
Janis Harrison is a Wound, Ostomy, Continence Nurse and Certified Foot Care Nurse that practices under contracts across Northeast Nebraska.
Janis believes strongly that her continuous research, study, and stress on patient education are what have led her to maintaining a reputation of providing leading edge wound care in a rural setting. As a RN,BSN,CWOCN, CFCN Janis has focused on best practices and new product research. Her posters are regularly displayed at WOCN Society and SAWC conventions. Janis trained at the National Hansen’s Disease Clinical Center and her passion has become combining the use of casting practices in conjunction with the latest wound care dressings and best practices. Janis holds a bachelor’s degree, summa cum laude, in nursing from Morningside College of Sioux City, Iowa. She received her wound, ostomy, and continence training through the WEBwoc on-line program. Her foot and nail care training were completed through an accredited WOCNCB program in Eau Claire, Wisconsin. Janis’ dedication to rural wound care was inspired at a time when her ostomate husband underwent 12 surgeries and no CWOCN services were available in Northeast Nebraska.
Harrison_Current-Dialogues-in-Wound-Management_2019_Article_5
BACKGROUND
The need to continuously improve wound dressings to improve healing time while reducing dressing changes has been a constant in the world of wound care. The wound care clinician strives to find those dressings which provide:
- Better Clinical Outcomes such as improved healing time and reduction of wound complications.1
- Reduced Costs such as wound dressings that require less time spent on application.1
- Increased Patient Comfort such as dressings that are gentler on periwound skin and correctly sized for the wound. Properly dressed wounds require less frequent dressing changes, reduce the risk of complications, and may allow the patient to perform daily physical activities without irritation.1
Adhesive Drapes can be an effective means of protection for incontinent patients, for wounds that are vulnerable to abrasion, and in conjunction with negative pressure wound therapy. In this article, I present the use of the DERMATAC™ Drape which was trialed on four individual patients with the clinical goal(s) of:
- Reducing Medical Adhesive Related Skin Injuries (MARSI), defined as erythema and/or other manifestation of cutaneous abnormality (including, vesicle, bulla, erosion, or tear) is present 30 minutes or more after removal of the adhesive.2
- Reducing patient pain caused by dressing changes
- Increasing wear time until 72 hours when used on wounds in contact with abnormally high activity and abrasive environments
- Providing greater flexibility when applied to areas requiring greater conformity to angular wound terrain.
REPRESENTATIVE CASE STUDIES
Case 1
A 48-year-old female presented with a Stage 4 sacral pressure injury of greater than 2 months. Her medical history includes dyskinesia, severe mental disability, aphasia and some akinesia. The patient lives in a group home and is in a wheelchair most of the day. Previous treatments included wet-to-dry gauze for 3 weeks followed by a regimen of absorptive foam for 2 weeks. The patient was referred for surgery to have full surgical debridement of the wound to remove all eschar and slough. The ACTIV.A.C.™ Therapy System was initiated in the surgical suite and within 2 weeks of therapy, progress was noted in the wound. However, there was noted irritation from the traditional drape applied around the V.A.C.® SIMPLACE™ Dressing, with dressing changes every 2-3 days. The patient cried and was in constant motion as the dressing was removed. This patient was unable to communicate her pain, so we used the Wong-Baker FACES Pain Rating Scale for determining pain and arrived at an 8-10 rating (Figure 1).

We chose this patient as a candidate for the new DERMATAC™ Drape in hopes to improving patient comfort during dressing changes. The patient’s skin improved in the week that we trialed the DERMATAC™ Drape. However, due to constant uncontrollable movement, the edges of the dressing rolled. After 2 weeks an attempt to close the wound with sutures was made. This patient was nutritionally compromised due to her constant movement, resulting in poor wound healing. Two weeks after attempted surgical wound closure, the suture line dehisced and the patient was left with an open wound that measured 1.8 x 1.5 x 1.7-cm3. This patient was admitted to the hospital for bedrest and placed on an air fluidized bed. Therapy was changed to wet-to-dry (Dakins 0.125% solution) gauze dressings held in place with mesh panties or Montgomery straps. For this patient, the DERMATAC™ Drape provided a positive outcome for less MARSI and reduced pain during dressing changes. However, due to the patient’s constant movement, further intervention was required.
Case 2
A 52-year-old male presented with a Stage 3 right trochanter pressure injury of greater than 3 months. His medical history includes Down’s Syndrome with some verbal communication, and past dislocation of his left shoulder without repair. This patient was living in a group home and unable to maintain bed rest. The patient tended to lean to the right side in his wheelchair due to the discomfort of his left shoulder. He was seen by the surgeon for surgical debridement of the wound. Wet-to-dry (Dakins 0.125% solution) gauze dressings were ordered after surgery and dressings were changed two times a day. After 15 days, no progress was noted, and this patient would cry and fight his care givers whenever the dressings needed to be changed. Eventually, the wound refilled with slough and eschar and the periwound area presented with erythema and several small skin tears from tape. Induration was noted along with an odor and the patient was taken to surgery for further debridement and admitted to the hospital for bedrest, intravenous antibiotics, and NPWT using the V.A.C.ULTA™ Therapy System using the traditional V.A.C.® Drape, with dressing changes every 2-3 days. Post-surgical wound measurements were 2.0 x 2.1 x 2.4-cm3. Due to the MARSI, we had tried a hydrocolloid dressing around the periwound skin for placement of the V.A.C. drape for a seal; however, patient discomfort at dressing changes and periwound skin irritation were still noted.
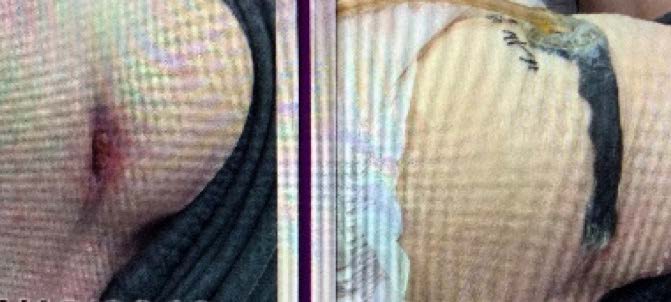
We chose this patient for the trial of the DERMATAC™ Drape to help with improved periwound skin comfort and reduced pain during dressing changes (Figure 2). Fortunately, the patient displayed greater comfort and cooperation almost immediately upon utilization of the DERMATAC™ Drape with V.A.C.ULTA™ Therapy System. Periwound skin irritation was resolved after 2 days of NPWT with the DERMATAC™ Drape. After 33 days of NPWT with DERMATAC™ Drape, the wound bed was 90% covered with healthy granulation tissue. The patient was discharged to a long-term acute care nursing facility to continue NPWT.
For this patient, use of DERMATAC™ Drape with NPWT achieved a positive outcome of full closure of periwound skin tears, reduced the patient’s fear of dressing changes, and promoted granulation tissue formation in the wound bed.
Case 3
A 70-year-old male presented with a rectal surgery wound dehiscence of greater than 4 months. The patient had a history of rectal cancer with radiation prior to surgery followed by a partial colectomy with rectal closure resulting in a permanent colostomy. The patient was taking long-term oral antibiotics as prescribed by the infectious disease specialist. This patient had been discharged from the hospital with the ACTIV.A.C.™ Therapy System using traditional V.A.C.® Drape in place and was followed by Home Health. Dressing changes occurred every 2-3 days. The patient complained of itching and discomfort at the rectal and gluteal cleft due to the drape being used to hold the NPWT dressing in place and was applying an antifungal spray to his skin prior to application of the next drape dressing. Redness, weeping, and pruritus were noted in the wound, and the patient was referred to the wound clinic after 60 days to have the moisture and pruritus addressed. The excess moisture caused the dressing seal of the drape to be difficult to maintain. We decided that the patient should try the DERMATAC™ Drape due to discomfort. The wound underwent mechanical debridement where wound infection and a cyst were identified. The cyst was drained, and that patient was started on oral antibiotics. Application of NPWT using V.A.C. WHITEFOAM™ Dressing in the explored wound tunnel, V.A.C. SIMPLACE™ Dressing, and DERMATAC™ Drape were performed (Figure 3). After 70 days of NPWT with DERMATAC™ Drape, the wound was fully closed.


During dressing changes, the patient commented that the dressing was much less harsh on his skin during removal and that he did not have any further pruritus (Figure 4). Maintaining the seal was supported with the application of the DERMATAC™ Drape. Due to the fact that the wound was in the gluteal cleft, it was initially difficult to place the dressing without wrinkles and creases; however, the DERMATAC™ Drape could be lifted, and upon initial placement, reset to move the dressing and rid the area of wrinkles. In the end, the patient experienced immediate relief that lasted until the next dressing change.
Overall, our experience with the DERMATAC™ Drape was a positive one. We selected patients under stressful living and clinical conditions for the study time frame. With this said, there are important conclusions that one can take away from this case series:
- Although, the DERMATAC™ Drape was prone to rolling edges in Case 1, the product merits further study on patients displaying lesser extremes. This case demonstrates, as one would expect, that there is a limit to the DERMATAC™ Drape ability to resist rolling.
- Case 2 yielded excellent results regarding patient pain. The DERMATAC™ Drape will be an important tool for our center in the reduction of patient anxiety as it relates to pain during dressing changes.
- Case 2 also demonstrated that the DERMATAC™ Drape can be used on delicate periwound skin which may help reduce MARSI.
- Case 3 illuminates the scenario in which the DERMATAC™ Drape may be a valuable tool when a drape requires repeated lifting and repositioning during initial placement over acute body terrain.
During our evaluation of DERMATAC™ Drape, it was found to be easier to handle, cut, apply, and readjust than traditional V.A.C.® Drape. A similar amount of adhesiveness to V.A.C.® Drape was noted; however, DERMATAC™ Drape was easier on the skin. In this case series at our center, the DERMATAC™ Drape generated meaningful positive outcomes when used for with NPWT. Our case series also demonstrates that under the most stressful of conditions the DERMATAC™ Drape can perform admirably and should be considered as an essential item in the wound specialist’s toolbox.
References
- Hy-Tape International. Medical adhesives and wound dressing application strategies. Wound Source. https://www.woundsource.com/blog/medical-adhesives-and-wound-dressing-application-strategies. Accessed September 1, 2019.
- McNichol L, Lund C, Rosen T, Gray M. Medical adhesives and patient safety: state of the science: consensus states for the assessment, prevention, and treatment of adhesive-related skin injuries. J Wound Ostomy Continence Nurs. 2013;40(4):365-380.
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
Specific indications, contraindications, warnings, precautions and safety information exist for KCI products and therapies. Please consult a clinician and production instructions for use prior to applications. This material is intended for healthcare professionals.

