
Dr. Dennis Orgill is Vice Chairman for Quality Improvement in the Department of Surgery at Brigham and Women’s Hospital (BWH) and Professor of Surgery at Harvard Medical School. He is a reconstructive plastic surgeon and has a PhD from MIT in medical engineering. He is the Director of the BWH Wound Care Center and runs a tissue engineering and wound healing laboratory. His lab at BWH is working to develop better technologies to treat wounds including work with artificial skin, micromechanical forces, platelets, and stem cells. Dr. Orgill has consulted for several medical device and start-up companies and is the inventor on several patents. He worked on the team that developed Integra, a skin replacement therapy that has been commercially developed and used successfully on thousands of patients.
Orgill_Current Dialogues in Wound Management_2018_Volume 4_Issue 4
Despite great attention given to pressure injuries (PIs) by regulatory agencies and provider networks, the incidence of PIs continues to increase. PIs occur either as a result of shearing of the skin or because of a lack of blood flow that causes necrosis of tissues (Figure 1). We know that after about 2 hours of warm ischemia that irreversible changes in cell function occur that can lead to tissue necrosis. Once the tissue is dead, it needs to be removed before healing can occur. The body can remove some of this tissue by natural enzymes (autolytic), by externally applied enzymes (enzymatic debridement), or by mechanical means.
The vast majority of PIs are taken care of by nursing staff or physicians who do not have the capacity to do a surgical intervention. Fortunately, most of these healthcare providers are well trained, apply appropriate care, and promote healing in most cases. There are several types of wounds that do not heal and which referral to a surgeon may be beneficial. Most of the wounds referred to our clinic are deep, reaching muscle or bone (stage 3 and 4), that have been present for several weeks. Surgical techniques, particularly flaps, have the capacity to close the majority of wounds, although only a subset of patients may be good surgical candidates.
Prior to performing an operation, these are some of the questions I ask:
Why did they develop the PI and what can be done to minimize the chance of recurrence?
We commonly see spinal cord injury patients. People with paraplegia spend substantial time in their wheelchair but normally do not have sensation in their buttocks. They commonly present with ischial PIs that are a direct result of sitting too long without adequate off-loading. Making sure they have optimal sitting surfaces and an off-loading mattress are critical. More importantly, they need to commit to off-loading frequently while in the chair. Because they have good use of their upper extremities, many can do this while they are in their wheelchairs. In contrast, people with quadriplegia have limited use of their upper extremities, and it becomes more challenging to keep these wounds closed over a long time. Tilting wheelchairs can often relieve pressure in these cases. In contrast, someone who develops a PI as a result of a motor vehicle accident who becomes ambulatory has a good chance of healing the wound without the need for surgery. Being able to stand and walk provides a tremendous benefit to these patients.
Many patients with PIs do not understand off-loading. We have found some patients with PIs are admitted to the hospital for another reason where they have excellent nursing care with frequent turning and dressing changes. A proportion of these patients will heal their wounds while in the hospital without surgery.
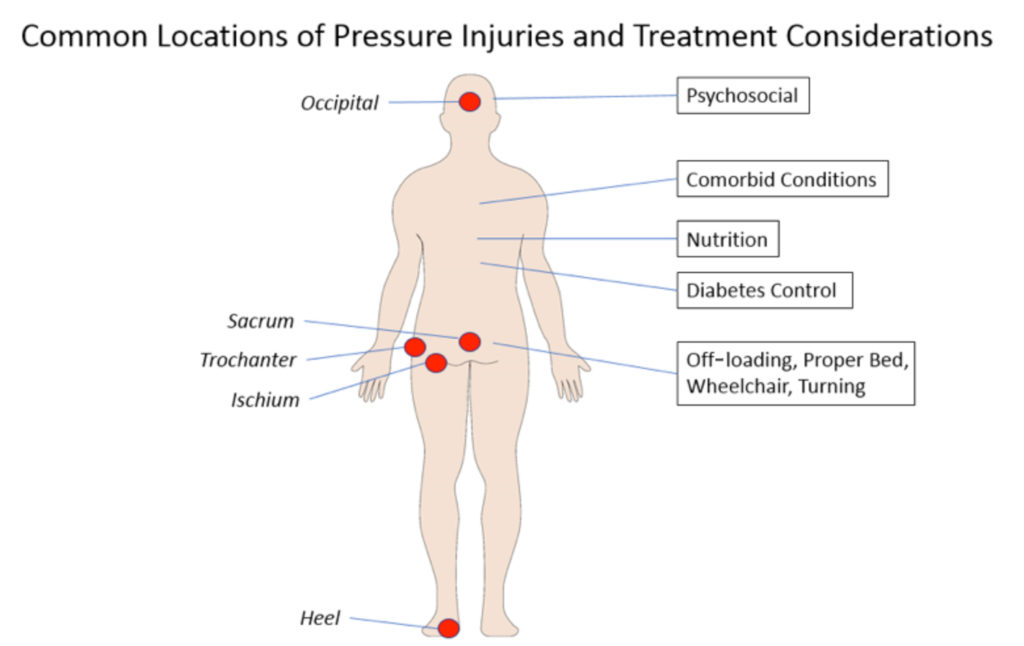 Figure 1. Common locations of Pls and treatment considerations. Pls occur in predictable locations that are dependent on the mobility impairment. Prior to operation, there are a number of treatment considerations to be evaluated.
Figure 1. Common locations of Pls and treatment considerations. Pls occur in predictable locations that are dependent on the mobility impairment. Prior to operation, there are a number of treatment considerations to be evaluated.
What is their nutritional status?
We see many patients whose nutrition is not optimal. Taking a careful history about diet, recent surgery, and weight changes can give the healthcare provider a good idea of an individual patient’s nutritional status. We find that serum measurement of albumin and prealbumin can be helpful in diagnosing malnutrition. It is well accepted in the surgical literature that patients with nutritional deficiency have delayed healing and higher complications if they undergo surgery. We place patients on high protein diets to try and reverse this prior to performing elective surgery. Often, we have found that by just correcting their nutrition, we can dramatically improve wound healing and, on occasion, patients have gone on to heal without the need for surgical intervention.
Paradoxically, obese individuals with PIs are often nutritionally depleted. In some cases, individuals who are morbidly obese need to lose substantial weight before an operation is appropriate. This is quite challenging, as weight loss often makes these patients catabolic and their nutritional status worse. Close collaboration with an expert in nutrition is helpful in many of our cases.
What is their care status at home?
We find many patients do not have adequate support at home to conduct dressing changes. Providing them with adequate resources to engage in positional changes is critical before elective surgery is scheduled.
Will they be able to comply with instructions when they return home?
We request that our patients keep all pressure off the closure for 6 weeks following surgery and then we start them on a gradual sitting protocol. We let them know that they will not be able to sit as much as before the operation. We also request that all patients return at 6 months following closure for follow up. This appointment with the surgeon seems to be highly motivating to keep the pressure off during this period. Hopefully, by this time, they have made permanent lifestyle modifications that will prevent recurrence.
What are their co-morbid conditions?
We have a number of patients with metastatic cancer, heart disease, pulmonary disease, or renal failure who may not be good candidates for surgery. Reversible factors such as poorly controlled diabetes are better dealt with before, rather than after an operation.
Do they have more than one PI?
In my clinical experience, I find that patients with more than one PI have a very high rate of recurrence. We try very hard to get all PIs to heal using non-surgical interventions. Occasionally, we will have to operate on more than one PI at a time, but these have very high rates of recurrence.
Have we done everything possible to shrink the wound?
I find that patients with smaller wounds tend to do better with surgery. We try to reduce the size of the wound as much as possible prior to attempting surgery. Ideally, this goes down to a single sinus tract. At that point, the wound can be excised easily, the bone shaved down, and a flap performed without putting undue tension on the skin closure. We commonly use negative pressure wound therapy devices to assist with wound bed preparation.
Do they understand the high rate of recurrence?
For many PIs, the reported incidence of recurrence over the long term can be as high as 50% or greater. I believe that doing the items mentioned above will reduce the risk of recurrence substantially. However, even in our clinic, we have some patients each year in whom PIs recur. These patients need to understand that addressing the wound soon after the injury develops will maximize the wound healing potential. We try to design our flap closure so if there is a recurrence, we can re-advance or re-use the flap.
FINAL THOUGHTS
The development of flaps for the treatment of PIs has been a great advance in plastic surgery and has benefited numerous patients with PIs. Being able to have a totally closed wound reduces infections. These operations are technically difficult to do as any breakdown in the closure often results in a wound that is twice as big as it was at the time of the original operation. In our clinic, we have found that our wound care nurse and our extended care team are critical in preparation for the patient’s surgery. Our goal is to prepare our patients as well as possible prior to surgery, to do the best operation that we can, and to provide them with the capacity to off-load their wound in the post-operative period.

