Dr. Fernandez is a Clinical Assistant Professor of Surgery and Family Practice at the University of Texas Health Center at Tyler. He is also an Attending Teaching Staff in the Division of Surgery for Mother Frances Health System and East Texas Medical Center in Tyler. Dr. Fernandez obtained his residency training at Loyola University, the University of Illinois, the University of Chicago and Northwestern University, Chicago, Illinois, with special training in Trauma and Burns at Kings County Hospital, SUNY Down State System, Brooklyn, New York, NY. He is well published in multiple areas of research both in peer-reviewed articles and book chapters, and has made numerous oral and poster presentations at national and international conferences.
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
INTRODUCTION
Management of the Open Abdomen (OA) is an aspect of surgery that has expanded rapidly over the last 20 years.1 Some of the factors that have led to improved outcomes and decreased mortality in open abdomen cases include the following:
•Enhanced clinical perspective (from civilian and combat surgical experience)
•Improved understanding of the underlying pathophysiology that affects open abdomen patients
•A broader adoption of the concept of Damage Control Surgery (DCS) and the use of Temporary Abdominal Closure (TAC) in this patient population
CASE STUDY: PNEUMATOSIS INTESTINALIS
Chief Complaint
The patient is a 59-year-old female with a history of hypertension, coronary artery disease (with prior myocardial infarction / coronary stent placement), non-insulin dependent diabetes mellitus and a past surgical history of total abdominal hysterectomy and bilateral salpingo-oophorectomy, who presents with nausea and vomiting and diffuse abdominal pain out of proportion with the physical exam, in septic shock.
Work up
The most relevant abnormal laboratory results reveal a white blood cell count of 18 thousand with 9% bands, BUN / Creatinine is 12/75 respectively, and a serum glucose of 623 mg/dl.
A CT scan of the abdomen and pelvis with intravenous contrast reveals air in the portal system and liver (Figures 1, 2).
The patient was taken for emergent exploratory celiotomy and underwent the following procedures in the index case (Figures 3-5):
•80% Small Bowel Resection
•Cholecystectomy
•Appendectomy
•Central Venous Pressure and Arterial-Line placement in the operating room
•Damage Control Surgery / Open Abdomen
•Placement of the KCI ABThera™ Open
Abdomen Negative Pressure Therapy SystemThe patient underwent subsequent washouts at 48-hour intervals, multiple small bowel anastomoses (including at the ileo-cecal junction), as well endoluminal stent placement and revascularization of bilateral lower extremities due to ischemia from a cardiac-aorto-iliac embolism. The patient’s abdomen was closed on the fourth and final operative intervention with placement of a PREVENA™
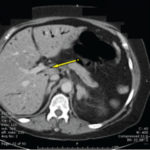 Figure 1. CT/AP: Air in Portal vein
Figure 1. CT/AP: Air in Portal vein
 Figure 2. CT/AB: Portal Air throughout the liver
Figure 2. CT/AB: Portal Air throughout the liver
Incision Management System (Figures 6-9).
On postoperative day 7, the PREVENA™ Incision Management System was removed and the underlying skin was found to be intact. On postoperative day 14, a CT of the abdomen and pelvis with oral contrast shows no evidence of abscess or anastomotic leak. The patient was discharged to a long-term hospital in stable condition, tolerating 4-6 small meals per day on hospital day 24 (Figure 10-12).
 Figure 3. Initial exploration reveals 80% dead small bowel
Figure 3. Initial exploration reveals 80% dead small bowel Figure 4. DCS/OA done; ABTheraTM dressing being applied.
Figure 4. DCS/OA done; ABTheraTM dressing being applied.
Brief Overview of the Problem
Over the past two decades, the way in which trauma surgeons approach an individual with multiple severe injuries has undergone an evolution. Trauma surgeons no longer attempt to fix everything during the initial operation. Stone and colleagues were the first to describe a technique of ‘truncated laparotomy’ for patients with clinically evident coagulopathy and retrospectively reviewed its efficacy in 1983.3 In 1993, Rotondo et al retrospectively reviewed the management of patients undergoing laparotomy for exsanguinating penetrating injuries (requiring transfusion of >10 units of packed red blood cells [PRBC]).4Studies in subsequent years have validated this technique by demonstrating decreased mortality and immediate post-operative complications. In the previously mentioned paper, Rotondo and colleagues modified the naval concept of damage control for ship salvage and coined the term Damage Control Surgery for use in the trauma setting.
 Figure 6. Multiple small bowel anastomoses done on remaining 50cm of small intestine
Figure 6. Multiple small bowel anastomoses done on remaining 50cm of small intestine
The current literature reflects the cumulative experience of trauma/acute care surgeons, which affirms that conservative (truncated) operative techniques and short operating times, even when all organ repairs have not been completed, increases survival in civilian and military patients with multiple trauma. These principles hold true for all affected regions of the body, including the abdominal cavity and its contents.
 Figure 7. Multiple small bowel anastomoses done on remaining 50cm of small intestine
Figure 7. Multiple small bowel anastomoses done on remaining 50cm of small intestine
Discussion: Damage Control Surgery, TAC and Management of the Open Abdomen
The indications for damage control laparotomy have evolved not only to encompass abdominal compartment syndrome, but abdominal sepsis, abdominal vascular catastrophies and other aspects of acute care surgery (including, but not limited to neck, orthopedic, thoracic, and military injuries).
 Figure 8. Ileo-Cecal valve preserved
Figure 8. Ileo-Cecal valve preserved
 Figure 9. PREVENATM Incision Management System in place
Figure 9. PREVENATM Incision Management System in place
The concepts of Damage Control Resuscitation, and those aspects that form the Total Management of the Open Abdomen (e.g. perioperative critical care, sedation, paralysis, nutrition, and fluid management strategies) as described by Demetriades, Kaplan, Miller and others, may improve closure rates and recovery.12-15 In the management of OA, the primary goal is to close the wound as quickly as physiologically possible, preferably within 7 to 8 days. Indeed, Miller’s reported findings suggest a progressive complication rate and morbidity and mortality increase after failure to close the abdomen without significant fascial tension before the 8th day of temporary TAC. Following these authors’ recommendations, most open abdomens may be successfully closed within 7-10 days. In the rare cases of inability to primarily close the abdomen, there are a number of reconstructive strategies that may be used in the acute and chronic phases of abdominal closure.
The benefits of managing patients with an open abdomen include prevention of intra-abdominal hypertension (IAH) and abdominal compartment syndrome (ACS), early identification of intra-abdominal complications (e.g. bowel ischemia) and ease of re-entry. Despite these benefits, maintenance of an open abdomen creates numerous management challenges such as development of fistula and infection. Prolonged maintenance of an open abdomen may also lead to a reduced chance of re-approximation of the fascia, as abdominal contents become ‘fixed.’
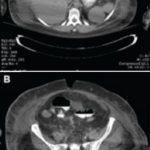 Figure 11. CT/AB with PI shows no anastomotic leak
Figure 11. CT/AB with PI shows no anastomotic leak
With increasing adoption of open abdomen techniques has come an increased demand for Temporary Abdominal Closure (TAC) methods to protect the Open Abdomen during the phase of open treatment. Principal techniques for TAC are: Negative Pressure Therapy (NPT), Vacuum-Pack method, artificial burr (Whitmann Patch™, Starsurgical, Inc.), absorbable mesh/sheet, zipper, “plastic silo,” skin closure and dynamic retention sutures. These techniques vary in their efficacy with regard to fascial closure rates, associated morbidity and mortality rates.
 Figure 12. Patient tolerating elemental tube feeding
Figure 12. Patient tolerating elemental tube feeding
In an austere setting, first-line management of the open abdomen may include use of dressings or impermeable devices (eg Bogota bag) to protect the exposed organs and limit leakage of fluid. The abdomen may be left to heal by secondary intention, or delayed closure may be done using sutures, mesh repair (biologic mesh preferred), skin grafts, muscle flaps or a combination of these. The choice of closure technique depends on the size of the wound and other clinical and local resource considerations.
SUMMARY
As discussed above, a number of systematic reviews, expert opinion and growing surgical experience with the management of the open abdomen have concluded that the artificial burr and NPWT have the highest fascial closure and lowest mortality rates when used alone.3,4 Negative pressure wound therapy (NPWT) for the open abdomen may be used in the management of patients with an open abdominal wound (laparostomy) when the gut and other intra-peritoneal organs are exposed. Because of its relative ease of application, and preservation of fascial tissue, NPWT is becoming a dominant choice for TAC in the open abdomen patient, particularly when used synergistically with biologic mesh as an adjunct for abdominal closure.
References
1.MacLean AA, O’Keeffe T, Augenstein J: Management strategies for the open abdomen: survey of the American Association for the Surgery of Trauma membership. Acta Chir Belg. 2008, 108: 212-218. PubMed Google Scholar
2.Cheatham ML, Safcsak K: Is the evolving management of intra-abdominal hypertension and abdominal compartment syndrome improving survival. Crit Care Med. 2010, 38: 402-407. 10.1097/CCM.0b013e3181b9e9b1. View ArticlePubMedGoogle Scholar
3.Stone HH, Strom PR, Mullins RJ. Management of the major coagulopathy with onset during laparotomy. Ann Surg 1983;197:532–5.
4.Rotondo MF, Schwab CW, McGonigal MD, et al. ‘Damage control’: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma 1993; 35:375–82.
5.Warfare Manual. Department of the Navy. The Department; Washington (DC): 1996.
6.Fernandez LG. Temporary Abdominal Closure Techniques. http://emedicine.medscape.com/article/196820-overview, Updated: Sep 01, 2015
7.Granchi T, Schmittling Z, Vascuez J, et al. Prolonged use of intraluminal arterial shunts without systemic anticoagulation. Am J Surg. 2000; 180:493–6. [PubMed]
8.Scalea TM, Boswell SA, Scott JD, et al. External fixation as a bridge to nailing for patients with multiple injuries and with femur fractures: damage control orthopedics. J Trauma. 2000; 48:613–21. [PubMed]
9.Vargo DJ, Battistella FD. Abbreviated thoracotomy and temporary chest closure: an application of damage control after thoracic trauma. Arch Surg. 2001; 136:21–24. [PubMed]
10.Holcomb JB, Helling TS, Hirshber A. Military, civilian and rural application of the damage control philosophy. Mil Med. 2001; 166:490–3. [PubMed]
11.Godat L, Kobayashi L, Costantini T, et al. Abdominal damage control surgery and reconstruction: World society of emergency surgery position paper. World J Emerg Surg. 2013, 8 (1): 53-10.1186/1749-7922-8-53.PubMed CentralPubMedGoogle Scholar
12.Demetrios Demetriades. Total management of the open abdomen. Int Wound J. 2012 August; 9 (Suppl 1): 17–24. doi: 10.1111/j.1742-481X.2012.01018.x
13.Kaplan M, Banwell P, Orgill D, et al. Guidelines for the Management of the Open Abdomen. Wounds Suppl.: 2005.
14.Miller RS, Morris JA Jr, Diaz JJ Jr, et al. Complications after 344 damage-control open celiotomies. J Trauma. 2005; 59(6): 1365–71. doi: 10.1097/01.ta.0000196004.49422.af. [PubMed] [Cross Ref]
15.Coccolini F, Biffl W, Catena F, et al. The open abdomen, indications, management and definitive closure. World J Emerg Surg. 2015; 10:32. doi: 10.1186/s13017-015-0026-5. [PMC free article] [PubMed] [Cross Ref]
16.Quyn AJ, Johnston C, Hall D, et al.. The open Abdomen and Temporary Abdominal Closure Systems – Historical Evolution and Systematic Review, Colorectal disease: the official journal of the Association of Coloproctology of Great Britain and Ireland. 2012. Google Scholar
17.Boele van Hensbroek P, Wind J, Dijkgraaf MGW, et al. Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. World J Surg. 2009, 33: 199-207. 10.1007/s00268-008-9867-3. PubMed CentralView ArticlePubMedGoogle Scholar
18.Fernandez L, Norwood S, Roettger R, et al. Temporary intravenous bag silo closure in severe abdominal trauma. J Trauma. 1996 Feb. 40(2): 258-60. [Medline].
19.Fernandez L, Norwood S, Wilkins H 3rd, et al. Intraperitoneal silo: a form of temporary abdominal closure. Surg Rounds. 1999. 22:467-478.



