Dr. Fernandez is a Clinical Assistant Professor of Surgery and Family Practice at the University of Texas Health Center at Tyler. He is also an Attending Teaching Staff in the Division of Surgery for Mother Frances Health System and East Texas Medical Center in Tyler. Dr. Fernandez obtained his residency training at Loyola University, the University of Illinois, the University of Chicago and Northwestern University, Chicago, Illinois, with special training in Trauma and Burns at Kings County Hospital, SUNY Down State System, Brooklyn, New York, NY. He is well published in multiple areas of research both in peer-reviewed articles and book chapters, and has made numerous oral and poster presentations at national and international conferences.
Fernandez_Innovations in Addressing Non-Viable Tissue_2018_Volume 1_Issue 1
INTRODUCTION
Negative pressure wound therapy (NPWT) is an advanced wound care therapy commonly used in chronic and complex wounds. Historically, standard NPWT has been associated with higher-cost advanced wound care therapies; however, several studies have shown an overall savings in direct and indirect costs, in a large part due to decreases in operating room (OR) visits, early wound closure in many treated patients, reduced hospital stay, less required dressing changes (with resultant lower material/manpower cost and care delivery efficiency), as well as improved limb preservation rates.1-7 Over the years, NPWT has evolved to include the ability to instill topical wound solutions, which are allowed to dwell directly onto the open wound.8-10A growing body of literature supports the use of NPWT with instillation and dwell time (NPWTi-d; V.A.C. VERAFLO™ Therapy) with positive clinical outcomes and potential cost savings being reported.
Recommendations exist in the literature for the use of NPWTi-d in acute and chronic wounds.8-10Several dressings for use with NPWTi-d have been developed, among them a reticulated open cell foam dressing with through holes (ROCF-CC; V.A.C. VERAFLO CLEANSE CHOICE™ Dressing) that assists in removing thick wound exudate and infectious materials.16 ROCF-CC is useful for wound cleansing when debridement is not possible or appropriate, particularly in high operative risk patients. Here, we report our early experience on the use of NPWTi-d with ROCF-CC in the following cases of complex wounds.
CASE STUDIES
Case 1
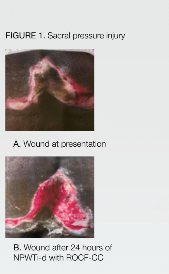
A 72-year-old male, with a history of essential hypertension, cerebrovascular accident, and moderate to severe malnutrition, presented with an unstageable sacral pressure injury. The wound at presentation measured 15.0 cm x 11.0 cm with >60% adherent nonviable tissue on the wound surface (Figure 1A). After 24 hours of ROCF-CC; V.A.C. VERAFLO CLEANSE CHOICE™ Dressing NPWTi-d (70cc hypochlorous solution with a 10-minute dwell time, followed by 3 hours of NPWT at -125 mmHg), the wound surface filled with >90% viable tissue (Figure 1B). After noting the results, the patient was transitioned to standard NPWT and discharged to a long-term acute care (LTAC) hospital.
Case 2
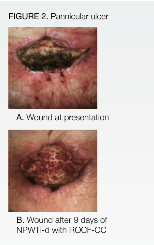
A 59-year-old female, with medical history of obesity, diabetes mellitus, and previous stomach stapling, presented with panniculitis and a grade 3 panniculus ulcer. The ulcer measured 4cm x 8.5cm x 3cm with 80% devitalized tissue and foul-smelling, purulent discharge (Figure 2A). After 9 days of ROCF-CC; V.A.C. VERAFLO CLEANSE CHOICE™ Dressing NPWTi-d (38 mL hypochlorous solution with a 10-minute dwell time, followed by 2 hours of NPWT at -125 mmHg), the wound displayed >90% viable tissue (Figure 2B). The dressing changes were done at 48 to 72-hour intervals. The patient was transitioned to standard NPWT and discharged to a skilled nursing facility the same day NPWT was initiated.
DISCUSSION
Based on our initial experience, the ROCF-CC dressing demonstrated unique properties that allowed effective and rapid removal of thick exudates in large complex wounds that contained substantial areas of devitalized tissue. We also observed that NPWTi-d with ROCF promoted excellent development of underlying granulation tissue. In the two cases presented, the dressing was used safely in severely debilitated as well as frail patients.
The term “frailty” has become more commonly used in the medical and surgical literature to describe a multifactorial state of general physical weakness, often under recognized patient vulnerability and decreased physiologic reserve. Perioperative risk is heterogeneous in this group, and age and comorbidities, in and of themselves, fail to predict functional deficits and cannot adequately predict operative and perioperative morbidity and mortality in this population group.17-24 In a recent systematic study, it was noted “in patients over 75 years of age, frailty has been found to increase post-operative complications; prolonged length of stay; 30-day mortality and discharge to long term care facility” (eg, long-term acute care hospital and/or skilled nursing facility). These findings were noted, “irrespective of the type of surgery conducted “and were found to be consistent across different frailty measurement techniques. The majority of the current literature investigating frailty and surgery has defined ‘geriatric’ as those above 60 or 65 years old. Studies in this patient population have recognized frailty being more prevalent with increasing age. A recent systematic review incorporating 31 studies of frailty in persons 65 years or older found a prevalence of from 4.0% to 17.0% (mean 9.9%) of physical frailty, with a higher prevalence when psychosocial frailty was also included. 25,26 Thus, in our two cases, NPWTi-d was chosen for therapy, as these patients were not candidates for surgical debridement due to their underlying comorbidities contributing to their perceived frailty risk.
It is interesting to note that the use of NPWTi-d with ROCF-CC may potentially decrease cost of care by assisting in bedside wound cleansing and reducing the need for debridement in the OR. However, further study is warranted in the use of this novel treatment modality to determine the clinical benefits and its cost effectiveness in wound care. This will help to more clearly define and inform best evidence-based practice guidelines for its clinical application in the case of patients with complex chronic wounds.
References
1.Moues CM, Van Den Bemd GJ, Meerding WJ, Hovius SE. An economic evaluation of the use of TNP on full-thickness wounds. J Wound Care 2005;14:224-227.
2.Sinha S, Mudge E. The national health-care agenda in relation to negative pressure wound therapy. British Journal of Community Nursing 2013;Suppl:S6, S8, S10-S13.
3.Kaplan M, Daly D, Stemkowski S. Early intervention of negative pressure wound therapy utilizing vacuum assisted closure in trauma patients: impact on hospital length of stay and cost. Adv Skin Wound Care 2009; 22:128-132.
4.Dowsett C, Davis L, Henderson V, Searle R. The economic benefits of negative pressure wound therapy in community-based wound care in the NHS. Int Wound J2012; 9:544-552.
5.Le Franc B, Sellal O, Grimandi G, Duteille F. [Cost-effectiveness analysis of vacuum-assisted closure in the surgical wound bed preparation of soft tissue injuries]. Ann Chir Plast Esthet 2010;55:195-203.
6.Apelqvist J, Armstrong DG, Lavery LA, Boulton AJ. Resource utilization and economic costs of care based on a randomized trial of vacuum-assisted closure therapy in the treatment of diabetic foot wounds. Am J Surg2008; 195:782-788
7.Driver VR, Blume PA. Evaluation of Wound Care and Health-Care Use Costs in Patients with Diabetic Foot Ulcers Treated with Negative Pressure Wound Therapy versus Advanced Moist Wound Therapy. J Am Podiatr Med Assoc 2014; 104:147-153.
8.Kim PJ, Attinger CE, Crist BD et al. Negative pressure wound therapy with instillation: review of evidence and recommendations. Wounds 2015;27:S2-S19.
9.McKanna M, Geraci J, Hall K et al. Clinician panel recommendations for use of negative pressure wound therapy with instillation. Ostomy Wound Manage 2016; 3-14.
10.Gupta S, Gabriel A, Lantis J, Teot L. Clinical recommendations and practical guide for negative pressure wound therapy with instillation. Int Wound J2016;13:159-174.
11.Kim PJ, Attinger CE, Steinberg JS et al. The impact of negative-pressure wound therapy with instillation compared with standard negative-pressure wound therapy: a retrospective, historical, cohort, controlled study. Plast Reconstr Surg 2014; 133:709-716.
12.Gabriel A, Kahn K, Karmy-Jones R. Use of negative pressure wound therapy with automated, volumetric instillation for the treatment of extremity and trunk wounds: clinical outcomes and potential cost-effectiveness. Eplasty 2014; 14:e41.
13.Brinkert D, Ali M, Naud M, Maire N, Trial C, Teot L. Negative pressure wound therapy with saline instillation: 131 patient case series. Int Wound J 2013; 10:56-60.
14.Fluieraru S, Bekara F, Naud M et al. Sterile-water negative pressure instillation therapy for complex wounds and NPWT failures. J Wound Care 2013; 22:293-299.
15.Wolvos T. The use of negative pressure wound therapy with an automated, volumetric fluid administration: An advancement in wound care. Wounds 2013; 25:75-83.
16.Teot L, Boissiere F, Fluieraru S. Novel foam dressing using negative pressure wound therapy with instillation to remove thick exudate. Int Wound J 2017; 14(5):842-848.
17.Ravaglia G, Forti P, Lucicesare A, et al. Development of an easy prognostic score for frailty outcomes in the aged. Age Ageing 2008; 37(2):161–6.
18.Institute of Medicine (US) Committee on the Future Health Care Workforce for Older Americans. Retooling for an aging America: building the health care workforce. Washington, D.C.: National Academies Press (US), 2008.
19.Bettelli G. Anaesthesia for the elderly outpatient: preoperative assessment and evaluation, anaesthetic technique and postoperative pain management. Curr Opin Anaesthesiol 2010; 23(6):726–31.
20.Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): Developed in Collaboration With the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation 2007; 116(17):1971–96.
21.Deiner S, Silverstein JH. Anesthesia for geriatric patients. Minerva Anestesiol 2011; 77(2):180–9.
22.El-Haddawi F, Abu-Zidan FM, Jones W. Factors affecting surgical outcome in the elderly at Auckland Hospital. ANZ J Surg 2002; 72(8):537–41.
23.Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg 2010; 210(6):901–8.
24.Walston J, Hadley EC, Ferrucci L, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc2006 Jun; 54(6):991-1001.
25.Lin H-S, Watts JN, Peel NM, Hubbard RE. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatrics 2016; 16(1):157.
26.(26)Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: A systematic review. J Am Geriatr Soc. 2012;60:1487–1492. [PubMed]