. In addition, those who undergo “late” amputations, or amputations after unsuccessful salvage attempts, had the highest complication rate in this study3, although the definition of “late amputation” was not explicitly delineated. Unfortunately, “mangled extremity” scores were not part of the evaluated data, and, like other studies, we are not left with a great deal of hard data to make the “salvageability” decision, in spite of “scores”. Other studies have evaluated this patient set and determined few long-term functional outcomes between those with amputations and those with salvaged limbs.
Therefore, the determination of “salvageability” of a limb is largely a clinical “gestalt”, with the proviso that a “score” may help in coming to that “feeling”. In our case, our initial gestalt, with a hemodynamically stable patient with minimally documented comorbidities, and a MESS of 6 (limb ischemia <6 hours, reduced pulse but intact perfusion, age > 50, no shock, and presumed high-speed injury) led us to believe that limb salvage was at least initially, a reasonable approach. Importantly, when the patient’s clinical condition changed, our overall patient evaluation and algorithm similarly changed, and the prudent, life-saving choice was an immediate amputation with a staged approach. With orthopedic assistance, vascular control was obtained, and a trans-femoral amputation was completed through the existing intra-medullary rod. A negative-pressure dressing was applied, and the patient was subsequently stabilized in the Surgical ICU. Subsequently, the patient experienced a waxing and waning course, with repeated takebacks and washouts in the operating room. Ultimately, he was able to be liberated from mechanical ventilation and was progressing for transfer out of the ICU when he experienced a respiratory event that required initiation of ultimately unsuccessful Advanced Cardiac Life Support. He died, twelve days after his initial admission. At the time of his death, his amputation site was closed after placement of antibiotic-impregnated beads in the femoral canal. An autopsy was declined by the family.
The patient with the “mangled” extremity is, ultimately, a trauma patient who requires careful, considerate trauma evaluation and stabilization per ATLS guidelines. The mangled extremity, on initial evaluation, has significant “dramatic” impact. It’s important to methodically evaluate and treat the patient with such a mangled extremity, in spite of the gruesome injury. One should also keep in mind that the force required to “mangle” an extremity is, by-and-large, sufficient to cause significant, even life-threatening multi-system injury and care for the patient with a “mangled” extremity, rather than the extremity itself is paramount. A surviving patient, even with a traumatic amputation is a better outcome than a dead patient with a “salvaged” limb if efforts to salvage the limb result in significant or insurmountable morbidity. The decision to amputate vs salvage the limb is primarily clinical. The MESS or other similar scoring systems may help in that determination, but making a determination expressly using a “score” is not recommended. Ultimately, we suspect that, as in our case, most of these decisions are made after thoughtful consideration, often in conjunction with specialists such as orthopedic or vascular surgeons. The stable patient can often tolerate attempts at salvage but the unstable patient is typically less tolerant of such lengthy and extensive operative procedures. Ultimately, an attempt at a guiding algorithm (Fig 4), formulated by the Western Trauma Association, published in 2012 by Scalea et al helps direct the practitioner in many of the challenges managing patients with severe extremity
. Multi-disciplinary care of the patient with such injuries, keeping in mind the overall patient status, often leads to optimal functional outcomes. Such expertise is most frequently encountered at verified trauma centers. Patients initially evaluated at non-trauma centers should be referred to the nearest trauma center for expeditious transfer and evaluation. Ultimately, limb salvage comes down to patient characteristics such as age and injury patterns as well as hemodynamic status. Decisions regarding limb-salvage should be carefully considered in the patient with multi-system injury in light of the patient‘s overall clinical status, and frequent communication between the trauma and specialist teams is important for optimizing overall patient outcomes.
References
1.Advanced Trauma Life Support, 9th ed. (2012). Chicago, IL; American College of Surgeons Committee on Trauma
2.Schiro, G.R., Sessa, S., Piccioli, A., Maccauro, G., Primary Amputation vs Limb Salvage in Mangled Extremity: A Systematic Review of the Current Scoring System. BMC Musculoskeletal Disorders. (2015); 16:372-78
3.Harris, A.M; et al. Complications Following Limb-Threatening Lower Extremity Trauma. J Orthop Trauma. (2009); 23:1-6
4.Scalea, T.M., et al. Western Trauma Association Critical Decisions in Trauma: Management of the Mangled Extremity. J Trauma. (2012); 72:86-93

