Dr. Subhas Gupta is the Chairman of the Department of Plastic Surgery at Loma Linda University in Southern California where he holds the academic rank of Professor and is the director of research. He is an innovative plastic surgeon who holds a PhD in Medical Informatics focused on the introduction of new technologies to clinical care. He is the director of the Loma Linda University Soft Tissue Reconstruction Team and directs a bio-investigative cell biology and wound healing laboratory.
Gupta_Current Dialogues in Wound Management_2018_Volume 4_Issue 3
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
It never fails that when a plastic surgeon is called for a consult at 4:00 PM on a Friday afternoon, someone has a patient in the hospital with a wound that is not progressing.In this article, I want to share with you our strategic approach to the holistic management of our wound patients that makes the Friday afternoon consult a very rare occurrence.
Assessing a patient with a wound systematically and examining them systemically are the components of HOLISTIC wound management. While the complexity and severity of the wounds seen by a plastic surgeon are high, the principles of holistic wound management are consistent across all wound care professionals. Modern approaches to wound care generally consider primary disease processes, co-morbidities, and lifestyle factors. Identifying all of the etiologic factors for a wound is essential to treating it well. The sum of the patient history and findings allow for this holistic approach to diagnosis and should guide management of the patient.
A holistic approach to wound care includes several steps that should be performed in a consistent fashion. This starts with diagnosis including cues from the wound characteristics, and repeated assessment of progress once treatment has begun. Treatment must be inclusive of patient and wound preparation and follow-up to assess and hopefully prevent recurrence.
Creating a systematic model of this holistic approach may well be the ideal method of approaching chronic wounds which are notoriously difficult to heal and have high rates of recurrence.
Our recent guideline on this topic created a general guide for effective wound management from diagnosis to follow-up and is briefly outlined in Figure 1.1 The process is very much cyclical as many steps are repeated throughout treatment. A detailed assessment of the patient and the wound help ascertain the etiology of the wound. The multidisciplinary team has a focus of whole patient care and is not just wound-centric. The goals of therapy arereviewed with the patient, who becomes a stakeholder in the progress more than just being the object of care. We have found this to be valuable in increasing adherence to the care plan.
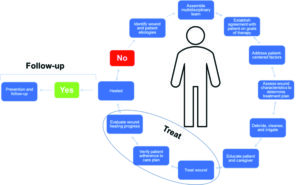 Figure 1. Holistic pathway for managing chronic wounds.1
Figure 1. Holistic pathway for managing chronic wounds.1
Wound debridement is a common entry point to the treatment portion of the cycle. Next, appropriate dressings and therapies are chosen based on wound etiology and characteristics. The healing progress is regularly assessed, and a follow-up plan is critical to reduce recurrence. Figure 1 summarizes this cycle of holistic wound care.
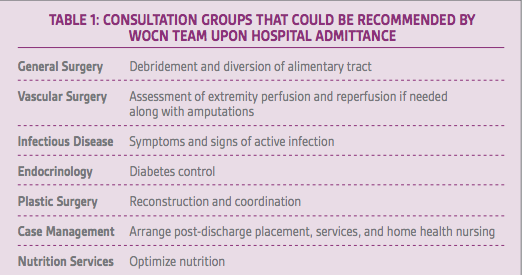
As a plastic surgeon, my introduction to the holistic pathway was initiated by a clearly identified unmet need: our wound care patients were spending time in the hospital for extended periods of time without progression of diagnosis and treatment. The “serial” model of operation of traditional care teams was replaced in a stepwise fashion by a “parallel” processing model of diagnosis and care. Initially, this applied to the diagnosis portion only, whereby the admitting service triggered a wound care nurse consultation that concluded with a list of recommended consultations for treatment. The services listed included the surgical teams of general surgery (debridement and diversion of alimentary tract), vascular surgery (assessment of extremity perfusion and reperfusion if needed along with amputations), infectious disease (symptoms and signs of active infection), endocrinology (diabetes control), plastic surgery (reconstruction and coordination), case management (arrange post-discharge placement, services, home health nursing), and nutrition services (optimize nutrition). The key to this process working was the initial “quarterbacking” done by our wound nurse consultant. The wound nursing team was given the authority to initiate all of the above consultations with a simple, defined list of criteria. Their consultation note produced “suggested orders” that the admitting team only had to co-sign. This abbreviated the time from understanding the wound to beginning treatment (Table 1) and removed 3.7 days on average from the length of stay. By letting the surgical services consult concurrently, this allowed for procedures to be performed during the same anesthetic for several patients. This
was the biggest factor in reducing length of stay as the plastic surgeons frequently went to the operating room (OR) with the other services and converted the open wounds to wounds that could be managed on an ambulatory basis.
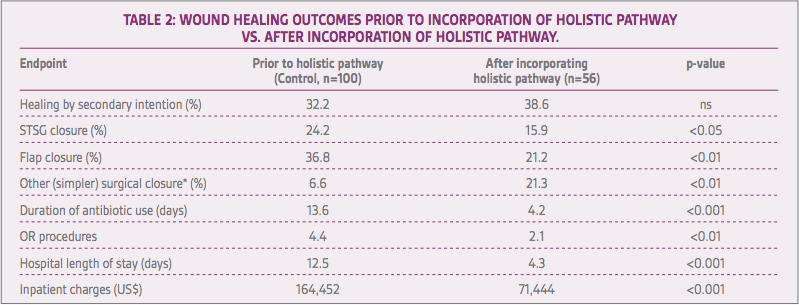
Overall, the improvements from this holistic pathway were broad. Compared to a historical cohort of control patients at our institution, the duration of antibiotic use (13.6 vs. 4.2 days, respectively; p<0.001), number of operating procedures (4.4 vs. 2.1, respectively; p<0.01), and length of hospital stay (12.5 vs. 4.3 days, respectively; p<0.001) were all significantly lower for the holistic-pathway treated patients. Inpatient charges were significantly lower for holistic-pathway treated patients compared to historic control patients ($71,444 vs. $164,452; p<0.001). A greater number of patients in the holistic-pathway group received simpler, less morbid surgical closures that were performed largely in an outpatient setting. The differences following the implementation of the pathway are summarized in Table 2.
The lessons we learned by implementing this system are important ones and should be actively considered for any institution that wishes to adopt a similar approach. Firstly, incorporating this management system involved a substantial re-organization of services that spanned from clinical services (e.g., infectious disease, wound care, and vascular surgery) to discharge planning, case management, and home health. And secondly, the key to success for this new process was the wound care nurse’s timely order placement and organization of parallel services for each patient. In the end, in our institution, the impact of this holistic wound patient management system has been tremendous, including a significant reduction in complexity of surgical closures, antibiotic use, OR procedures, hospital length of stay, and inpatient charges.
References
Gupta S, Andersen C, Black J et al. Management of Chronic Wounds: Diagnosis, Preparation, Treatment, and Follow-up. Wounds2017;29:S19-S36.