Center for Wound Healing and Hyperbaric MedicineDepartment of Plastic and Reconstructive SurgeryMedStar Georgetown University Hospital
Thalia Attinger is a family nurse practitioner, board certified by the American Nurses Credentialing Center. She obtained her Bachelor of Arts as well as Bachelor in Science and Master of Science dergrees from Georgetown University in Washington, DC. Prior to joining the Center for Wound Healing and Hyperbaric Medicine she spent over five years working in the Medical Intensive Care Unit at MGUH. She hopes to provide her patients and their families with a sense of control and responsibility by encouraging them to become active participant in their care and to create an environment that promotes physical and emotional healing.

Associate ProfessorDirector of ResearchCenter for Wound Healing and Hyperbaric MedicineDepartment of Plastic and Reconstructive SurgeryMedStar Georgetown University Hospital
Paul J. Kim is the Director of Research and holds the rank of Associate Professor at Georgetown University School of Medicine and is a Senior Faculty in the Department of Plastic Surgery at Georgetown University Hospital. He is also a Fellow of the American College of Foot and Ankle Surgeons.
Kim and Attinger_Innovations in Addressing Non-Viable Tissue_2018_Volume 1_Issue 1
INTRODUCTION
Negative pressure wound therapy (NPWT) with instillation and a dwell time (NPWTi-d) combines the benefits of traditional negative pressure with intermittent dwelling of a topical wound solution. This adjunctive therapy has been shown to improve outcomes for complex patients with infected or contaminated wounds.1-3 At our institution, we have demonstrated that NPWTi-d can result in greater efficiency and effectiveness to prepare a wound for closure or coverage as compared with traditional NPWT (Kim, Attinger et al. 2014, Kim, Attinger et al. 2015).4,5However, our use of NPWTi-d had been used solely in conjunction with surgical excisional debridement. Our assumption had been that sharp debridement is absolutely necessary to remove nonviable tissue because NPWTi-d is not indicated for this action. With the advent of the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing, this dressing may provide an additional wound cleansing option when surgical debridement is not possible or appropriate.
There is a subpopulation of wound patients who are not candidates for excisional debridement and therefore cannot undergo either surgical or bedside debridement. The patient may be too high risk (due to comorbidities) for surgical debridement; the patient cannot tolerate sharp debridement at bedside; there may not be a surgeon available to perform excisional debridement; or there may be a lack of regular or prescheduled access to the operating room. In many cases, decubitus ulcers are managed exclusively by nurses or other healthcare providers who may be prohibited by state licensing or hospital regulations from performing sharp debridement. Therefore, default daily or twice daily dressing changes utilizing wet-to-wet or wet-to dry dressing changes with a variety of solutions are performed. Dressing changes in this manner are highly inefficient and are resource intensive, consuming hours of work and in many occasions multiple individuals. This method would be acceptable if it clearly demonstrated good outcomes. However, there is no evidence for this technique being effective.
In such an environment, the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing may be a viable answer. We present our first two patients who received V.A.C. VERAFLO™ Therapy using the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing for the primary management of sacral ulcers.
PATIENT #1
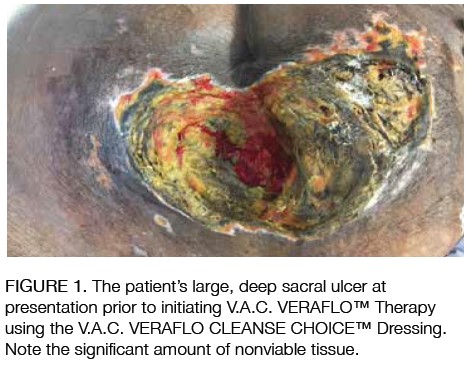
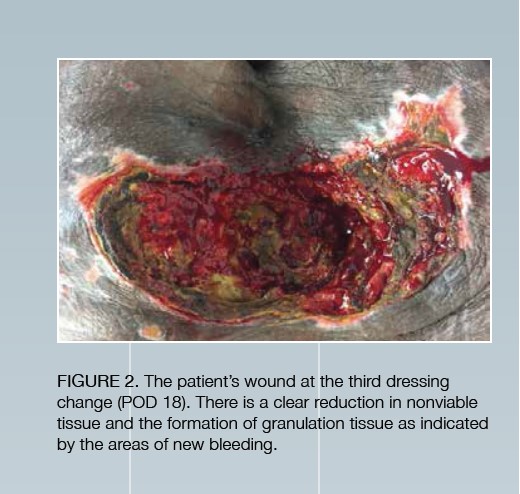
A morbidly obese 54-year-old male with a BMI of 45 and a past medical history of Type 2 diabetes, hypertension and bilateral lower extremity nonhealing wounds was admitted for multiple bowel perforations requiring small bowel resection at 3 sites, acute kidney injury, and klebsiella Pneumonia bacteremia. Postoperatively, the patient was on multiple vasopressors and started on a 2-month course of antibiotics. He suffered from persistent anastomotic leaks with frank stool coming from the Jackson-Pratt drains, which persisted despite multiple revisions. Complications persisted with hernias, bowel obstructions and further perforations. This all resulted in a very large controlled enterocutaneous fistula, with NPWT and multiple drains putting out bile-stained fluid. As a result, the patient was on vasopressors and continuous veno-venous hemofiltration on and off throughout his stay. He required almost daily blood transfusions. Due to worsening of the lungs (pleural effusion layering, atelectasis vs pneumonia) he was placed on the ventilator for the majority of his hospitalization. Over the next 5 days, the patient began to drain increasing fluid from the left flank pressure ulcer, which was then sharply debrided and packed. One week into his hospitalization, the nurses noted a Stage IV, 12x10cm sacral ulcer with extensive necrotic tissue, no pus or erythema, no deeper fluid pockets, and no bleeding, which was subsequently managed with betadine paint and acetic acid and shifting the position of the patient when possible. The patient then received V.A.C. VERAFLO™ Therapy with the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing on this wound with 3 dressing changes (Figure 1, 2). The solution instilled was normal saline with a dwell time of 20 minutes, followed by 2 hours of negative pressure (-125 mmHg). The patient was eventually discharged to a long term acute care facility on standard NPWT.
PATIENT #2
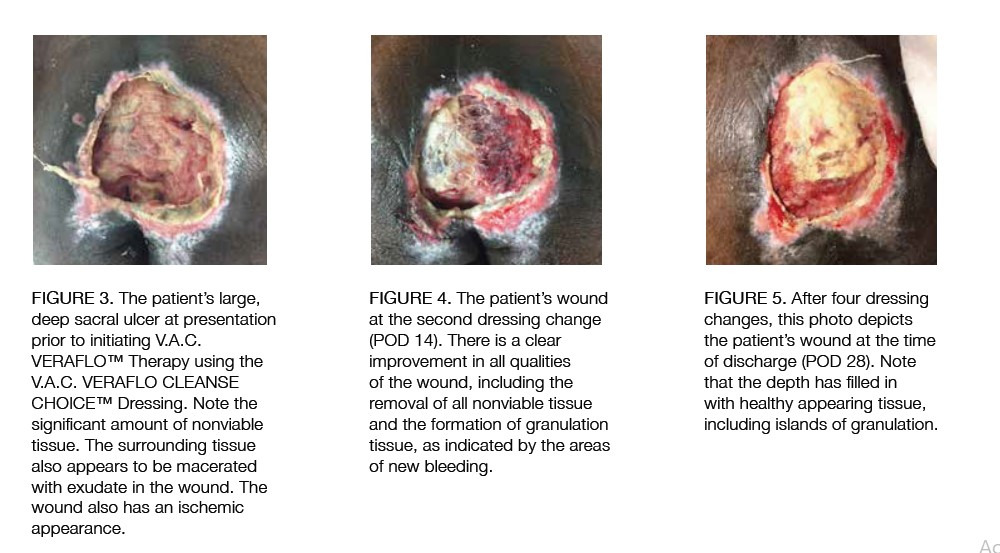
This patient was a male with a history of Type 2 diabetes, hypertension, coronary artery disease, atrial fibrillation, cerebral vascular accident with residual right-sided weakness, chronic obstructive pulmonary disease, mild pulmonary hypertension and congestive heart failure ejection fraction of 40-45%. He also had a complicated history of prior retrocolic Billroth II for peptic ulcer with intraoperative course complicated by cardiac arrest and postoperative course complicated by duodenal stump leak and bleeding from transverse colon status post exploratory laparotomy, and placement of multiple drains and total parenteral nutrition. This patient presented with tachycardia concerning for sepsis following a recent protracted hospital course for abdominal pain. This was complicated by atrial fibrillation rapid ventricular rate status post diltiazem drips, pneumoperitoneum and volume overload caused by duodenal stump leak status postoperative re-exploration and abdominal washout with placement of multiple drains and duodenostomy tube, as well as pulmonary embolism. This hospital admission was complicated by episodes of atrial fibrillation with rapid ventricular rate, acute hypoxic respiratory failure, as well as sacral decubitus ulcers with polymicrobial infection (acinetobacter, methicillin resistant Staphylococcus Aureus, gram negative rods, Pseudomonas), as well as progressive altered mental status in the context of worsening oliguric/anuric renal failure. On initial evaluation, he was noted to have increased drainage from his abdominal Jackson-Pratt drain; however, computerized tomography imaging revealed no new? intraabdominal collections. The same imaging did reveal extensive area of soft tissue fluid collection, stranding with bubbles of gas straddling the midline, posterior and inferior to the coccyx with concern for Stage IV sacral decubital ulcer infection and osteomyelitis of the coccyx. The patient received wet-to-dry dressings twice daily until we initiated V.A.C. VERAFLO™ Therapy using the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing for 4 weeks (Figure 3-5). The solution instilled was normal saline with a dwell time of 20 minutes, followed by 2 hours of negative pressure (-125 mmHg). The patient was eventually discharged to a long term acute care facility on standard NPWT.
DISCUSSION
We present our first 2 patients who received V.A.C. VERAFLO™ Therapy using V.A.C. VERAFLO CLEANSE CHOICE™ Dressings. Both patients were very sick with a multitude of comorbidities, including poor nutritional and healing potential. Both patients received no excisional debridement throughout their treatment. It was clear to us that the wounds showed significant reduction of nonviable tissue over the weeks of treatment. In our institution, these were ideal candidates for using the novel foam construct with instillation therapy. Although we have a surgical bias, some patients we encounter are not surgical candidates. However, even in our institution, this novel foam may have a role in those patients in which operative debridement is not possible or appropriate and may be able to advance the wound efficiently to closure or coverage.
There is still a need to examine this foam dressing within the confines of a robust study. Currently, there is only one case series that demonstrates its utility (Teot, Boissiere et al. 2017). We believe this dressing has a role and may expand the uses for NPWTi-d to include more complex hosts and complex wounds that for one reason or another cannot be excisionally debrided. It is important to understand that the foam dressing should be used in concert with the V.A.C. VERAFLO™ Therapy System. The topical solution provides a medium for softening and hydrating the nonviable tissue and the foam facilitates the removal under negative pressure of thick wound exudates and other infectious materials.
References
1.Timmers MS, Graafland N, Bernards AT, Nelissen RG, van Dissel JT, Jukema GN. Negative pressure wound treatment with polyvinyl alcohol foam and polyhexanide antiseptic solution instillation in posttraumatic osteomyelitis. Wound Repair Regen 2009; 17:278-286.
2.Brinkert D, Ali M, Naud M, Maire N, Trial C, Teot L. Negative pressure wound therapy with saline instillation: 131 patient case series. Int Wound J 2013; 10:56-60.
3.Gabriel A, Kahn K, Karmy-Jones R. Use of negative pressure wound therapy with automated, volumetric instillation for the treatment of extremity and trunk wounds: clinical outcomes and potential cost-effectiveness. Eplasty 2014; 14:e41.THALIA ATTINGER, NPCenter for Wound Healing and Hyperbaric MedicineDepartment of Plastic and Reconstructive SurgeryMedStar Georgetown University HospitalThalia Attinger is a family nurse practitioner, board certified by the American Nurses Credentialing Center. She obtained her Bachelor of Arts as well as Bachelor in Science and Master of Science dergrees from Georgetown University in Washington, DC. Prior to joining the Center for Wound Healing and Hyperbaric Medicine she spent over five years working in the Medical Intensive Care Unit at MGUH. She hopes to provide her patients and their families with a sense of control and responsibility by encouraging them to become active participant in their care and to create an environment that promotes physical and emotional healing. Corresponding AuthorPAUL J. KIM, DPM, MSAssociate ProfessorDirector of ResearchCenter for Wound Healing and Hyperbaric MedicineDepartment of Plastic and Reconstructive SurgeryMedStar Georgetown University HospitalPaul J. Kim is the Director of Research and holds the rank of Associate Professor at Georgetown University School of Medicine and is a Senior Faculty in the Department of Plastic Surgery at Georgetown University Hospital. He is also a Fellow of the American College of Foot and Ankle Surgeons.
4.Kim PJ, Attinger CE, Steinberg JS et al. The impact of negative-pressure wound therapy with instillation compared with standard negative-pressure wound therapy: a retrospective, historical, cohort, controlled study. Plast Reconstr Surg 2014; 133:709-716.
5.Kim PJ, Attinger CE, Oliver N et al. Comparison of Outcomes for Normal Saline and an Antiseptic Solution for Negative-Pressure Wound Therapy with Instillation. Plast Reconstr Surg 2015; 136:657e-664e.