Dr. Fernández is a Clinical Assistant Professor of Surgery and Family Practice at the University of Texas Health Center at Tyler. He is also an Attending Teaching Staff in the Division of Surgery for Mother Frances Health System and East Texas Medical Center in Tyler. Dr. Fernandez obtained his residency training at Loyola University, the University of Illinois, the University of Chicago and Northwestern University, Chicago, Illinois, with special training in Trauma and Burns at Kings County Hospital, SUNY Down State System, Brooklyn, New York, NY. He is well published in multiple areas of research both in peer-reviewed articles and book chapters, and has made numerous oral and poster presentations at national and international conferences.
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
BACKGROUND
Most combat-related deaths occur prior to the injured soldier reaching definitive care and involve rapidly exsanguinating injuries. This is due to the devastating effect and nature of the improvised explosive devices (IEDs) used by the enemy combatant forces (Figure 1-3) 1,2.The widespread use of advanced body armor, better initial combat injury care, rapid evacuation of the wounded, and the deployment of Forward Surgical Teams (FST) have led to increased casualty survival rates (Figure 4) 3-5.
EPIDEMIOLOGY
Combat injuries are commonly high-energy transfer wounds that cause significant disruption of soft tissue and underlying osseous components, resulting in devitalized and contaminated wounds with a high risk for infection, delayed healing and limb amputation6.
Wounds are contaminated with remnants of explosive devices, bullet fragments, and clothing, as well as environmental contaminants. Blast injuries commonly cause vascular injury, leading to tissue ischemia and necrosis which contribute to coagulopathy, acute renal injury and multiple organ system failure. This causes the blast injury victim to be immunocompromised and predisposes the patient to infection7.
The high risk of nosocomial infection by resistant bacteria from other geographic regions of the world involving patients, elements of the care team, facilities throughout
 Figure 1: Ammunition rigged for an IED discovered by Iraqi police in Baghdad in November 2005.
Figure 1: Ammunition rigged for an IED discovered by Iraqi police in Baghdad in November 2005.
Source: https://en.wikipedia.org/wiki/Improvised_explosive_device
 Figure 2: Cougar Mine-Resistant Ambush Protected(MRAP) in Al Anbar, Iraq, was hit by a directed charge IED approximately 300–500 lbs. in size.
Figure 2: Cougar Mine-Resistant Ambush Protected(MRAP) in Al Anbar, Iraq, was hit by a directed charge IED approximately 300–500 lbs. in size.
Source: IraqSlogger (http://iraqslogger.powweb.com/index.php/post/4265/IED_Destroys_MRAP_But_Soldiers_Survive?PHPSESSID=b155c5eb6418ac653ca2ce675e6fb7f8), EUReferendum (http://eureferendum.blogspot.com/2007/08/imagine-this-was-snatch.html), Defense Industry Daily (http://www.defenseindustrydaily.com/cougar-armored-trucks-to-stalk-mines-on-the-battlefield-updated-0532/),Defense Department Contracts for 2,400 More MRAP Vehicles (http://www.defense.gov/news/newsarticle.aspx?id=47849)
the tier of transfer, and definitive care is well documented8-11 and includes steps such as: casualty evacuation, tactical medical evacuation by the Army forward surgical team, strategic aeromedical evacuation to a combat support hospital within 72 hours to a major U.S.-based military hospital where definitive care can be received and, ultimately, post-acute care back in the U.S.12
 Figure 3: Marine Corpsman providing treatment to a wounded Iraqi soldier, 2003.
Figure 3: Marine Corpsman providing treatment to a wounded Iraqi soldier, 2003.
Source: This Image was released by the United States Marine Corps with the ID 030402-M-3138H-006 (http://www.navy.mil/view_image.
asp?id=6574) (next) (https://commons.wikimedia.org/w/index.php?title=Category:Files_created_by_the_United_States_Marine_Corps_with_known_IDs&filefrom=030402-M-3138H-006#mw-category-media).
 Figure 4: Members of the 541st Forward Surgical Team (FST) (Airborne) perform an assessment of an Afghan man on Forward Operating Base (FOB) Farah, Afghanistan in support of Operation Enduring Freedom(OEF) on December 26, 2012.
Figure 4: Members of the 541st Forward Surgical Team (FST) (Airborne) perform an assessment of an Afghan man on Forward Operating Base (FOB) Farah, Afghanistan in support of Operation Enduring Freedom(OEF) on December 26, 2012.
Source: https://www.dvidshub.net/image/806979/medicalcasualty-treatment-fob-farah High-resolution image (https://www.dvidshub.net/download/image/806979)
The Joint Theater Trauma Registry for the United States Army Institute for Surgical and Battlefield Research was queried for United States service members receiving treatment for wounds sustained during Operation Iraqi Freedom and Operation Enduring Freedom. The main distribution of combat wounds was: extremities (49.4-55%), head and neck (30-36.2%), thorax (10%), and abdomen (10%). Almost 75% resulted from explosive mechanisms; just 20% were gunshot wounds. The distribution of these wounds was as follows: head/neck 36.2%, thorax 7.5%, abdomen 6.9%, and extremities 49.4% (Figure 6)13-16.
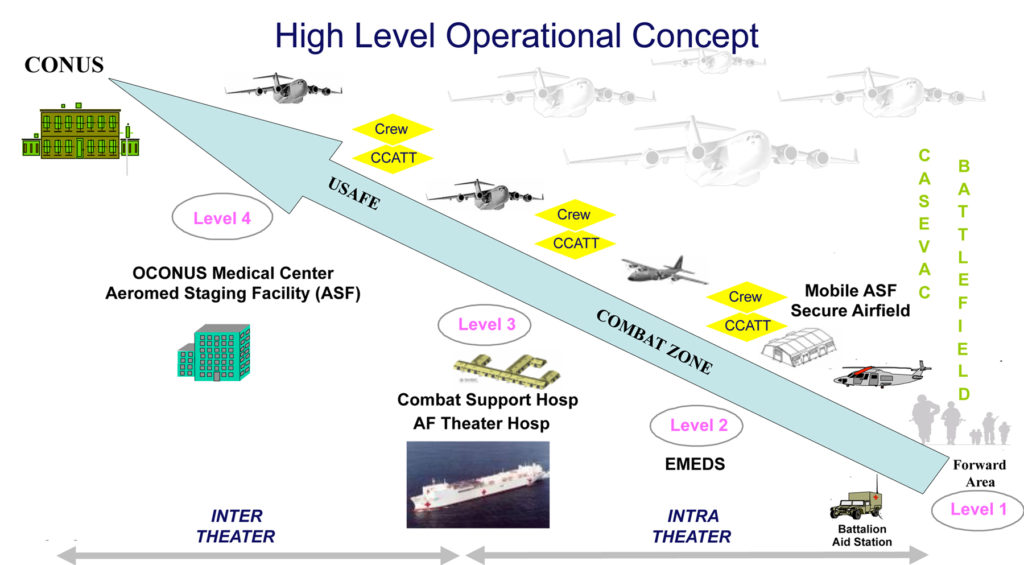 Figure 5: Military Medical Transfer Tiers: CCATT = Critical Care Air Transport Team; USAFE= U.S. Air Forces in Europe;CONUS=Contiguous United States; OCONUS= Outside Contiguous United States; EMEDS= Expeditionary Medical Support System.
Figure 5: Military Medical Transfer Tiers: CCATT = Critical Care Air Transport Team; USAFE= U.S. Air Forces in Europe;CONUS=Contiguous United States; OCONUS= Outside Contiguous United States; EMEDS= Expeditionary Medical Support System.
Source: Lt Col Patricio G. Bruno, Do, FAAFP, FHM. http://amops.org/wp-content/uploads/2015/04/CCATT-by-Patricio-Bruno-DO.pdf
THERAPEUTIC INTERVENTIONS: THE ROLE OF NEGATIVE PRESSURE WOUND THERAPY
Debridement, irrigation, and closure by secondary intention are fundamental principles for the management of combat injuries. These often require multiple operations across all levels of care. Damage control surgical principles have contributed to decreased bleeding, and an increase in limb preservation, and overall survival
 Figure 6: Example of secondary blast injuries to both legs.
Figure 6: Example of secondary blast injuries to both legs.
Source: : O’Brien PJ, Cox MW. J Surg Radiol. 2011; 2(1):1-112, 155
Negative Pressure Wound Therapy (NPWT) has been a helpful adjunct in the management of these devastating wounds. The benefits of NPWT in the civilian experience have been well documented and are the basis for its initial use in the care of combat wounds (Figure 7)19-25.
MODES OF DELIVERY OF NEGATIVE PRESSURE WOUND THERAPY AND THEIR EFFECTS
The Vacuum-Assisted Closure FREEDOM™ Therapy System (V.A.C. FREEDOM™ Therapy System) (first used in 2004) was tested and validated according to the Joint Airworthiness Certification Test Protocol for interoperability and functionality at cabin pressures typical of Critical Care Air Transport Teams/MEDEVAC flights (Figure 8)26,27.
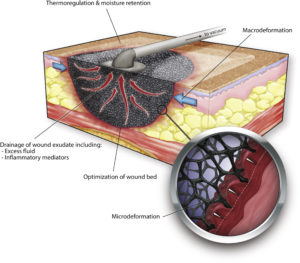 Figure 7: Huang C, Leavitt T, Bayer LR, Orgill DP. Effect of negative pressure wound therapy on wound healing.
Figure 7: Huang C, Leavitt T, Bayer LR, Orgill DP. Effect of negative pressure wound therapy on wound healing.
Curr Probl Surg. 2014; 51(7): 301-331.
Reports of the efficacy and utility of NPWT in the treatment of soft tissue combat injuries show that this adjunctive modality has been effective in improving wound healing and overall patient outcome28,29.Negative Pressure Wound Therapy with instillation and dwell time (NPWTi-d, V.A.C. VERAFLO™ Therapy) provides intermittent delivery of a timed, predetermined volume of topical wound solution, which is allowed to dwell in the wound bed for a user-selected time period prior to resuming NPWT30. The use of NPWTi-d for soft tissue wounds has become more common in the civilian patient population. NPWTi-d has been reported to reduce length of hospital stay, trips to OR, and may be used to prepare the wound to enhance granulation tissue formation in a variety of wound types between operative debridements when compared to standard NPWT. (Figure 9-10) 31-35. It is this author’s opinion that NPWTi-d may be an innovative and effective form of therapy for the management of all forms of complex soft tissue, including combat related injuries. Further studies are necessary to evaluate the effectiveness for combat wounds
 Figure 8: V.A.C. FREEDOM™ Therapy System, a NPWT device with, long battery life (~12 hours) and lightweight design that enables patients to be mobile and active.
Figure 8: V.A.C. FREEDOM™ Therapy System, a NPWT device with, long battery life (~12 hours) and lightweight design that enables patients to be mobile and active.
Source: Kinetic Concepts, Inc.
 Figure 9: V.A.C. VERAFLO™ Therapy as applied by V.A.C.ULTA™ Therapy Unit.
Figure 9: V.A.C. VERAFLO™ Therapy as applied by V.A.C.ULTA™ Therapy Unit.
Source: Kinetic Concepts, Inc.
CONCLUSIONS:
The principles of early debridement, irrigation, fracture stabilization, and delayed closure of wounds remain the cornerstone of care for those injured in combat and civilian casualty care. NPWT is one of a number of techniques for managing military high-energy injuries. The published literature suggests that conventional military wound management doctrine may be improved with the NPWT, resulting in early, more reliable primary closure of wartime injuries; and, this may be further enhanced with the application of NPWTi-d in appropriately selected cases.
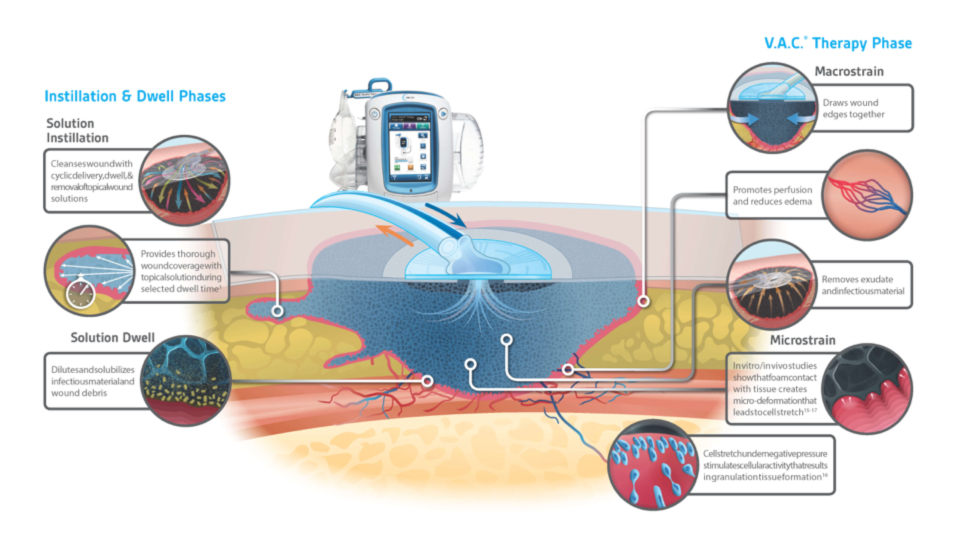 Figure 10: V.A.C. VERAFLO™ Therapy combines the benefits of V.A.C.® Therapy with automated topical wound solution distribution and removal.
Figure 10: V.A.C. VERAFLO™ Therapy combines the benefits of V.A.C.® Therapy with automated topical wound solution distribution and removal.
Source: Kinetic Concepts, Inc. Rycerz AM, et al. Int Wound J 2013;10:-214-220. Sazena SM, et al. Plast Recon Surg 2004;114(5):1086-1095. McNulty AK, et al.Wound Repair Regen 2009 Mar; 17(3):192-199. McNulty AK et al. Wound Repair Regen 2007;15:838-846.
References
1.Sebesta, James. “Special lessons learned from Iraq.” Surgical Clinics 86.3 (2006): 711-726.
2.Lewis, N. Tactical Combat Casualty Care Manual, Ed 1. Washington, DC, U.S.
3.Thorson, Chad M., et al. “Military trauma training at civilian centers: a decade of advancements.” Journal of Trauma and Acute Care Surgery 73.6 (2012): S483-S489.
4.Eastridge, Brian J., et al. “Forward Surgical Teams provide comparable outcomes to combat support hospitals during support and stabilization operations on the battlefield.” Journal of Trauma and Acute Care Surgery 66.4 (2009): S48-S50.
5.Shen-Gunther, Jane, et al. “Operation Enduring Freedom: trends in combat casualty care by forward surgical teams deployed to Afghanistan.” Military medicine 176.1 (2011): 67-78.
6.Gawande, Atul. “Casualties of war—military care for the wounded from Iraq and Afghanistan.” New England Journal of Medicine 351.24 (2004): 2471-2475.
7.Heath, Christopher H., et al. “A review of the Royal Perth Hospital Bali experience: an infection control perspective.” Healthcare Infection 8.2 (2003): 43-54.
8.Sharpnack, Douglas D., et al. “The pathology of primary blast injury.” Conventional Warfare: Ballistic, Blast, and Burn Injuries: Department of the Army, Office of the Surgeon General (1991): 271-294.
9.Petersen, Kyle, et al. “Trauma-related infections in battlefield casualties from Iraq.” Annals of surgery 245.5 (2007): 803.
10.Schrager, Jason J., et al. “Lessons from the tip of the spear: medical advancements from Iraq and Afghanistan.” Respiratory care 57.8 (2012): 1305-1313.
11.Bailey, J., et al. “Joint Trauma System: Development, Conceptual Framework, and Optimal Elements, US Department of Defense.” US Army Institute for Surgical Research 51 (2012).
12.National Academies of Sciences, Engineering, and Medicine. 2016. A national trauma care system: Integrating military and civilian trauma systems to achieve zero preventable deaths after injury. Washington, DC: The National Academies Press. doi: 10.17226/23511.
13.Owens, Brett D., et al. “Combat wounds in operation Iraqi Freedom and operation Enduring Freedom.” Journal of Trauma and Acute Care Surgery 64.2 (2008): 295-299.
14.Owens, Brett D., et al. “Characterization of extremity wounds in operation Iraqi freedom and operation enduring freedom.” Journal of orthopaedic trauma 21.4 (2007): 254-257.
15.Belmont, P. J., et al. “Epidemiology of combat wounds in Operation Iraqi Freedom and Operation Enduring Freedom: orthopaedic burden of disease.” J Surg Orthop Adv 19.1 (2010): 2-7.
16.Belmont, P.J., et al. “Combat Wounds in Iraq and Afghanistan from 2005 to 2009.” J trauma acute care surg 73.1 (2012):3-12.
17.Rotondo, Michael F., et al. “’Damage control’: an approach for improved survival in exsanguinating penetrating abdominal injury.” The Journal of trauma 35.3 (1993): 375-82.
18.Murray, Clinton K., et al. “Prevention and management of infections associated with combat-related extremity injuries.” Journal of Trauma and Acute Care Surgery 64.3 (2008): S239-S251.
19.Argenta, L. C., and M. J. Morykwas. “Vacuum-assisted closure: a new method for wound control and treatment: clinical experience.” (1997): 563-577.
20.DeFranzo, A. J., et al. “The use of vacuum-assisted closure therapy for the treatment of lower-extremity wounds with exposed bone.” Plastic and reconstructive surgery 108.5 (2001): 1184-1191.
21.Herscovici, Dolfi, et al. “Vacuum-assisted wound closure (VAC therapy) for the management of patients with high-energy soft tissue injuries.” Journal of orthopaedic trauma 17.10 (2003): 683-688.
22.Huang, Chenyu, et al. “Effect of negative pressure wound therapy on wound healing.” Current problems in surgery 51.7 (2014): 301-331.
23.Chen, Kuang-Den, et al. “Mechanotransduction in response to shear stress roles of receptor tyrosine kinases, integrins, and Shc.” Journal of Biological Chemistry 274.26 (1999): 18393-18400.
24.Saxena, Vishal, et al. “Vacuum-assisted closure: microdeformations of wounds and cell proliferation.” Plastic and reconstructive surgery 114.5 (2004): 1086-1096.
25.Orgill, Dennis P., et al. “The mechanisms of action of vacuum assisted closure: more to learn.” Surgery 146.1 (2009): 40-51.
26.Hinck, D., et al. “Use of vacuum-assisted closure negative pressure wound therapy in combat-related injuries—literature review.” Military medicine 175.3 (2010): 173-181.
27.Couch, K., et al. “Negative-pressure wound therapy in the military: lessons learned.” Plastic and reconstructive surgery 127 (2011): 117S-130S.
28.Geiger, Scott, et al. “War wounds: lessons learned from Operation Iraqi Freedom.” Plastic and reconstructive surgery 122.1 (2008): 146-153.
29.Leininger, Brian E., et al. “Experience with wound VAC and delayed primary closure of contaminated soft tissue injuries in Iraq.” Journal of Trauma and Acute Care Surgery 61.5 (2006): 1207-1211.
30.Wolvos, T. A. “Negative pressure wound therapy with instillation: the current state of the art.” Surgical technology international 24 (2014): 53-62.
31. Back, David A., et al. “Recommendations on negative pressure wound therapy with instillation and antimicrobial solutions–when, where and how to use: what does the evidence show?” International wound journal 10.s1 (2013): 32-42.
32.Gabriel, Allen, et al. “Use of negative pressure wound therapy with automated, volumetric instillation for the treatment of extremity and trunk wounds: clinical outcomes and potential cost-effectiveness.” Eplasty 14 (2014).
33.Kim, Paul J., et al. “The impact of negative-pressure wound therapy with instillation compared with standard negative-pressure wound therapy: a retrospective, historical, cohort, controlled study.” Plastic and reconstructive surgery 133.3 (2014): 709-716.
34.Lessing, Chris, et al. “Negative pressure wound therapy with controlled saline instillation (NPWTi): dressing properties and granulation response in vivo.” Wounds 23.10 (2011): 309.
35.Lessing, M. Christian, Roberta B. James, and Shannon C. Ingram. “Comparison of the effects of different negative pressure wound therapy modes—continuous, noncontinuous, and with instillation—on porcine excisional wounds.” Eplasty 13 (2013).

