Cathy is an Advanced Practice WOC Nurse providing care to patients across the continuum in acute care, long-term care, home health and outpatient settings. Employed by Connecticut Clinical Nursing Associates, she also provides consulting to organizations wishing to improve wound outcomes, conducts clinical research, lectures nationally and internationally, is the Co-Editor of the text Wound, Ostomy, Continence Secrets and provides clinical support to Wound Reference.com. She currently serves as the Co-chair of the Post-Acute Care Symposium. Additionally, she serves as a Nurse Board Member of the Association for the Advancement of Wound Care and an Associate Clinical Professor at the Yale School of Nursing.
Milne_Current Dialogues in Wound Management_2019_Volume 5_Issue 2
INTRODUCTION
It goes without saying that chronic wounds take a large toll on individuals and incur substantial costs to societies worldwide. These wounds are subject to infection, which leads to a cycle of inflammation and tissue damage that further supports microbial growth and undercuts the ability to heal.
Treating infected wounds early and appropriately reduces these burdens and should be a priority of all health providers involved in wound care. At the same time, overuse of antibiotics can result in the development of antibiotic-resistant organisms and may contribute to increased disease complications and healthcare costs. It is paramount to use antibiotics with restraint and seek other treatment strategies.
THE SILVER SOLUTION
Antimicrobial silver dressings are a well-established approach to managing wound infections—but not all silver dressings are created equal. The formulation of silver has a bearing on clinical activity, and health providers must understand the distinctions between products to ensure make the most appropriate selection.
In its natural state, silver does not have antimicrobial activity. The soluble ion (Ag+) is required to draw electrons from bacterial cells and thus halt their proliferation. Ag OXYSALTS™ Technology (silver oxynitrate) is the only compound used in dressings that releases Ag1+, Ag2+ and Ag3+ ions. Of these, Ag2+and Ag3+ exert a stronger pull on the electrons within microbial cells and have a greater ability to stop the metabolic processes within these cells.
Solubility also influences the clinical action of silver salts: the greater the solubility, the faster the antimicrobial action. Some compounds, such as silver chloride, are virtually insoluble. Others, including Ag OXYSALTS™ Technology, are highly soluble in fluid, where they can quickly release Ag ions to exert their beneficial effects.1Taken together, the unique properties of Ag OXYSALTS™ Technology result in sustained, broad-spectrum antimicrobial activity.1 Even when infection is not present, Ag OXYSALTS™ Technology promote healing by generating oxygen, which provides the energy for effective wound repair.
RESEARCH QUESTION
In unblinded case reports, use of fibrous silver oxysalt dressings (FSOD) has been associated with decreased bioburden, as measured by bioburden assessment scores and reductions in wound surface area.2,3The effect of these dressings on wound-related inflammation, however, has not been established.
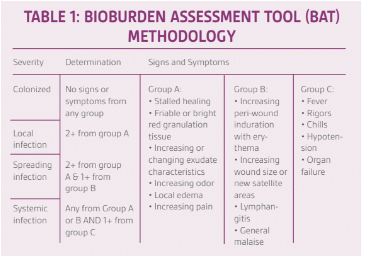
To determine whether FSODs have the capacity to reduce inflammation as well as bioburden, several nurses participated in an evaluation using wound thermography along with a standard bioburden assessment tool (BAT) (Table 1).
METHODS
At baseline and at the end of the two-week treatment period, ten certified nurses evaluated wounds of different etiologies in 9 different patients through standard wound photographs and the BAT to assess bioburden. Infrared thermography photos of the wounds were used concurrently to assess wound-bed and peri-wound inflammation. All wounds were treated with a FSOD over a two-week period. Participants were not aware of the treatment protocol. The number of dressing changes varied depending on wound drainage.
WHY INFRARED THERMOGRAPHY?
It is known that infected wounds have a higher temperature. In chronic wounds, increased local temperature is one of the classic signs of wound infection and inflammation, and measuring the temperature may help optimize the assessment and treatment of lesions.4Interest in using infrared thermography to assess and manage wounds began several decades ago. Over the years, as the technology improved, it became possible to demonstrate that infrared thermography could measure inflammation (Figure 1).
OUTCOMES
After the two-week FSOD treatment, wounds improved significantly. Of note, the improvement in BAT scores correlated with the reduction in inflammation (as determined by visual inspection of infrared thermographs). The following two cases from the study illustrate the improvement seen after application of Ag OXYSALTS™ Technology in patients with a poor response to previous treatment.
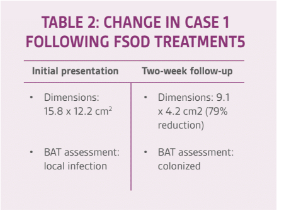
CASE 1: RESOLUTION OF AN INFECTION
An older woman presenting with venous hypertension with ulceration received standard foam dressing for two weeks with adequate compression, but her condition did not improve. The standard dressing was then substituted with an FSOD. The affected area was covered by an abdominal pad prior to reapplying compression. The dressing was changed a total of 9 times. As detailed in Table 2 and Figure 2, the wound resolved significantly following treatment.
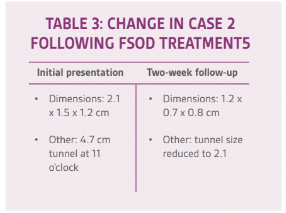
CASE 2: IMPROVED WOUND CHARACTERISTICS
A middle-aged man experienced infection at the site of a ruptured cyst. His initial treatment consisted of incision and drainage, followed by systemic antibiotics for 2 weeks and local wound care with foam dressing and topical silver alginate packing 3 times weekly for 4 weeks. When the wound didn’t heal, the patient was sent for evaluation and re-treatment. The wound, deemed to be a local unresolved infection, was packed with an FSOD and covered with a foam dressing. After 2 weeks of this new protocol, the wound dimensions and characteristics improved significantly, as summarized in Table 3 and Figure 3
IMPLICATIONS
As demonstrated in this small evaluation, Ag OXYSALTS™ Technology can improve wound outcomes by reducing inflammation and helping to manage localized infection.
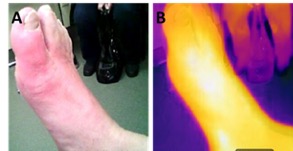 Figure 1. Example of infrared thermography. A. Image of active gout flare; B. Infrared thermography image of active gout flare. Note that the lighter the color, the more heat (inflammation) that radiates from the tissue
Figure 1. Example of infrared thermography. A. Image of active gout flare; B. Infrared thermography image of active gout flare. Note that the lighter the color, the more heat (inflammation) that radiates from the tissue
The nurses participating in this evaluation were able to assess how a variety of wounds responded to treatment with a FSOD, using wound thermography to evaluate inflammation paired with a bioburden assessment tool. When applied over a two-week period, FSODs were found to reduce bioburden as well as wound bed and peri-wound inflammation.
This study lends support to previous research showing that infrared thermography can identify infection and changes in wound inflammation.4 When paired with a bioburden assessment tool, infrared thermography can help improve wound evaluation. The technology also provides information about wound status that can help clinicians gauge wound healing and select the most appropriate management strategy.
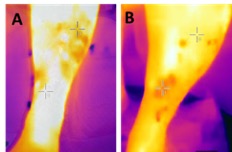 Figure 2. Venus leg ulcer infrared thermography. A.Left leg baseline, wound temperature 99.2°F, epithelialized area temperature 96.7°F; B. Left leg after 2 weeks of treatment, wound temperature 96.0°F, epithelialized area temperature 96.8°F
Figure 2. Venus leg ulcer infrared thermography. A.Left leg baseline, wound temperature 99.2°F, epithelialized area temperature 96.7°F; B. Left leg after 2 weeks of treatment, wound temperature 96.0°F, epithelialized area temperature 96.8°F
Standard assessment of wounds has a strong subjective component, and confirmatory microbiologic testing can take time. The real-time visualization afforded by infrared thermography adds a layer of confidence to wound assessment and can help inform management decisions. Further study of infrared thermography and FSOD use is warranted
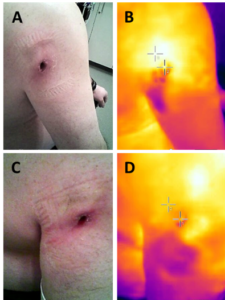 Figure 3. Right arm wound. A. Wound prior to FSOD dressing application. B. Infrared thermography of wound, temperature measured 101.2°F and 98.1°F; C. Wound after 2 weeks of FSOD treatment; D. Infrared thermography of wound after 2 weeks of FSOD treatment, temperature measured 97.3°F and 97.9°F.
Figure 3. Right arm wound. A. Wound prior to FSOD dressing application. B. Infrared thermography of wound, temperature measured 101.2°F and 98.1°F; C. Wound after 2 weeks of FSOD treatment; D. Infrared thermography of wound after 2 weeks of FSOD treatment, temperature measured 97.3°F and 97.9°F.
References
1.Dick S, Kalan L, Thomason HA, Joshi Poonam. Unique chemical structure and clinical efficacy ofAg Oxysalts. Ostomy Wound Management;64(S1):1-8.
2.Bakeer M, Vair A, Keast D. Evaluation of silver-Impregnated dressings in a clinical setting: observations on efficacy and practicality. Paper presented at: Edmonton West Primary Care Network, May 2015, Edmonton, Canada.
3.Motta G, Merkle D, Milne CT, Saucier D. A multi-center prospective clinical evaluation and cost comparison of a new silver oxysalts dressing. Paper presented at: Wound, Ostomy, Continence Nurses Society 44th annual conference; June 2012, Charlotte, NC.
4.Dini V, Salvo P, Janowska A, Difrancesco F, BarbiniA, Romanelli M. Correlation between wound temperature obtained with an infrared camera and clinical wound bed score in venous leg ulcers. Wounds 2015; 27:274-278.
5.Milne, C. Using Objective Measurements to Evaluate Reduction in Inflammation andBioburden Response to application of a Fibrous Silver Oxysalt Dressing. Paper presented at: Symposium for Advanced Wound Care; April 2017. San Diego, CA.
Photos and patient information courtesy of Catherine Milne, ARPN, MSN Connecticut Clinical Nursing Associates, Bristol, CT.As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.NOTE: Specific indications, contraindications, warnings, precautions, and safety information may exist for Systagenix, KCI (Acelity companies), and Argent Limited Partnership products. Please consult a healthcare provider and production instructions for us prior to application.