
Kara Couch is a Family Nurse Practitioner and Certified Wound Specialist, who has been working in wound care for the past 13 years. She is a member of the Board of Directors for both the Association for the Advancement of Wound Care (AAWC) and the Alliance of Woundcare Stakeholders. Kara also serves as co-leader of the International Consolidated Venous Ulcer Guidelines for AAWC and has authored or co-authored numerous articles and chapters on wound healing. She lectures nationally on wound care and wound healing topics.
Couch_Current Dialogues in Wound Management_2017_Volume 3_Issue 1
A diabetic foot ulcer precedes 84% of all non-traumatic lower extremity amputations1. Within the world, every 20 seconds, someone loses a limb due to diabetes2. In 2014, the American Diabetes Association noted that in a single day in the United States, 200 lives are lost, 200 limbs amputated and 86 million people were at risk for complications due to diabetes3. It has been known for decades that the morbidity and mortality rates skyrocket after major amputation. After a major amputation, 50% of people will have their other limb amputated within 2 years5. The relative 5-year mortality rate after limb amputation is 68%. When compared with the mortality rates of various cancers, the mortality rates associated with diabetic foot ulcers are second only to lung cancer at 86%. By comparison, the mortality rates for other common cancers are colorectal cancer 39%, breast cancer 23%, Hodgkin’s disease 18%, and prostate cancer 8%
The life expectancy of an amputee is measured in months, not years, after the procedure and so it is important to work swiftly towards prosthetic fitting and gait training. If a patient is unable to do so due to co-morbid conditions, they will likely be wheelchair bound for the rest of their lives. Early engagement with physical medicine and rehabilitation is key to assess for possible barriers to using a prosthetic as well as to develop an appropriate treatment plan.
Once an amputation occurs, the clinical focus should shift towards preparing the residual limb for a prosthesis. The distal residual limb is in the shape of a square (Image 1) postoperatively but needs to be conical to fit in a socket properly. Edema reduction is a key component of this. Either an ACE® bandage (Becton, Dickinson and Company, Franklin, NJ) or a rigid dressing can be applied intraoperatively and maintained for 1-4 days postoperatively (Fig 1 and 2). The ACE® bandage (Becton, Dickinson and Company, Franklin, NJ) needs to be wrapped evenly and may need to be re-done if it loosens or becomes dislodged. However, these allow for visual inspection of the residual limb. Rigid dressings are made from plaster and also can reduce the limb volume effectively. They can act as a barrier to protect the residual limb from trauma and can prevent knee contracture. However, they do not allow for visualization of the limb. They can place the patient at risk for ulceration and also are challenging in those with neuropathy. In addition to rigid dressings, early prone positioning can help to prevent hip flexion contractures.
After the first few days of edema control, a stump shrinker should be used to continue to effectively reduce volume. In the absence of having a stump shrinker from a prosthetist, a compression dressing such as TUBIGRIP™ (Molnlycke Health Care AB, Gothenburg, Sweden) can be used. If there is significant edema, compression bandage systems such as an Unna Boot or multi-layer bandages can be applied safely (Image 2)6. These are typically changed every 5-7 days. The shrinker/compression wrap should continue until the patient is ready to be fit with a liner, which is usually 4-6 weeks postoperatively.
Immediate wound care is relatively straightforward and consists of monitoring the incision. As sutures can be snagged on elastic bandages or shrinkers, a simple dressing of post-op sponges or ABD pads can be applied to protect the incision. If there is any exudate coming from the incision, this can be managed using a foam dressing and then donning a shrinker. Some patients are considered high risk for wound complications and have negative pressure wound therapy (NPWT) applied in the operating room (OR) over the fresh incision. Elastic/ACE® Bandages (Becton, Dickinson and Company, Franklin, NJ)can be applied safely over NPWT, while taking care to place the tubing on the outside of the wrap.
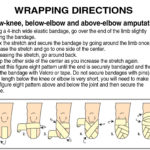 Figure 1. Wrapping directions for below-knee, below-elbow and above-elbow amputations
Figure 1. Wrapping directions for below-knee, below-elbow and above-elbow amputations
Just as patients with diabetes are instructed to inspect their feet daily for new areas of concern, amputees need to check their residual limb for any new skin concerns or possible trauma related to their prosthesis7. This can be accomplished by using a mirror or having a family member examine the limb. As with diabetes, retinopathy can negatively affect the patient’s ability to assess the limb for a problem. Education for the patient of what is normal and what is abnormal is necessary, in addition to assessing if the patient can actually see if there is an issue. Initially, patients should inspect their residual limb at each liner change or socket application as well as when they are removed. This surveillance allows for early identification of a potential problem and swift intervention.
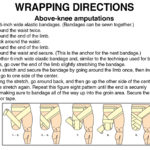 Figure 2. Wrapping directions for above-knee amputations
Figure 2. Wrapping directions for above-knee amputations
Distal residual limbs need to be washed daily with a mild soap and carefully dried prior to donning a liner or shrinker to prevent dermatitis. Patients should be cautious to use hot water, alcohol or to shave the limb as that can promote excessive drying/microtrauma of the skin, which can lead to fissuring and cracking once the liner is re-donned. The liner and shrinker require careful cleansing to reduce buildup of bacteria that can cause a superinfection of the limb. At nighttime, moisturizing of the residual limb is indicated as it is typically not necessary to sleep wearing a shrinker or liner. Some patients experience an increase in perspiration of the residual limb. Various treatment regimens exist, including the use of applying antiperspirant to the skin and BOTOX® (Allergan Inc., New Jersey, United States) injections, in extreme cases.
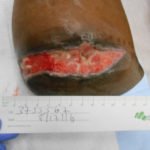 Image 1. Dehisced BKA, note the squared edge since patient had zero compression for the past 6 weeks since amputation
Image 1. Dehisced BKA, note the squared edge since patient had zero compression for the past 6 weeks since amputation
To prepare for prosthetic fitting, patients can employ several techniques to de-sensitize the limb and help with nerve repair. Scar massage of this incision by performing a series of “X” and “O” motions along the scar helps to reduce any keloiding as well as to help solidify the collagen. The use of a cotton ball swiped along the residual limb helps to remind the limb about touch and to prepare it for contact with a shrinker/liner/socket. Light tapping (using 2 fingers) along the skin gradually increases tolerance to pressure. All of these modalities can be initiated within the first week postoperatively.
 Image 2. Multi-layer compression applied to distal residual limb
Image 2. Multi-layer compression applied to distal residual limb
Early physical and occupational therapy (within the first few days of procedure) is key to help adapt the patient to their recovery process6,7. Physical and Occupational Therapists (PT, OT) are critical to successful recovery post-amputation. Not only do they help the patient learn to walk again, but they prepare the body for the physical stress of ambulation with a prosthesis. Gait training with a prosthesis is extremely challenging for both therapist and patient as the patient must re-learn biomechanics of ambulation along with using a prosthesis. PTs are expert teachers in gait training and they also spend quite a bit of time educating the patient on the de-sensitization techniques as well as limb assessments as described above.
Once the incision is healed and the distal residual limb has been shaped for a prosthetic, socket fitting can begin. This is typically 4-6 weeks after surgery if all goes well. Amputees will have a test socket made and then a series of adjustments are made prior to the final socket mold. During this time, skin conditions such as pressure ulcers or contact dermatitis can occur. Prompt evaluation and intervention by a wound provider hastens recovery from these issues so that the overall process doesn’t become too delayed.
Gait training with the prosthesis is the next step. A brief stay in an acute rehab unit should be considered to provide intensive therapy and allow the patient to become very familiar with the socket and how they can accomplish their activities of daily living. Some patients may only ambulate in their home while others may be able to become very high functioning over time.
The contralateral limb should not be ignored during this process. If the amputation was due to diabetes and/or peripheral arterial disease, careful monitoring of the other limb is needed to ensure that the same process is not going to threaten the sound limb. The added pressure of being the sound limb can predispose it to development of ulcers and abrasions since there is increased pressure during ambulation. If evidence of peripheral arterial disease (PAD) is present, surveillance non-invasive testing can be done every 6 months in the absence of an ulcer and should be repeated immediately if a new ulcer develops.
Finally, the psychological impact of becoming an amputee cannot be ignored by providers9. Patients will grieve for their lost limb and fear the loss of independence in their lives. Assessment of a depressive state/coping challenges with limb loss should be done pre-operatively (in an ideal environment) and certainly postoperatively. Psychiatric evaluation is indicated for patients who exhibit signs of depression and anxiety, such as withdrawal from care plans, refusal to look at their residual limb, and refusal to engage with rehabilitation1,9. There are many amputee support groups available for assistance, as well as peer visitors who will come to the bedside and educate patients’ on their new normal. Patients also derive great strength from their faith and assistance from their congregations provides great emotional support. The Amputee Coalition of America (www.amputee-coalition.org) offers resources and education for patients, caregivers and providers to help the amputee achieve their full potential after amputation..
In summary, care of the amputee patient does not cease once the procedure is completed. Amputees require a great deal of education and training on how to successfully complete their activities of daily living and also how to navigate their new normal life. Integration of care among disciplines and careful surveillance of both limbs reduces the likelihood of complications after amputation.
References
1.Neal R. Barshes, Meena Sigireddi, James S. Wrobel, Archana Mahankali, Jeffrey M. Robbins, Panos Kougias, David G. Armstrong. The system of care for the diabetic foot: objectives, outcomes, and opportunities. Diabet Foot Ankle. 2013; 4.
2. Bharara, Mills, Suresh, Armstrong, Int Wound J, 2009
3.American Diabetes Association 2014
4.Armstrong, et al, J Amer Podiatr Med Assn, 1997
5.Armstrong, et al, Guest Editorial: Are diabetes-related wounds and amputations worse than cancer? International Wound Journal, 2007
6.Ficke, J. Transtibial Amputation: Surgical Management. Management of Adults with Lower Limb Amputations. In. Atlas of Amputations and Limb Deficiencies, 4th edition. 485-492. 2016
7.Dudek NL, Marks MB, Marshall SC. Skin problems in an Amputee Clinic. American Journal Physical Medicine & Rehabilitation. 2006; 85:424-429.
8.Gailey RS, Gaunaurd IA, Laferrier JZ. Physical Therapy Management of Adults with Lower Limb Amputations. In. Atlas of Amputations and Limb Deficiencies, 4th edition. 597-620. 2016
9.MacKenzie EJ, Wegener ST. Psychological Adaptation to Limb Amputation. In. Atlas of Amputations and Limb Deficiencies, 4thedition. 719-730. 2016

