Liz McElroy is a Nurse Practitioner in Wound, Ostomy, and Continence Care at the Reading Health System in West Reading, PA. She graduated from Gwynedd Mercy University with her MSN in Adult Nurse Practitioner in 2009, became a Certified Wound Specialist (CWS) in 2010, and certified in Wound, Ostomy, and Continence (CWOCN) in 2012. She serves as an in-patient wound, ostomy, and continence specialist for a 647-bed Level II Trauma Center. She focuses on care of the perioperative, post-operative, cardiac and critical care patients, with an interest in nursing and physician education and V.A.C. VERAFLO™ Therapy. She also has two years experience in an outpatient wound care center prior to her acute care position.
McElroy_Current Dialogues in Wound Management_2017_Volume 3_Issue 3
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
Every year when I go to conference, there is usually a new buzz word or focus for the year. In the last several years, wound bed preparation and skin substitutes were the buzz words of the conference season. This past year I would say that biofilm has taken over as the buzz word of conferences. When discussing wound bed preparation, especially as it relates to chronic wound care, an important part of the conversation is the role of biofilm in wound bed preparation. By definition, wound bed preparation is a concept emphasizing a holistic and systemic approach to evaluate and remove barriers to the healing process to allow the wound healing process to progress normally1. The aim of wound bed preparation is the formation of good quality granulation tissue leading to complete wound closure. Management of the wound bed can accelerate healing so that other therapies can be effective in aiding in wound closure.
In a literature search on wound bed preparation, there is no clear consensus on when a chronic lower extremity wound is “ready” for a skin substitute or skin graft. In 2003, TIME came out as an acronym to help clinicians think about wound bed preparation in a logistically, systematic fashion. TIME stands for tissue debridement, infection or inflammation, moisture balance and edge effect. TIME was created by the International Wound Bed Preparation Advisory Board as a guide for clinicians to help with dressing and therapy selection to meet the needs of the wound and the patient. Ideal conditions for successful STSG include red granulation tissue dominating the wound bed, no visible tendon or bone, no discernible sloughing or exudate in wound, no residual necrotic tissue, no local signs of soft-tissue infection, no systemic signs of infection, and no severe peripheral arterial disease (ankle-brachial index 0.9 or distal pulses present)2. When educating newer wound care providers, I simplify this very complex subject by telling them that wound bed preparation, on a very basic level, is actively utilizing a treatment that will push the chronic wound out of the inflammatory phase and into the proliferative phase to facilitate healing or acceptance of a dermal or epidermal cover.
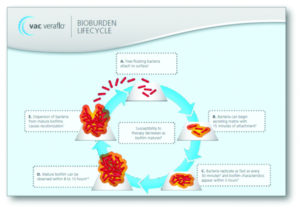
Each of the categories, tissue debridement, infection or inflammation, moisture balance, and edge effect, come with their own list of factors and therapies. When discussing the role of biofilm with wound bed preparation, the focus should be on tissue debridement and infection or inflammation. There are several different methods of debridement that can assist with the tissue debridement. Possible methods are surgical, mechanical, autolytic, enzymatic and biological methods. Surgical is preferred as it is fast and effective in the removal of non-viable tissue. However, surgical debridement is not always possible or feasible. It is important for the clinician to not only look at the needs of the wound, but the patient as well. As a wound care clinician in the acute care setting, I am aware of the issues that can arise to prevent a thorough surgical debridement from occurring in a timely manner: Lack of OR time, obtaining medical clearance, obtaining consent, patient stability and clinical factors, etc. When surgical debridement is not an immediate option, V.A.C. VERAFLO CLEANSE CHOICE™ Dressing when used in conjunction with V.A.C. VERAFLO™ Therapy is a viable wound cleansing option to assist in solubilizing the exudate and infectious material in the wound base with subsequent removal under negative pressure. There is also the use of an enzymatic debridement agent, especially in the outpatient and long-term settings where frequent debridement may not be possible. Regardless of the method, it is important that a good debridement occur, especially in the face of biofilm. A recent supplement to the WOUNDS journal3 focused on Wound Biofilm: Current perspectives and strategies n biofilm disruption and treatments. The “what we know about biofilm in chronic wounds” listed the following:
1.Biofilms exist and are prevalent in chronic wounds
2.Biofilms, in addition to other factors, are a barrier to wound healing.
3.Routine culture is not an effective means of identifying biofilm bacteria.
4. Biofilms have a natural ability to rebuild rapidly.
5.Systemic antibiotics are of limited use in managing biofilm.
6. Surgical or conservative sharp wound debridement is effective in removing biofilm from an open wound surface.
7. Appropriate topical antimicrobial application can suppress biofilm reformation.
Previously, it was thought that bacteria levels of 106 were considered infection. There are also symptoms that can lead a clinician to believe that the wound is infected or with biofilm such as increasing ulcer size, increasing exudate, and friable or unhealthy granulation tissue. Clinicians should carefully assess and treat for biofilm at every encounter as the panel agreed that biofilm was pervasive in chronic wounds, with some studies showing that it was present in 100% of all chronic wounds, potentially disrupting healing. Moisture balance should be achieved not only to provide good wound care but to also ensure that a STSG or skin substitute would be appropriate. The edge of the wound should also be properly managed, ensuring there is no epiboly or callous formation. After reviewing literature and speaking with the surgeons who apply skin substitutes and STSG, there are several methods that have been explored to prepare the wound bed and get a better sense of when the wound/ patient would be ready for a skin substitute or STSG. Visual examination of the wound base proving robust granulation tissue was one of the most common themes. Microbiology results have historically played a role in helping to determine if there was too great of a bacterial presence that the wound bed was well prepared. Finally, how the wound is progressing seemed to be one of the most important considerations.
When I completed the literature review, NPWT came up frequently as a treatment to help prepare the wound bed. With the use of V.A.C. VERAFLO™ Therapy and V.A.C. VERAFLO CLEANSE CHOICE™ Dressing now available, we may be able to expedite the preparation of the wound bed. V.AC. VERAFLO™ Therapy’s ability to prepare the wound bed is through the following mechanisms:
1.Cleansing via instillation of topical wound solution
2.Softening/solubilization of thick wound exudate such as fibrin and slough
3.Removal of wound exudate under negative pressure
4.Promoting granulation tissue formation
5.Decreasing edema
The impact of negative-pressure wound therapy with instillation of Prontosan® Wound Irrigation Solution* was compared with standard negative-pressure wound therapy in a retrospective, historical cohort – controlled study of patients whose infected wounds required hospitalization and surgical debridement. The results showed that wounds treated with V.A.C. VERAFLO™ Therapy were significantly more likely to be closed at time of discharge and had a decreased length of time to final procedure vs V.AC.® Therapy alone.4Lessing, et al. demonstrated in a porcine model on non- infected wounds a 43% improvement in granulation tissue formation with the use of V.A.C. VERAFLO™ Therapy with saline instillation vs standard V.A.C.® Therapy.5 What needs to be further explored is if utilizing the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing will impact any of this data.
Clinicians are left with lots of options for treatment of the wound bed in order to fully prepare the wound for final closure. With reduced funds for medical treatment, it is important that the clinician use the most advanced therapies early on in wounds that have failed to progress through the normal stages of healing. Facilitating a wound base to be able to accept a skin substitute or STSG could not only mean a time savings, but also in health care dollars. Additionally, the patient is less likely to develop an infection or have sequela from the open wound. Therefore, at the time of the initial encounter and at every encounter, the clinician needs to actively assess and address wound bed preparation in the face of biofilm.
References
1.Halim A S, Khoo T L, Mat Saad A Z. (2012). Wound bed preparation from a clinical perspective. Indian J Plast Surg; 45: 193-202.
2. Aerden D, Bosmans I, Vanmierlo B, Spinnael J, Keymeule B, Van den Brande P. (2013). Skin grafting the contaminated wound bed: reassessing the role of the preoperative swab. J Wound Care ; 22: 859.
3. Snyder RJ, Bohn G, Hanft J, Harkless L, Kim P, Lavery L, Schultz G, Wolcott R. (2017). Wound Biofilm: Current Perspectives and Strategies on Biofilm Disruption and Treatments. Wounds; June Supplement;29(6):S1-S17.
4. Kim PJ, Attinger CE, Steinberg JS, Evans KK, Powers KA, Hung RW, Smith JR, Rocha ZM, Lavery L. (2014). The impact of negative-pressure wound therapy with instillation compared with standard negative-pressure wound therapy: a retrospective, historical, cohort, controlled study. Plast Reconstr Surg; 133: 709-71
5. Lessing, C; Slack, P; Hong, KZ; Kilpadi, D; McNulty, A. (2011) Negative Pressure Wound Therapy With Controlled Saline Instillation (NPWTi): Dressing Properties and Granulation Response In Vivo. WOUNDS; 23 (10): 309-319.