
Dr. Regina Fearmonti is a microvascular fellowship-trained plastic and reconstructive surgeon with a background as a breast surgical oncologist. She is board certified through the American Board of Plastic Surgery and the American Board of Surgery. She practices through Alon Aesthetics Plastic Surgery in San Antonio and New Braunfels. With privileges in hospitals throughout New Braunfels and San Antonio’s South Texas Medical Center, she has been serving patients in South Texas since September 2012. She is medical director of SKIN Alon and Restore Men’s Health, specializing in laser and radiofrequency skin rejuvenation, toxins, fillers, and allograft as well as PRP and adipose-derived injections for skin repair and hair regeneration.
She received her undergraduate degree from Northwestern University and her medical degree from Loyola University-Chicago, Stritch School of Medicine. She completed her training in general surgery at the distinguished Baylor College of Medicine and fellowship training in breast surgical oncology at The University of Texas M.D. Anderson Cancer Center, followed by a second residency at Duke University in plastic and reconstructive surgery. She then returned home to Texas and The University of Texas M.D. Anderson Cancer Center to complete a year-long fellowship in reconstructive microsurgery.
Dr. Fearmonti has trained with leading plastic surgeons from around the country, and she is an active member of the American Society of Plastic Surgeons, American Society for Aesthetic Plastic Surgery, Texas Society of Plastic Surgeons, is president of the San Antonio International Society of Plastic Surgeons, and she serves on the editorial board of the Plastic Surgery Education Network. Dr Fearmonti is a consultant for 3M.
Fearmonti_Current Dialogues in Wound Management_2020_Article_9
BACKGROUND
The number of women undergoing immediate implant-based breast reconstruction following mastectomy has increased in the United States over the past decades.1 With that, prepectoral reconstruction has been revisited as an alternative to a subpectoral, or dual-plane approach.2 Prepectoral implant placement decreases postoperative pain from pectoralis muscle spasm, prevents animation deformity, and preserves pectoralis strength.3 Challenges to a successful reconstruction remain patient selection as well as intraoperative considerations, such as mastectomy flap vascularity and need to resect skin or the nipple-areolar complex (NAC). Poor perfusion or need for skin removal may support placement of a tissue expander filled with room air or saline for a 2-stage reconstruction. Optimal conditions may facilitate immediate placement of a breast implant in the prepectoral plane at time of mastectomy for a 1-stage, or direct-to-implant (DTI) reconstruction.4
Postoperative care and minimizing incision complications impact both surgical and aesthetic outcomes. An ideal postoperative dressing following DTI reconstruction would offload mastectomy skin flaps, provide soft tissue support and stabilization, manage edema, limit shear forces, allow placement of drains, provide patient comfort, and provide protection from external contaminants. We describe the use of PREVENA RESTOR BELLA•FORM™ Incision Management System for use as a postoperative dressing for prepectoral DTI breast reconstruction.
Case Study
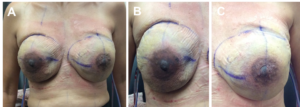
A 45-year-old female was diagnosed with suspicious microcalcifications in her left breast on her annual screening mammogram. She had undergone screening mammograms since the age of 35 due to a family history of breast cancer yet denied prior abnormalities or breast biopsy. A stereotactic core biopsy confirmed multifocal left breast ductal carcinoma in situ with concomitant lobular carcinoma in situ and atypical ductal hyperplasia. Genetic testing ruled out a deleterious mutation. The physical exam revealed a body mass index of 22.9 kg/m2 and the breast exam revealed dense fibrocystic breasts with no palpable masses, lymphadenopathy, or skin changes. She demonstrated bilateral grade II Regnault ptosis, base diameters of 13 cm, notch-nipple distances of 28 cm, and nipple-inframammary fold distances of 10 cm (Figure 1).

The patient opted for bilateral skin-sparing mastectomy and desired an immediate silicone implant-based reconstruction in a prepectoral plane. After discussion with the oncologic surgeon, it was confirmed that NACs could be preserved if the intraoperative core biopsy was negative. She was consented for bilateral immediate silicone implant versus tissue expander placement in the prepectoral plane, use of acellular dermal matrix (ADM), intraoperative fluorescent angiography, and placement of the PREVENA RESTOR BELLA•FORM™ System.
Bilateral skin and NAC-preserving mastectomies were performed via inframammary fold incisions, and fluorescent angiography confirmed adequate skin flap perfusion with sizers in place. The ADM was draped around the anterior aspect of the implant with a peripheral cuff and sewn into the mastectomy pocket. Bilateral 490 cc smooth round extra high-profile cohesive silicone implants were then placed in the prepectoral plane. A #19 French and #15 French Jackson-Pratt® drain (Cardinal Health™; Waukegan, Illinois) were placed in each mastectomy pocket (Figure 2).

The wound was closed in layers, and a PREVENA RESTOR BELLA•FORM™ Dressing was placed on each breast, oriented to include inframammary fold incisions and NACs, avoid overlap, and to exclude the drain exit sites. The breast skin was window-paned with a plastic drape at sites where the hydrocolloid adhesive contacted the skin to minimize shear forces. The preserved NACs were lifted and centered on the breast mounds to adjust for preoperative ptosis. The PREVENA RESTOR BELLA•FORM™ System was assembled per the package insert. Continuous negative pressure was administered at -125 mmHg, and the patient was discharged home with the device in place (Figures 3 and 4).


The patient was seen on postoperative day 6 and the PREVENA RESTOR BELLA•FORM™ System was removed. The patient’s incisions remained intact and mastectomy skin flaps and nipple-areolar complexes demonstrated no evidence of congestion or epidermolysis (Figure 5). Pathology results indicated no need for adjuvant treatment. The patient went on to heal uneventfully with follow-up at 191 days (Figure 6).

Discussion
In this case study, the PREVENA RESTOR BELLA•FORM™ System was used as a postoperative dressing following prepectoral DTI breast reconstruction. No skin or incisional complications occurred and the PREVENA RESTOR BELLA•FORM™ System was well tolerated by the patient. Positioning of the NAC prior to the dressing placement also aided in the correction of preoperative ptosis. The patient’s incisions remained closed and no surgical revision was necessary.
Postoperative dressing selection is as variable as surgical technique. In prepectoral reconstruction, erythema, blistering skin or epidermolysis, skin necrosis, or drainage require immediate intervention and may lead to loss of the implant, as there is minimal soft tissue coverage. In prepectoral DTI reconstruction, my postoperative protocol asks patients to limit arm abduction and extension for 6 weeks to minimize disruption of the incision edges and to allow the ADM to incorporate. Surgical bras, Steri-Strips™, occlusive and semi-occlusive antimicrobial dressings, Tegaderm™ and Ioban™ are options to protect the integrity of the incision, though none address the surrounding mastectomy skin or NAC. Closed incision negative pressure therapy may lead to decreased seroma formation5 and it has shown benefit in reducing the incidence of mastectomy skin flap necrosis and overall complications in immediate expander-based breast reconstruction.6 ciNPT also manages the environment of the closed incision by helping to hold the incision edges together, prevents external contamination, reduces edema, and removes infectious materials. Expanding the benefits of negative pressure beyond the incision may serve to stabilize the mastectomy envelope. The NAC, especially when an intraoperative core biopsy is performed, has a tenuous blood supply and additional offloading of tensile forces may assist in its recovery and maintenance of its position (Figure 6).
Conclusion
Closed incision negative pressure therapy with an expanded coverage area as afforded by the PREVENA RESTOR BELLA•FORM™ System effectively managed breast incisions and surrounding soft tissue in this patient. The PREVENA RESTOR BELLA•FORM™ System is an effective postoperative dressing option for these challenging reconstructive patients that may enhance patient comfort and aesthetic satisfaction.
Patient data and photos courtesy of Dr. Regina M. Fearmonti.
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
NOTE: Specific indications, contraindications, warnings, precautions and safety information may exist for these products. Please consult a healthcare provider and product instructions for use prior to application. Rx only.
References
- Albornoz CR, Bach PB, Mehrara BJ et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg 2013;131(1):15-23. doi:10.1097/PRS.0b013e3182729cde.
- Woo A, Harless C, Jacobson SR. Revisiting an Old Place: Single-Surgeon Experience on Post-Mastectomy Subcutaneous Implant-Based Breast Reconstruction. Breast Journal 2017;23(5):545-553. doi:10.1111/tbj.12790.
- Nahabedian MY. Current Approaches to Prepectoral Breast Reconstruction. Plast Reconstr Surg 2018;142(4):871-880. doi:10.1097/PRS.0000000000004802.
- Sbitany H, Lee KR. Optimizing Outcomes in 2-Stage Prepectoral Breast Reconstruction Utilizing Round Form-Stable Implants. Plast Reconstr Surg 2019;144(1S Utilizing a Spectrum of Cohesive Implants in Aesthetic and Reconstructive Breast Surgery):43S-50S. doi:10.1097/PRS.0000000000005949.
- Gabriel A, Sigalove SR, Maxwell GP. Initial Experience Using Closed Incision Negative Pressure Therapy after Immediate Postmastectomy Breast Reconstruction. Plastic and Reconstructive Surgery Global Open 2016;4(7):e819. doi:10.1097/GOX.0000000000000803.
- Kim DY, Park SJ, Bang SI, Mun GH, Pyon JK. Does the Use of Incisional Negative-Pressure Wound Therapy Prevent Mastectomy Flap Necrosis in Immediate Expander-Based Breast Reconstruction? Plast Reconstr Surg 2016;138(3):558-566. doi:10.1097/PRS.0000000000002431.
©2020 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. PRA-PM-US-02476 (07/20).

