Literature Synopsis_The Chronicles of Incision Management_2017_Volume 1_Issue 2
Literature Synopsis of Redfern, Roberta E., et al. “Closed Incision Negative Pressure Therapy Effects on Postoperative Infection and Surgical Site Complication After Total Hip and Knee Arthroplasty.” The Journal of Arthroplasty (2017).
INTRODUCTION
Total knee and hip arthroplasty, already two of the most common orthopedic procedures, are becoming increasingly prevalent. Many people who undergo these operations have comorbid diseases that increase the risk of surgical wound complications, which sometimes require revision surgeries that pose risks to health and incur added costs.
Traditionally, complicated and non-healing wounds have been treated with negative pressure wound therapy (NPWT)1,2 as a bridge between debridement and surgical closure. More recently, NPWT has also been used to manage closed wounds. In higher-risk patients (e.g., those with vascular surgeries or abdominal incisions), closed incision negative pressure therapy (ciNPT) may significantly reduce the burden of infection, postoperative hematoma, and seroma.3-7 This study sought to determine whether ciNPT would reduce wound complications in a comprehensive cohort of patients undergoing hip and knee arthroplasty.
MATERIALS AND METHODS
This single-center, open-label, non-randomized study enrolled 193 patients undergoing elective hip or knee arthroplasty in 2013-14 and treated them with ciNPT using the PREVENA™ Incision Management System (ACELITY™, San Antonio, TX) for 6-8 days postoperatively. Patients with known or suspected contraindications to this therapy were excluded. The control group—a retrospective cohort of 400 patients who underwent hip/knee arthroplasty in 2011-12—followed a standard gauze dressing protocol.
With the exception of the dressing protocol, the control and treatment groups received the same care. All patients were treated within a single institution utilizing a uniform surgical
procedure, performed by a single surgeon. Wound closure and dressing was performed by the physician assistant and not the attending surgeon. Most knees were closed with staples, while hips were typically closed with sutures and glue. External pneumatic compression cuffs were used in all cases, and incision management systems were in place for an average of 7 days. All patients followed a deep venous thrombosis (DVT) prophylaxis protocol suited to their risk level.
Patient Demographics
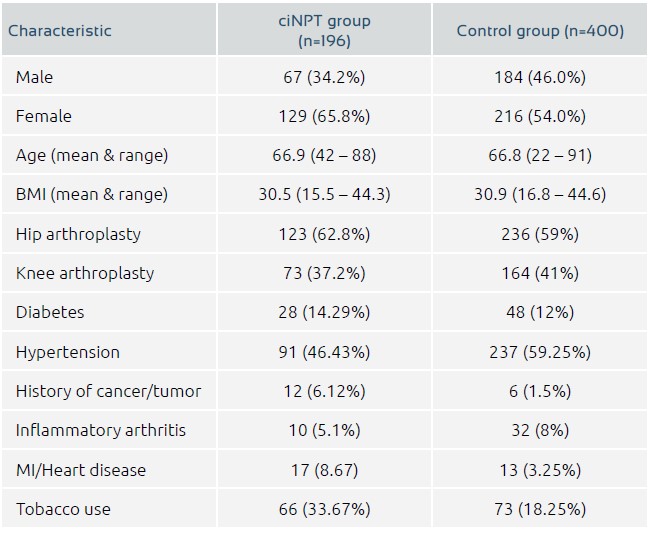
Baseline data included BMI, comorbid conditions, and surgical site (Table 1). The ciNPT group had a significantly greater proportion of females (65.8%) than the control group (54%). The ciNPT group also had a higher incidence of heart disease, tobacco use, and history of cancer, while hypertension was more prevalent in the control group.
Data on tissue appearance, edema, drainage, tape trauma, and dressing reaction were collected 24 hours after surgery and at two postoperative follow-up assessments (at 1 and 6 weeks in the treatment group and at 2 and 6 weeks in the control group). The use of postoperative anticoagulants was similar in both groups.
Statistical Analysis
The size of the cohort enabled the study to achieve 80% power with 0.05 significance level. SAS version 9.2 was used for statistical analysis. Post-hoc logistical regression was used to determine the effect of various patient characteristics on outcome measures.
RESULTS
The results of 196 incisions in 192 patients treated with ciNPT and of 400 control-group cases are reported here. The first follow-up assessment found no significant differences in skin color, swelling, drainage, infection, dehiscence, or seroma between the two study arms, although the incidence of ecchymosis was higher in the ciNPT group. At the second follow-up visit, none of these parameters (including ecchymosis) differed between the 2 groups.
Twenty-seven patients (13.7%) in the ciNPT group experienced blisters or reaction to the foam dressing, compared to 9 cases of tape trauma in the control group. Blister reactions were treated with topical antibiotics and resolved without further attention.
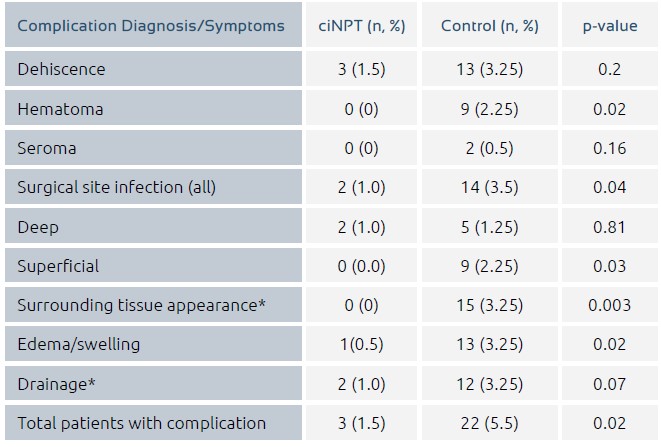
Table 2 lists the rates of clinically significant surgical site complications, defined as complications requiring surgical intervention or further physician visits. Relative to the control group, the treatment group had several favorable outcomes:
•A significantly lower rate of surgical site reaction (1.0% v 3.5%, p = 0.04)
•No hematomas requiring attention (vs. 9 in the control group)
•No seromas requiring attention (vs 2 seromas in the control group)
•Numerically lower rate of dehiscence with wound drainage (1.5% vs. 3.25%)
•Only 3 patients requiring reoperation, vs. 15 in the control group (1.5% vs. 3.75%, p = 0.14)
•In all, 3 patients with 5 complications requiring treatment (vs. 22 patients with 38 significant complications in the control group).
Complication rates were also evaluated based on surgical site of hip vs knee (p= 0.3625, OR=1.513, CI 0.620, 3.690). While infections (almost exclusively in the control group) occurred more frequently in the hip cohort, the surgical site did not affect the rates of hematoma, seroma, or dehiscence.
The post hoc logistic regression analysis did not find age, BMI, surgical site, or relevant comorbidities to impact the rate of postoperative complications. The treatment group was the only significant variable: the rate of postoperative complications was apprixmately 4 times higher in the control group than in the treatment group (OR 4.251, p = 0.0277).
DISCUSSION
These results suggest that use of ciNPT may reduce the rate of clinically significant wound complications after total hip or knee arthroplasty by more than four-fold.
Previous case series have found ciNPT to have a significant benefit in patient populations and incision types at greatest risk of skin breakdown and dehiscence. A larger study of post-sternotomy wound infections in a comprehensive patient population found that ciNPT reduced infection rates from 3.4% to 1.3%, suggesting a broader role for the technique.5The current report lends further support to this view, with the caveat that ciNPT did not significantly reduce deep surgical site reactions and may thus be unwarranted for universal use.
While more prevalent in the treatment group, dressing reactions occurred at a lower rate than reported in previous studies of total knee replacement, possibly due to the unique knit polyester covering on the PREVENA™ Incision Dressing.8-10 Of note, one report suggests that application technique (i.e., avoidance of stretching, application to a flexed knee) may also reduce blister formation.11Proposed mechanistic explanations for the benefits of NPWT include reduction of edema, stimulation of perfusion, protection from external sources of infection, stimulation of granulation tissue, and reduction of lateral tension on surgical edges.34
As one of the largest observations of NPWT in clean closed surgical incisions, this study counts sample size as a major strength. Study limitations include the use of a historical control group, dissimilarity between the two groups upon study entry, lack of blinding, differences in time to first follow-up assessment, and possible underpowering to detect differences in infection rates.
Further studies to determine whether ciNPT has more pronounced benefits in high-risk patients, as well as a health-economic analysis of routine use in hip/knee arthroscopy patients, are advised.
IMPORTANT DISCLAIMER:
Although the authors reported use of ciNPT for 6-8 days post-operatively, this time of application is outside the recommendations for Optimum Use as stated in the PREVENA™ Incision Management System Clinician Guide Instructions for Use: “The PREVENA™ Incision Management System is to be continuously applied for a minimum of two days up to a maximum of seven days.” Use for greater than 7 days is not recommended or promoted by KCI.
References
1.Stannard, James P., et al. “Incisional negative pressure wound therapy after high-risk lower extremity fractures.” Journal of orthopaedic trauma 26.1 (2012): 37-42.
2.Stannard, James P., et al. “Negative pressure wound therapy after severe open fractures: a prospective randomized study.” Journal of orthopaedic trauma 23.8 (2009): 552-557.
3.Grauhan, Onnen, et al. “Prevention of poststernotomy wound infections in obese patients by negative pressure wound therapy.” The Journal of thoracic and cardiovascular surgery 145.5 (2013): 1387-1392.
4.Grauhan, Onnen, et al. “Effect of surgical incision management on wound infections in a poststernotomy patient population.” International wound journal 11.s1 (2014): 6-9.
5.Weir, Gregory. “The use of a surgical incision management system on vascular surgery incisions: a pilot study.” International wound journal 11.s1 (2014): 10-12.
6.Pachowsky, Milena, et al. “Negative pressure wound therapy to prevent seromas and treat surgical incisions after total hip arthroplasty.” International orthopaedics 36.4 (2012): 719-722.
7.Atkins, Broadus Zane, et al. “Does negative pressure wound therapy have a role in preventing poststernotomy wound complications?” Surgical innovation 16.2 (2009): 140-146.
8.Howell RD et al. Blister formation with negative pressure dressings after total knee arthroplasty. Current Orthopedic Practice 2011;22:176.
9.Gomoll, Andreas H., Albert Lin, and Mitchel B. Harris. “Incisional vacuum-assisted closure therapy.” Journal of orthopaedic trauma 20.
10 (2006): 705-709. 10.Koval, Kenneth J., et al. “Tape blisters after hip surgery: can they be eliminated completely?” AMERICAN JOURNAL OF ORTHOPEDICS-BELLE MEAD- 36.5 (2007): 261.
11.Karlakki, S. L., et al. “Incisional negative pressure wound therapy dressings (inpWTd) in routine primary hip and knee arthroplasties.” Bone and Joint Research 5.8 (2016): 328-337.
12.Dohmen, Pascal M., et al. “Can post-sternotomy mediastinitis be prevented by a closed incision management system?” GMS hygiene and infection control 9.3 (2014).