
Dr. Laurie Punch is an acute care surgeon with three areas of focus including surgical education, gun violence prevention and the management of soft tissue infection and injury. With a strong foundation in the management of necrotizing soft tissue infection at the University of Maryland where Dr. Punch trained as a resident and fellow, she has developed clinical expertise and an extensive curriculum in the management of soft tissue.
Punch_Current Dialogues in Wound Management_2019_Special Spring Edition
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
BACKGROUND
Soft tissue injury and infection both create inflammation which, in turn, creates edema and pain. When these processes lead to loss of the skin, fat, fascia, and muscle there are, from my personal experience, three distinct challenges that confront patients and clinicians:
1.Ongoing control of infection and contamination;
2.Ongoing management of fluid loss, inflammation, and edema;
3.Maintenance of tissue integrity and domain that will facilitate eventual soft tissue coverage and closure.
Over the course of my career, I have observed surgical and traumatic wounds with a large surface area as the result of a myriad of different processes such as necrotizing soft tissue infection, pressure injury, degloving injury, postoperative infection, intrinsic skin disease such as hidradenitis, and ulcers related to lymphatic or venous insufficiency. While definitive care requires appropriate system support of the patient overall, the process of wound healing and coverage can be supported through intentional tissue resuscitation. This resuscitation, in response to the above three challenges, includes:
1.Ongoing removal of infectious and necrotic material;
2.Reduction of tissue edema while maintaining wound moisture balance;
3.Wound edge approximation with promotion of new tissue growth.
Large inflamed and infected wounds are best treated with a combination of both negative pressure wound therapy with instillation (NPWTi) and can be used as an adjunctive therapy in the management of these wounds, along with appropriate clinical protocol of debridement and antibiotic therapy. These modes of wound management together provide these three components of tissue resuscitation extremely well as described throughout the literature.
The challenge then is the successful application of NPWTi to large wound beds. While the addition of instillation to negative pressure therapy after application is not uniquely challenging, ensuring there is an adequate seal and appropriate parameters set for NPWTi are essential for the dressing to be successful. In addition, the anatomical location of the large wound can influence the function of the dressing. Factors like patient movement, continence, positioning, and mobility may have a significant impact, all of which can be managed or mitigated with careful planning.
Many wound types demonstrate these three challenges as well as the benefits of applying NPWTi including:
1.Acute wounds resulting from necrotizing soft tissue infection of the torso, groin, and axilla;
2.Pressure injury of the ischium or sacrum including septic arthritis;
3.Traumatic wounds such as large burns or degloving injuries.
 Figure 1: Panniculitis wound. A. Panniculitis with deep infection before surgery; B. Wound after debridement and placement of NPWTi.
Figure 1: Panniculitis wound. A. Panniculitis with deep infection before surgery; B. Wound after debridement and placement of NPWTi.
CASE STUDY #1
We present a case of a patient with severe panniculitis, refractory to treatment with antibiotics, with worsening swelling, induration, redness, and now fever (see Figure 1A). The patient required surgery for debridement due to a rapidly declining clinical status, but with a body mass index (BMI) of 80 kg/m2, he was at extremely high risk for the use of anesthesia. In addition, the patient had marked tenderness with touch to the affected area and was not likely to tolerate dressing changes while awake. Thus, he was a very good candidate for NPWTi. The considerations for using NPWTi included:
1.A high burden of devitalized tissue and infection which could benefit from wound cleansing;
2.A large wound with edema which needed to be resuscitated;
3.Repeated dressing changes would be unbearable for him and repeated anesthetics too high risk.
However, there were challenges in applying this dressing.
1.There was a large surface area to the wound with portions of the wound being much more dependent on body position (lying flat versus sitting up);
2.The surrounding skin was excoriated, weeping, and indurated;
3.The wound, after debridement, was 35 cm x 8 cm x 10 cm.
To address the unique challenges of this application, there are 2 key modifications in placing the dressing after debridement.
1.The instillation port and suction port of the V.A.C. VERAT.R.A.C. DUO™ Tube Set were supported by 2 extra layers of foam underneath to prevent blockage.
2.The V.A.C. VERAT.R.A.C. DUO™ Tube Set was used with the instillation port anterior on the wound to ensure the dependent passage of instill fluid throughout the entire wound.
3.Utilizing this dressing type on this wound bed allowed for assistance in solubilizing infectious material and wound debris, and wound cleansing without dressing changes as the patient was unable to undergo repeated episodes of anesthesia and was also very tender at the site. The wound site was continually monitored for any changes or signs of infection.
4.Instillation was evaluated for adequacy at the time of placement using the fill-assist mode on the V.A.C.ULTA™ Therapy Unit with a short-term plan of utilizing only standard negative pressure therapy and then beginning instillation the following morning. This ensured that the wound had good hemostasis before starting instillation and avoided early seal failure as consistent negative pressure can reduce the leak rate on large wounds like this one.
The dressing was placed and instillation was initiated utilizing normal saline (150 mL) with a dwell time of 10 minutes, followed by continuous negative pressure (-125 mmHg) for 3.5 hours (see Figure 1B). Normal saline was used as the patient had a gram-positive infection and no significant wound odor. In my practice, antimicrobial solutions such as 1/8 strength Dakins are reserved for gram-negative infections as saline has been proven to be effective in most wounds. The patient’s overall treatment plan included aggressive systemic antibiotics, critical care support for his respiratory failure, and septic shock, as well as nutritional supplementation through a feeding tube. After 3 days, he returned to the operating room for a repeat debridement and dressing change. At this time his overall stability had greatly improved. The dressing was replaced and another course of NPWTi given. After 1 week of therapy, the patient was able to transition to bedside dressing changes with standard V.A.C.® Therapy.
Typically, a wound of this size and contamination would require frequent explorations and dressing changes due to concern for ongoing uncontrolled infection and bioburden within the dressing itself. Instead, the patient’s infection was treated with systemic antibiotics and surgical debridement. The use of NPWTi assisted in the reduction of bacterial burden and removal of fluid from the wound without being exposed to anesthesia for these purposes, a reality that was significant for this patient with a very large wound and complex medical comorbidities.
 Figure 2. Stage IV pressure ulcer of the greater trochanter with osteomyelitis. A. Preoperative appearance of the stage IV pressure ulcer of the greater trochanter with osteomyelitis; B. Postoperative week 5 of the surgical site with completely successful primary healing. The drain was removed at week 7.
Figure 2. Stage IV pressure ulcer of the greater trochanter with osteomyelitis. A. Preoperative appearance of the stage IV pressure ulcer of the greater trochanter with osteomyelitis; B. Postoperative week 5 of the surgical site with completely successful primary healing. The drain was removed at week 7.
CASE STUDY #2
We present the case of a young man with a history of paraplegia secondary to a gunshot wound with bilateral greater trochanter stage IV pressure ulcers with osteomyelitis of the femoral head. He failed appropriate offloading, prolonged wound care, and a course of intravenous antibiotics. The patient was treated with Girdlestone pseudoarthroplasty for the removal of his femoral head and neck (see Figure 2).4 This surgery allowed for the eradication of his osteomyelitis but resulted in a large deep wound emanating from his acetabulum. The wound was highly inflamed and at risk for desiccation and non-healing. Because of this, he was a very good candidate for NPWTi with similar challenges as demonstrated in the first case, including a large space with significant edema, recent invasive infection, and the need to maintain wound tension to allow for eventual primary closure.
 Figure 3. Example of a V.A.C. VERAFLO CLEANSE CHOICETM Dressing application in a large open hip wound after Girdlestone procedure.
Figure 3. Example of a V.A.C. VERAFLO CLEANSE CHOICETM Dressing application in a large open hip wound after Girdlestone procedure.
A plan was made for placement of a V.A.C. VERAFLO CLEANSE CHOICE™ Dressing utilizing normal saline (50 mL) with a 10-minute dwell time followed by 3.5 hours of continuous negative pressure at -125 mmHg (see Figure 3). Once again, the instillation setting was held overnight and started once the hemoglobin was assessed to be stable and the dressing intact the following morning. Also, the instillation port was buttressed with additional foam to prevent blockage or obstruction. In this case, the foam cover layer can hold a very large amount of fluid when first beginning instillation and the foam is dry. A near 20% reduction in the calculated instill fluid is often required once the foam is wet to avoid over-filling the dressing.
CASE STUDY #3
A 70-year-old woman was previously involved in a high-speed motor vehicle collision and required right above-the-knee amputation after a severe degloving injury with a failed attempt at limb salvage. The patient was referred for care 7 weeks after the surgery (a total of 3 months after the initial injury). The patient’s previous medical history included obesity (BMI of 55 kg/m2). The large upper leg wound was infected and shown to have an invasive polymicrobial infection including a mold species (see Figure 4). The patient remained in the intensive care unit, critically ill with atrial fibrillation, renal failure on dialysis, and dependent on mechanical ventilation.
A multidisciplinary plan of care was created for this patient including consultation with infectious disease specialists, orthopedic surgery, and trauma surgery for removal of the devitalized tissue, revision of the amputation stump, and long-term antimicrobials. Despite appropriate treatment, the patient had progressive destruction of the tissue likely related to an invasive mold infection. Thus, several clinical applications for NPWTi are demonstrated in this case including:
 Figure 5. Application of V.A.C. VERAFLO™ Dressings over the open wound following surgical debridement.
Figure 5. Application of V.A.C. VERAFLO™ Dressings over the open wound following surgical debridement.
1.A very large wound bed with a high burden of devitalized tissue and refractory infection which could benefit from wound cleansing;
2.A large amount of edema and wound edge retraction;
3.Difficulty with adequate bedside dressing changes due to pain and wound size;
4.Multiple medical comorbidities contributing to a lack of wound healing
To address these factors the patient underwent surgical debridement followed by NPWTi with 150 mL of 1/8 strength Dakins solution. Given the large size of the wound, 2 medium sized V.A.C. VERAFLO CLEANSE CHOICE™ Dressings and a medium V.A.C. VERAFLO™ Dressing Kit were utilized (see Figure 5). To support successful instillation, the nursing staff had developed the plan for no turning of the patient during the installation phase and was updated on the likelihood of frequent canister changes. A single port was placed in the middle of the wound as the inferior portion of the wound elevation level changed based on the patient’s activity. The wound site was continually monitored for any changes or signs of infection.
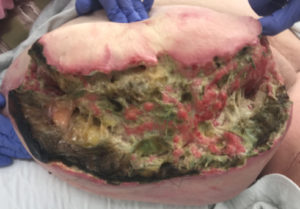 Figure 4. Open above knee amputation wound, 45 cm x10 cm x 5 cm with deep tunneling.
Figure 4. Open above knee amputation wound, 45 cm x10 cm x 5 cm with deep tunneling.
After 5 weeks of therapy, the patient was returned to the operating room with a small area of wound necrosis which was debrided. V.A.C. VERAFLO™ Therapy with V.A.C. VERAFLO CLEANSE CHOICE™ Dressings were initiated (Figure 6A). After 4 days of V.A.C. VERAFLO™ Therapy, the wound depth was reduced (8 cm x 3 cm x 2 cm) and healthy granulation tissue was noted (see Figure 6B).
 Figure 6. Above the knee wound. A. Above the knee wound with V.A.C. VERAFLO CLEANSE CHOICETM Dressing; B. Wound after 4 days of V.A.C. VERAFLOTM Therapy with V.A.C. VERAFLO CLEANSE CHOICETM Dressing.
Figure 6. Above the knee wound. A. Above the knee wound with V.A.C. VERAFLO CLEANSE CHOICETM Dressing; B. Wound after 4 days of V.A.C. VERAFLOTM Therapy with V.A.C. VERAFLO CLEANSE CHOICETM Dressing.
References
1.Lambert KV, Hayes P, McCarthy M. Vacuum assisted closure: A review of development and current applications. Eur J Vasc Endovasc Surg. 2005;29(3):219–226. https://doi.org/10.1016/j.ejvs.2004.12.017.
2.Gabriel A. Integrated negative pressure wound therapy system with volumetric automated fluid instillation in wounds at risk for compromised healing. Int Wound J. 2012;9 Suppl 1:25-31. doi: 10.1111/j.1742-481X.2012.01014.x.
3.Gabriel A, Shores J, Heinrich C, et al. Negative pressure wound therapy with instillation: A pilot study describing a new method for treating infected wounds. Int Wound J. 2008;5(3):399-413. doi: 10.1111/j.1742-481X.2007.00423.x.
4. Jain N, Horn CB, Andrade EG, Punch L. Combination of Girdlestone pseudoarthroplasty and negative pressure wound therapy with instillation and dwell in the treatment of invasive osteomyelitis of the proximal femur. Cureus. 2018;10(11):e3552. doi:10.7759/cureus.3552.



