
Liz McElroy is a Nurse Practitioner in Wound, Ostomy, and Continence Care at the Reading Health System in West Reading, PA. She graduated from Gwynedd Mercy University with her MSN in Adult Nurse Practitioner in 2009, became a Certified Wound Specialist (CWS) in 2010, and certified in Wound, Ostomy, and Continence (CWOCN) in 2012. She serves as an in-patient wound, ostomy, and continence specialist for a 647-bed Level II Trauma Center. She focuses on care of the perioperative, post-operative, cardiac and critical care patients, with an interest in nursing and physician education and V.A.C. VERAFLO™ Therapy. She also has two years experience in an outpatient wound care center prior to her acute care position.
McElroy_Current Dialogues in Wound Management_2017_Volume 3_Issue 1
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
As an in-patient consultant for wound, ostomy, and continence needs for an in-patient population at a 700+bed Level II Trauma Center, there are a wide variety of wounds and wound care needs that are addressed. When dealing with the trauma patient population, the numerous consults required to meet the patient’s needs offers a unique interdisciplinary team that manage Negative Pressure Wound Therapy (NPWT). The needs of each team and each patient are quite different. “NPWT offers a quick and reliable method for sealing the wound from nosocomial contaminants. Furthermore, by promoting local wound perfusion and drainage, definitive management can be safely delayed beyond the initial physiologic stabilization of the traumatized patient”.¹
From years of experience in this role, I have found three major categories of orthopedic trauma wounds:
1.Open traumatic injury requiring delayed primary closure or flap surgery
2.Open soft tissue deficit with closed orthopedic injury related to traumatic injury
3.Closed primary incision status post orthopedic surgical repair
Negative pressure wound therapy (NPWT) can play a key role in wound healing for each of the above wound categories, while each wound have a different set of needs and concerns. When ordering V.A.C. Therapy Systems for home use, the associated paperwork is an excellent tool for the prescribing clinician to utilize; as it focuses on identifying the outcome goal for the NPWT Therapy.”
The surgical staff should also be thinking of these goals when they are making decisions around the next stage of the patient’s care.
![]() Figure 1. Acelity V.A.C.® Therapy Insurance Authorization Form.
Figure 1. Acelity V.A.C.® Therapy Insurance Authorization Form.
Willy lists five mechanisms by which the application of negative pressure to a wound may aid in the healing process: 1) wound retraction, 2) stimulation of granulation tissue formation, 3) continuous wound cleansing after adequate primary surgical debridement, 4) continuous removal of exudate, and 5) reduction of interstitial edema.³
One common theme of each of the wound categories in traumatic orthopedic injuries is the management of edema surrounding the wound. The pathology of wound healing describes edema formation as part of the inflammatory phase of wound healing. For trauma patients, the initial injury starts this process, but it is often interrupted and restarted when the patient undergoes surgery. The inflammatory phase can last up to 72 hours. Managing the periwound edema in any type of wound, including a closed incision, is key to successful coaptation of the wound edge and proliferation of granulation tissue. This allows adequate perfusion and facilitation of the immune response in the surrounding tissue. Each wound type will have slightly different treatment plans and strategies however.
For open traumatic injuries requiring delayed primary closure or flap surgery, there are two phases of repair. First is orthopedic repair and wound stabilization. Negative pressure wound therapy (NPWT) or negative pressure wound therapy with instillation and dwell (NPWTi-d) can be used to help temporize the soft tissue deficit after a traumatic orthopedic injury. The choice of whether or not to use NPWTi-d versus NPWT can depend on a variety of factors including location of wound, nature of injury, appearance of wound base, and patient factors such as a BMI> 30, diabetes, current tobacco use, poor nutritional status, corticosteroid use,a history of wound infection, delayed healing, or fistula/ ostomy, and poor tissue quality at time of closure. The ability of the NPWT to provide macro and micro strain will aid in meeting the complex wound care needs. The principles of macro strain with NPWT are that NPWT can decrease wound margins, remove exudates, reduce edema, and remove infectious material.4 This can be of particular importance when the orthopedic team is placing screws, plates or other hardware onto the bone that could pose a risk of getting an implant infection. As the consequences for surgical site infections become greater, the surgeon needs to consider if the wound is ready to be closed. Prevention of these surgical site infections (SSI) are of upmost importance for quality patient care and prevention of financial penalties associated with hospital acquired infections (HAI). This is why NPWT or NPWTi-d can play such a major role in the management of open orthopedic injuries. Clinically, NPWT has been found to prepare the wound bed for closure and be able to remove enough edema that the tension on suture line at time of closure is less. Once closure is performed, the surgeon should consider the patient factors to determine whether or not to place incisional negative pressure wound therapy. In our institution, as an example, we have a checklist of comorbidities that may increase the risk of wound complications. If the patient has three of these comorbidities, we recommended the application of Prevena™ Incision Management System or incisional NPWT.
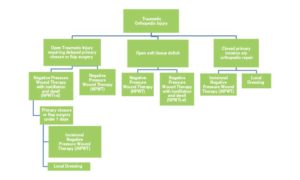 Proposed decision making tree for wound care options to consider for traumatic orthopedic injuries.
Proposed decision making tree for wound care options to consider for traumatic orthopedic injuries.
The second category of orthopedic trauma injury is a soft tissue deficit that is left open to heal by secondary intention. When closure is not a viable option after a surgical washout after initial presentation of the injury, the surgeons tend to leave the deficit open, to fill in by secondary intention. Negative pressure wound therapy is the gold standard for assisting in granulation tissue formation. Recently we have introduced the use of NPWTi-d to aid in getting an even better improvement in the granulation tissue proliferation. At my institution, the surgical staff initially held some resistance to utilizing the NPWTi-d, due to a lack of understanding around its benefits and the perceived increase in workload required but now they have come to utilize this technology for a majority of the cases due to experience, education and the use of real-world case studies. If the case is late or they aren’t confident about application, they place the NPWTi-d dressing while in the OR, and then consult the WOCN to set up the instillation settings the following day since the WOCN team is a courtesy service at our institution and not on-call. This is a good compromise to get the instillation therapy started as soon as possible while not prolonging time in the OR. The field continues to develop research surrounding the type of solution to instill and dwell settings for the use of NPWTi-d.
Patients who undergo an orthopedic repair with delayed closure have two options for incisional wound care at the time of closing. One option is Prevena™ negative pressure wound therapy, which is placed in the operating room at the time of incision closure. The other option would be that of local incisional wound dressings. The use of incisional negative pressure wound therapy is a relatively new therapy that has shown positive clinical outcomes in the management of closed surgical incisions by holding incision edges together, covering and protecting the incision from external contamination and removing fluid and infectiousmaterials.5 Stannard found incisional negative pressure wound therapy to be an effective wound care strategy for high risk fractures, suchas tibial plateau, pilon, and calcaneal fractures.
 Figure 2. Crush injury with fracture blister that was debrided to exposed tendon. Clinical decision made to close by secondary intention; NPWT to be applied.
Figure 2. Crush injury with fracture blister that was debrided to exposed tendon. Clinical decision made to close by secondary intention; NPWT to be applied.
The use of NPWT in various forms: closed incisional negative pressure wound therapy, negative pressure wound therapy with instillation and dwell, or negative pressure wound therapy, can improve the patient, clinician and hospital’s outcomes in the orthopedic trauma population. The author proposed a decision making tree for these injuries. Factors to consider are the surgical wound classification, tissue quality, other co-morbidities, edema, and use of hardware. There should be more data collection about the use of NPWT in its various forms to help clinicians utilize these therapies for better patient outcomes. While initial data shows improved outcomes with the use of NPWT, treatment algorithms should be developed and evaluated to integrate into potential clinical pathways for orthopedic trauma surgery.
 Figure 3. S/P ORIF LEFT DISTAL HUMERUS FRACTURE s/p MCC. Prevena™ Incision Management System applied for 5 days, dressing changed once for a total of 10 days of therapy, then transitioned to silver dressing; (ciNPWT changed due to institutional protocol; 5 days is typical length of time dressing kept in place before re-evaluation of wound; reapplication due to some periwound edema and slight maceration at wound edge)
Figure 3. S/P ORIF LEFT DISTAL HUMERUS FRACTURE s/p MCC. Prevena™ Incision Management System applied for 5 days, dressing changed once for a total of 10 days of therapy, then transitioned to silver dressing; (ciNPWT changed due to institutional protocol; 5 days is typical length of time dressing kept in place before re-evaluation of wound; reapplication due to some periwound edema and slight maceration at wound edge)
 Figure 4. Open fracture stabilized with NPWTi-d utilizing 20mL of a normal saline solution, dwell 5 minutes, every 3.5 hours at 125mmHG until flap procedure performed 2 days later
Figure 4. Open fracture stabilized with NPWTi-d utilizing 20mL of a normal saline solution, dwell 5 minutes, every 3.5 hours at 125mmHG until flap procedure performed 2 days later
References
1.Streubel, P. N., Stinner, D. J., & Obremskey, W. T. (2012). Use of negative-pressure wound therapy in orthopaedic trauma. The Journal Of The American Academy Of Orthopaedic Surgeons, 20(9), 564-574. doi:10.5435/JAAOS-20-09-564
2.Acelity™ (2016). V.A.C.® Therapy Insurance Authorization Form. Retrieved from: http://www.acelity.com/vac-therapy-insurance-auth.
3.Willy C, editor. (2006) The theory and practice of vacuum therapy. Scientific basis, indications for use, case reports, practical advice. Ulm,Germany: Lindqvist book publishing; p. 405.
4.Gupta, S., Gabriel, A., Lantis, J., & Téot, L. (2016). Clinical recommendations and practical guide for negative pressure wound therapy with instillation. International Wound Journal, 13(2), 159-174. doi:10.1111/iwj.12452
5.Willy, C., Engelhardt, M., Stichling, M., & Grauhan, O. (2016). The impact of surgical site occurrences and the role of closed incision negative pressure therapy. International Wound Journal, 1335-4
6. doi:10.1111/iwj.126596.Stannard, J., Volgas, D., McGwin G, 3., Stewart, R., Obremskey, W., Moore, T., & Anglen, J. (2012). Incisional negative pressure wound therapy after high-risk lower extremity fractures. Journal Of Orthopaedic Trauma, 26(1), 37-42.

