
Dr. Bernstein maintains active surgical staff privileges as part of the Division of Podiatry / Department of Orthopedics within St. Luke’s University and Health System in Bethlehem, Pennsylvania, USA and is the Assistant Program Director of the podiatric surgical residency. He graduated from the Temple University School of Podiatric Medicine and completed a residency in foot surgery at Aria – Jefferson Health Bucks County Hospital, a Limb Salvage fellowship in Atlanta, Georgia, USA with Dr. Stanley Kalish, and a traveling fellowship in Limb Lengthening and Reconstructive Surgery with Ilizarov Technique at the Orthopedic and Traumatologic Department of Garcia de Orta Hospital in Almada, Portugal. Dr Bernstein is a consultant for 3M.
Bernstein_Current-Dialogues-in-Wound-Management_2021_Article 8
A diabetic foot wound can be a frustrating diagnosis with which to grapple. It necessitates all of the basic tenets of chronic wound care in order for successful outcomes: maintaining a moist wound bed, performing frequent and complete sharp debridement, and assessing and correcting any macrovascular restrictions to the extremity to achieve healing. In addition, successful wound specialists will usually use a benchmark to assess the efficacy of their treatment plan. A typical benchmark is 50% surface area healing after 4 weeks of treatment based on studies showing that wounds failing to achieve this benchmark will not likely heal within 12 weeks.1,2
When a diabetic foot wound has a suboptimal healing velocity despite a moist wound bed, adequate arterial perfusion, and aggressive debridement – mechanical pressure is the typical culprit. Pressure can mean many things; direct pressure under a bony prominence, tendon imbalance causing pressure maldistribution, shear forces, or repetitive microtrauma of the area. Maintaining a robust wound healing trajectory in a diabetic neuropathic foot wound necessitates an aggressive offloading plan. There are unique non-surgical and surgical off-loading options for each specific anatomic area of the foot and ankle. Typically, non-surgical options are attempted first, and surgical options are reserved for situations when non-surgical offloading fails to achieve an optimal wound healing velocity.
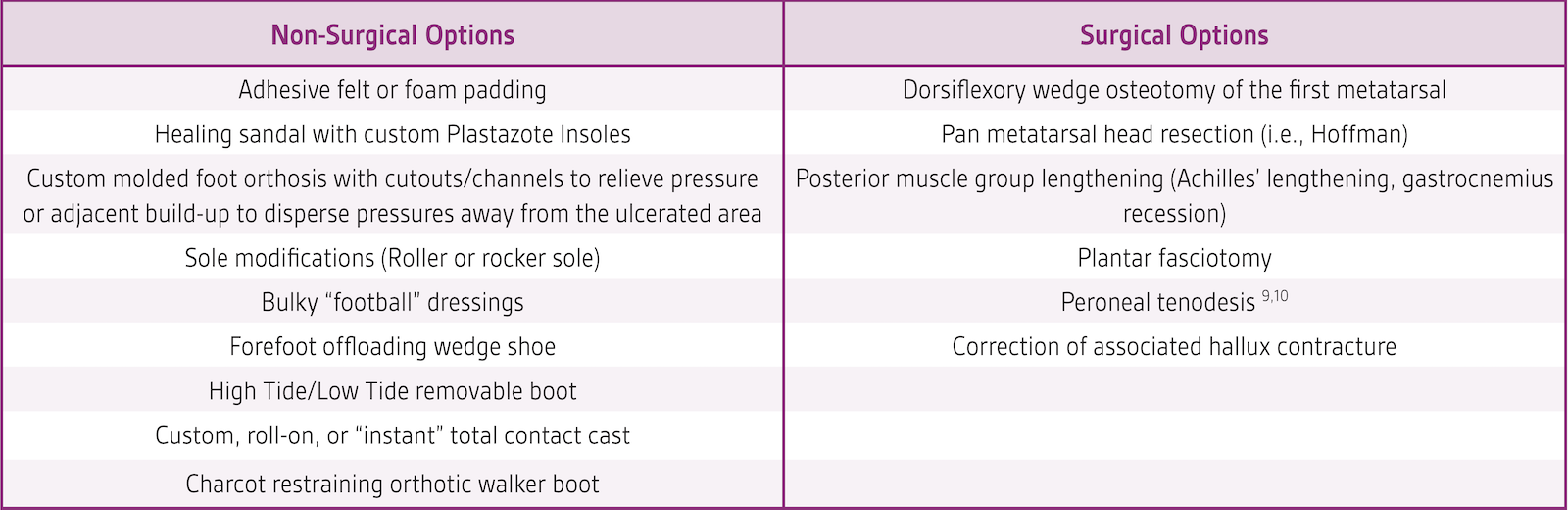
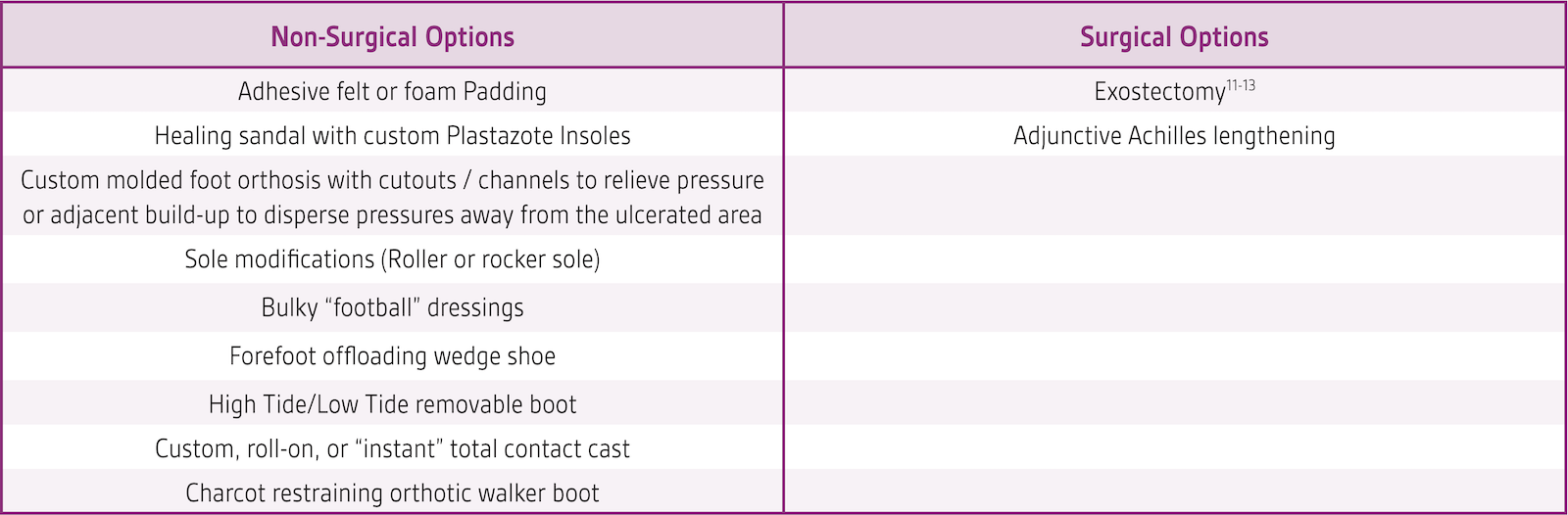
This article will serve as a primer for the busy practitioner when attempting to offload a diabetic foot lesion. Non-surgical and surgical offloading options by anatomic area are shown in Tables 1-16. Non-surgical options for each unique anatomic area will be discussed. Clinicians should note that observational and anecdotal experience has shown that approximately 30% of diabetic foot wounds ultimately require some type of surgical offloading procedure, however, a detailed description of surgical offloading options is beyond the scope of this article. There are numerous resources detailing the concepts of surgical offloading that should also be reviewed.3-6
Strict Non-Weightbearing
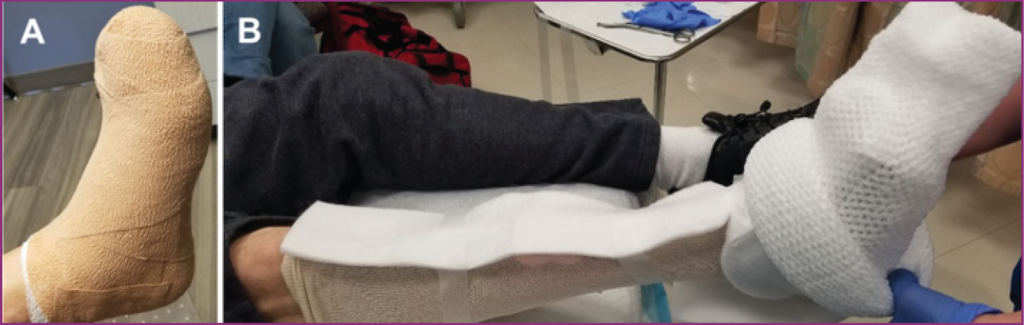
The vast majority of neuropathic ulcers will heal via strict non-weightbearing. However, few patients will be willing or capable of remaining non-weightbearing consistently enough to have a successful outcome. Typical issues are constraints of workplace, non-occupational responsibilities, structure of the residence, balance and strength issues, or general unwillingness. Devices available to allow absolute non-weightbearing on the injured extremity are under-arm crutches, forearm crutches, walker, knee scooter (Figure 1), knee-walker prosthetic, and wheelchair. In isolated situations, these may be viable options.

Offloading Specific Anatomic Locations
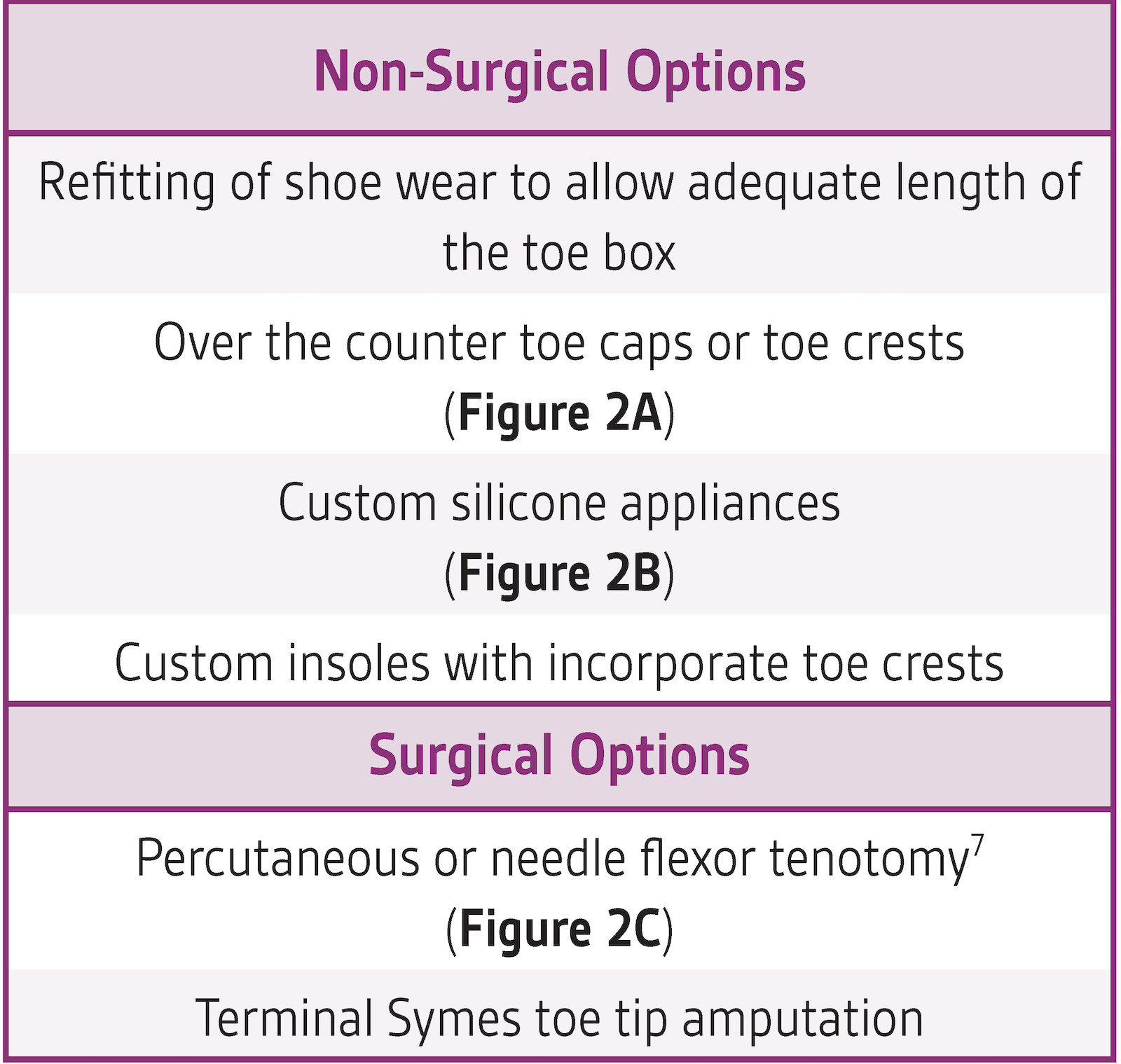
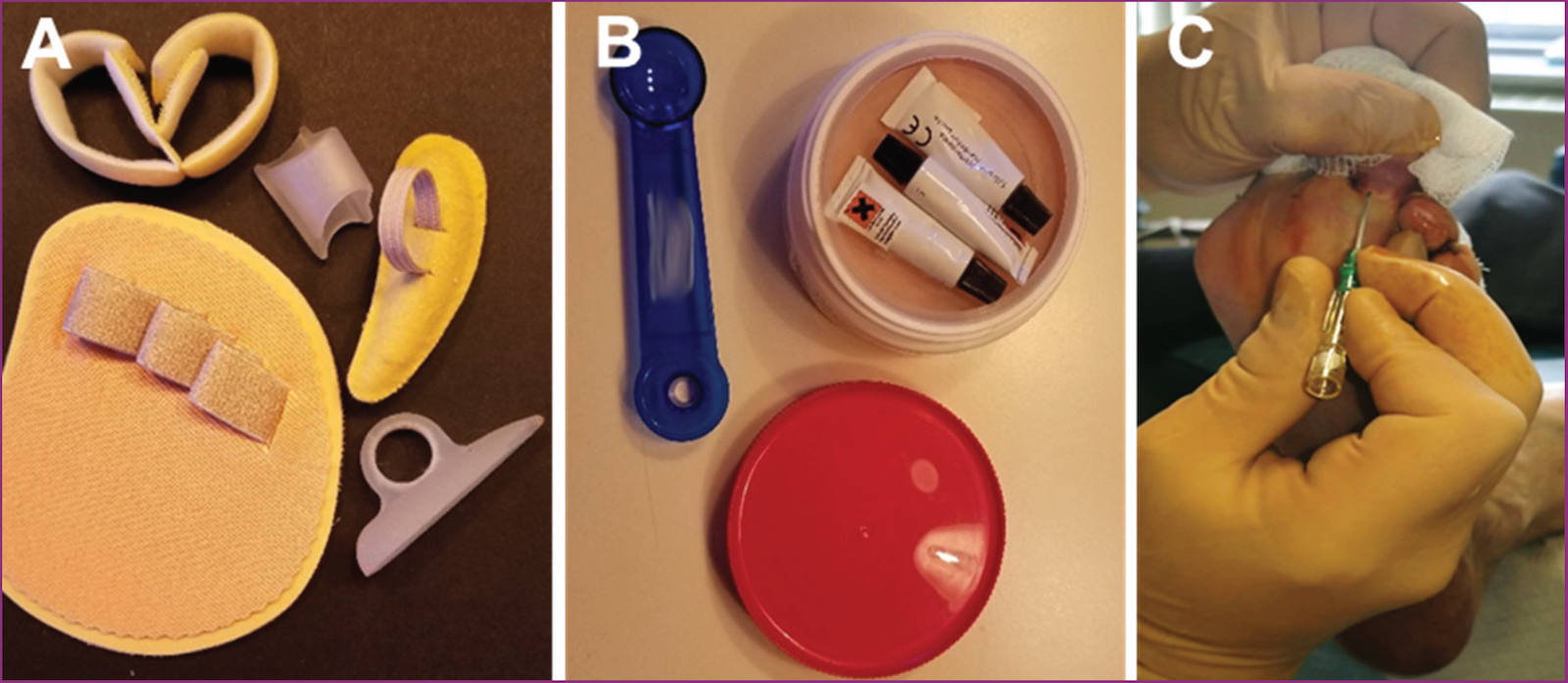
Distal lesser toes
The distal toes can become ulcerated due to ill-fitting (too short) shoe wear or from contractures of the flexor tendon (mallet toes or claw toes). One must be suspicious of any lesion on the tip of the toe as this can foretell underlying critical ischemia or of distal emboli with a predilection to lodge in the tiny terminal toe arterial tree (sometime known as “trash foot”). A full arterial evaluation and history is usually warranted when dealing with these lesions.
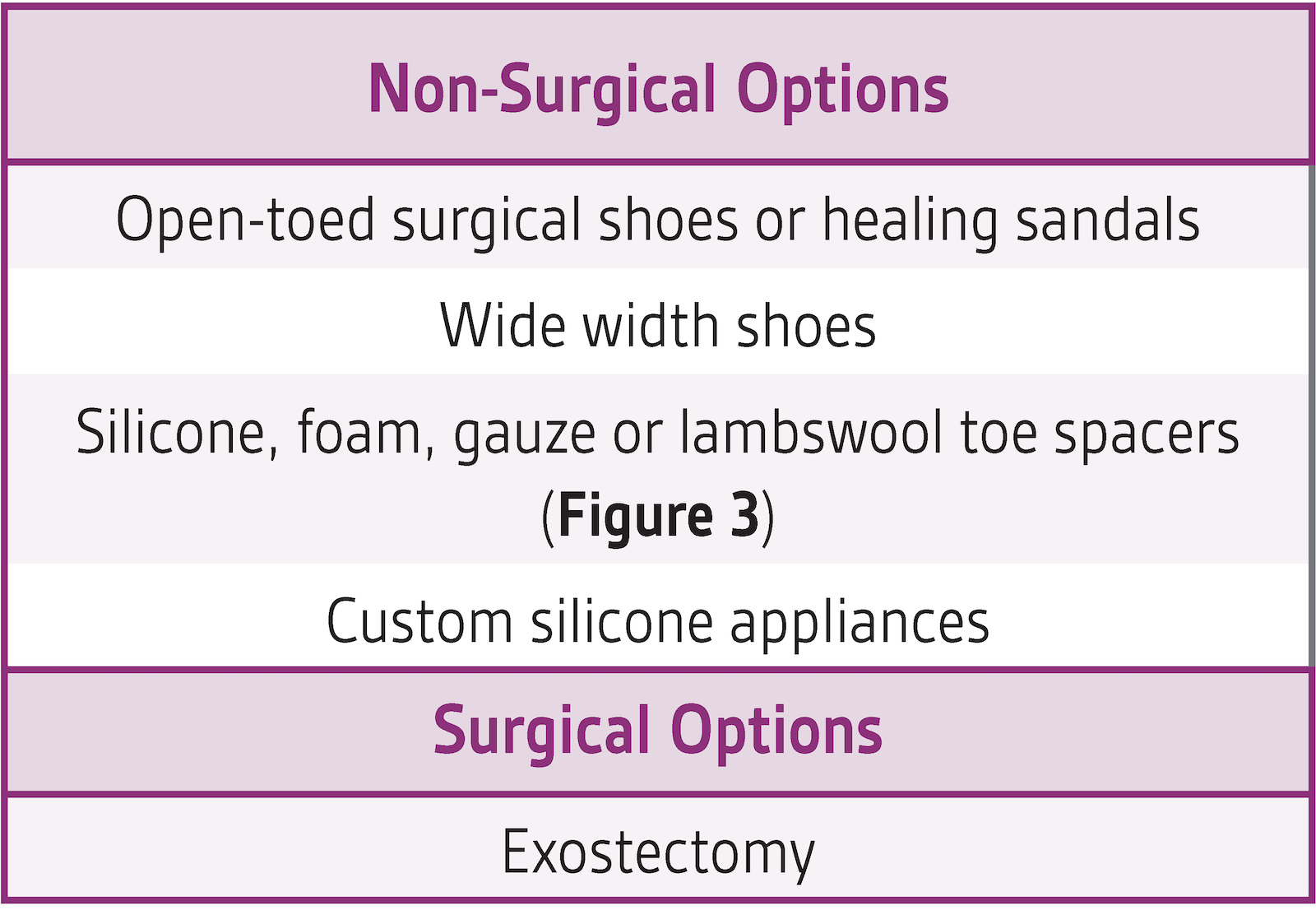
Interdigital
Interdigital surfaces between toes can be ulcerated due to crowding in a narrow toe box or from bony protuberances and deformities causing pressure necrosis between the toes. These lesions can sometimes be called “kissing” ulcers as both adjacent toes may have wounds “facing” each other. In this scenario close attention to the vascular supply to the foot is necessary, as interdigital skin breakdown is common in ischemic feet.

Dorsal Lesser Toe
Ulcerations on the dorsal lesser toes are typically due to a combination of sagittal plane toe contractures (claw toes, hammertoes, cross-over deformity) and inadequate depth in the toe box of a shoe. Diabetic motor neuropathy plays a role in formation of the toe deformities (known as an Intrinsic Minus Foot).

Distal Hallux
Distal hallux ulcers are typically associated with hallux clawing. Distal hallux ulcers can be difficult to deal with non-surgically and may often ultimately require a surgical solution.

Dorsal Hallux
Dorsal hallux ulcers are also typically associated with a hallux claw toe but somewhat easier to deal with than a distal hallux lesion without resorting to surgery.
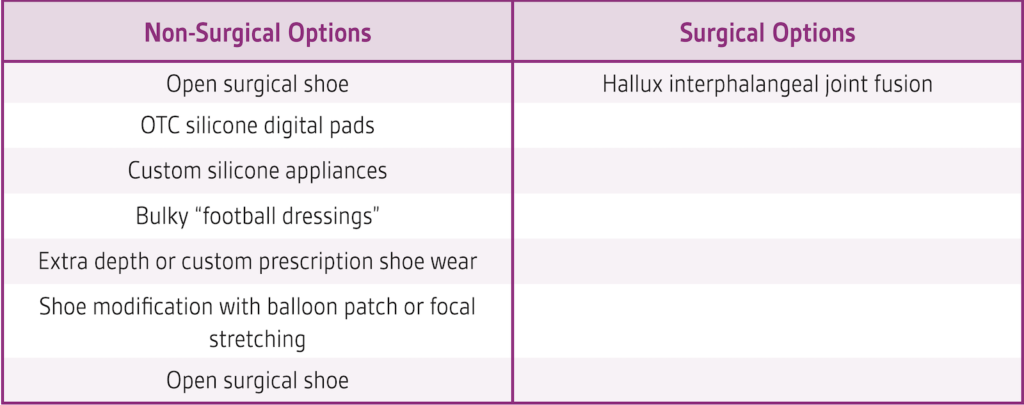
Plantar Hallux
A plantar hallux lesion is typically associated with hallux limitus. The limited range of motion of the hallux causes a high pressure spike sub-hallux when propulsing that leads to callous and ulceration development. Occasionally, a hallux interphalangeal accessory sesamoid bone may also be the underlying issue.
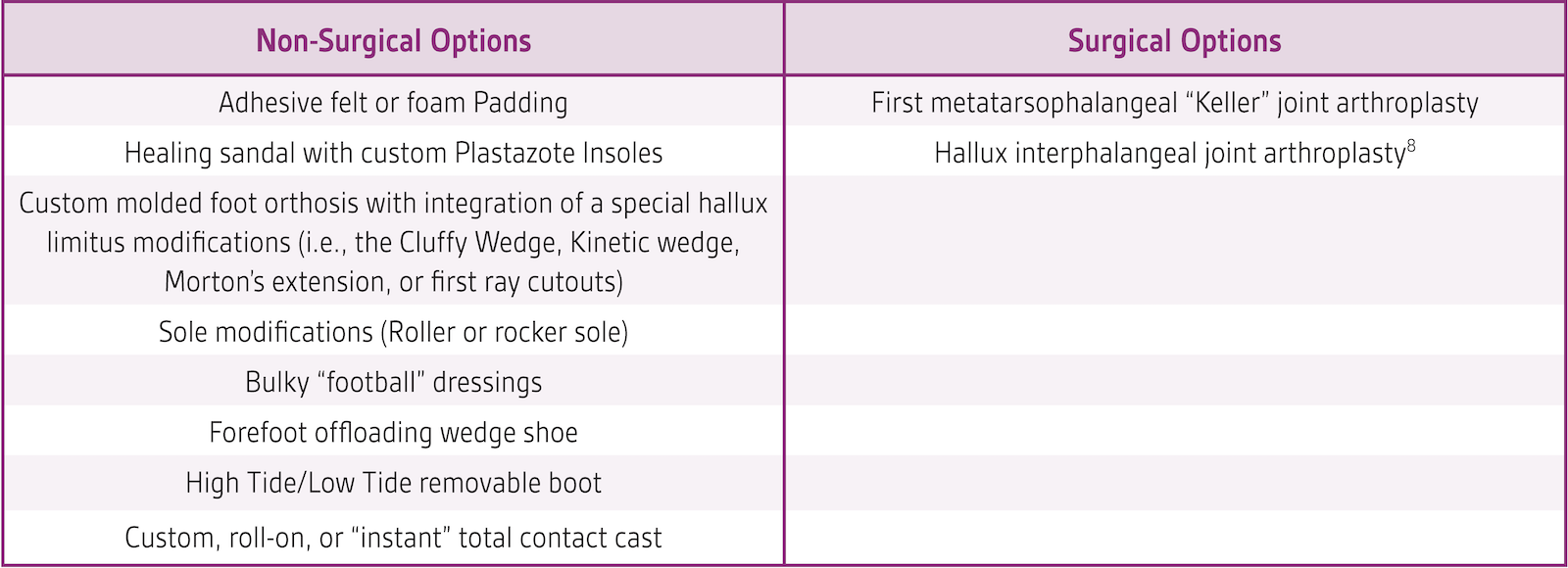
Sub metatarsal
These are some of the most common diabetic foot ulcers encountered in clinical practice and can be associated with toe deformities causing retrograde buckling, equinus, discrepancies in the metatarsal parabola from prior iatrogenic deformities (from previous ray or metatarsal head amputations).
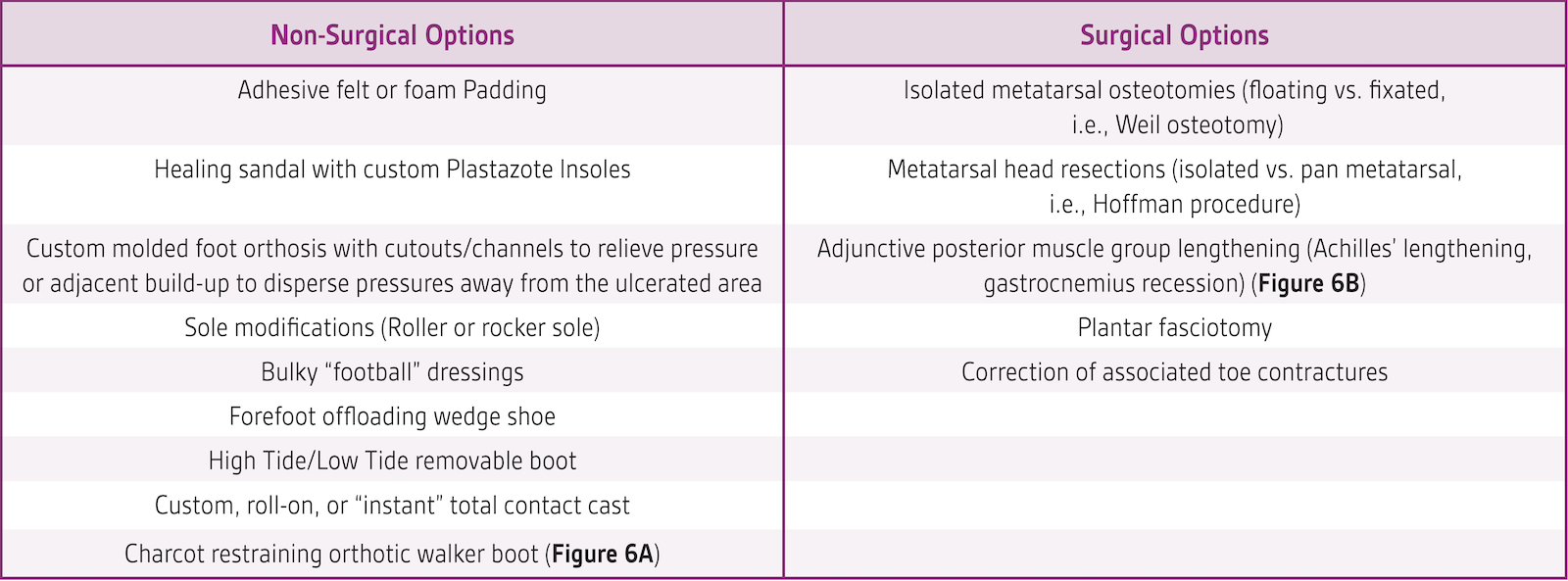
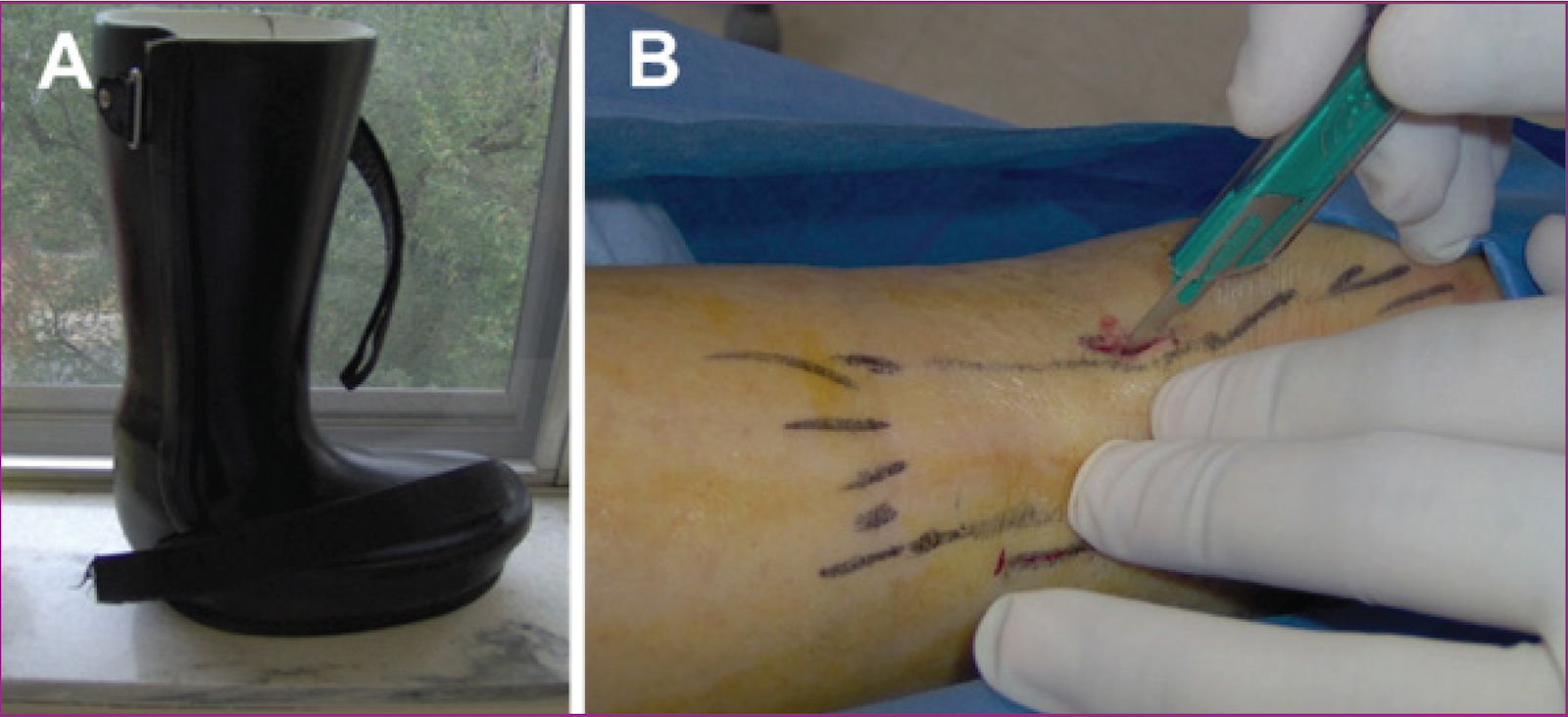
photo courtesy of Brent Bernstein, DPM
Sub metatarsal heads
Lesions under the first metatarsal heads can be due to discrepancies in the metatarsal parabola from prior iatrogenic deformities (previous ray or metatarsal head amputations), equinus, a plantarflexed first ray deformity which can be flexible, semirigid, or dynamic.
Chopart’s Amputation Stump Ulcer
In contrast to a simple shoe filler required from more distal amputations, patients who have undergone a Chopart’s amputation will require high profile bracing for life. Despite this, stump ulceration due to equinus is a very common sequela (even when appropriate Achilles tenectomy and tendon rebalancing has been performed) due to the shortened foot lever arm and subtalar joint instability.
Medial Cuneiform in Isolated in Plantigrade Foot
These lesions typical respond well with aggressive non-surgical offloading (i.e., total contact cast) and less so to more limited measures. Resistant cases that require surgery have been shown to respond well to simple bony exostectomy.
Cuneiforms in rocker bottom foot
These lesions typically do not heal as well with non-surgical offloading other than total contact cast and have high recurrence rates in anything other than long term use of a Charcot restraining orthotic walker boot. If ambulation in prescription shoes is considered the goal, these feet usually require realignment via reconstruction rather than simple exostectomy.
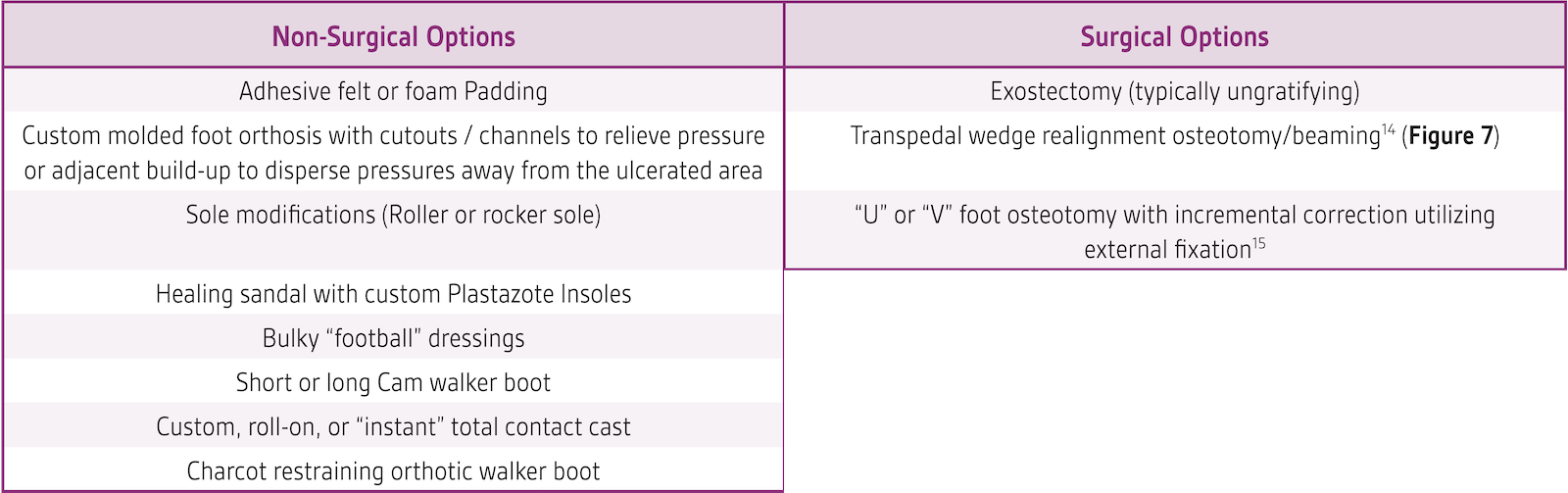
Lateral (Cuboid) Midfoot
This is commonly seen in midfoot Charcot neuroarthropathy cases when there is fragmentation of the navicular bone. Clinicians may see a typical radiographic finding of bone debris above the talar head (remnants of the navicular) and the clinical manifestation of a short medial column and associated C-shaped/Bean-shaped foot. These lesions can be very difficult to heal without surgical means and are also typically resistant to simple exostectomy procedures and require hindfoot realignment procedures.
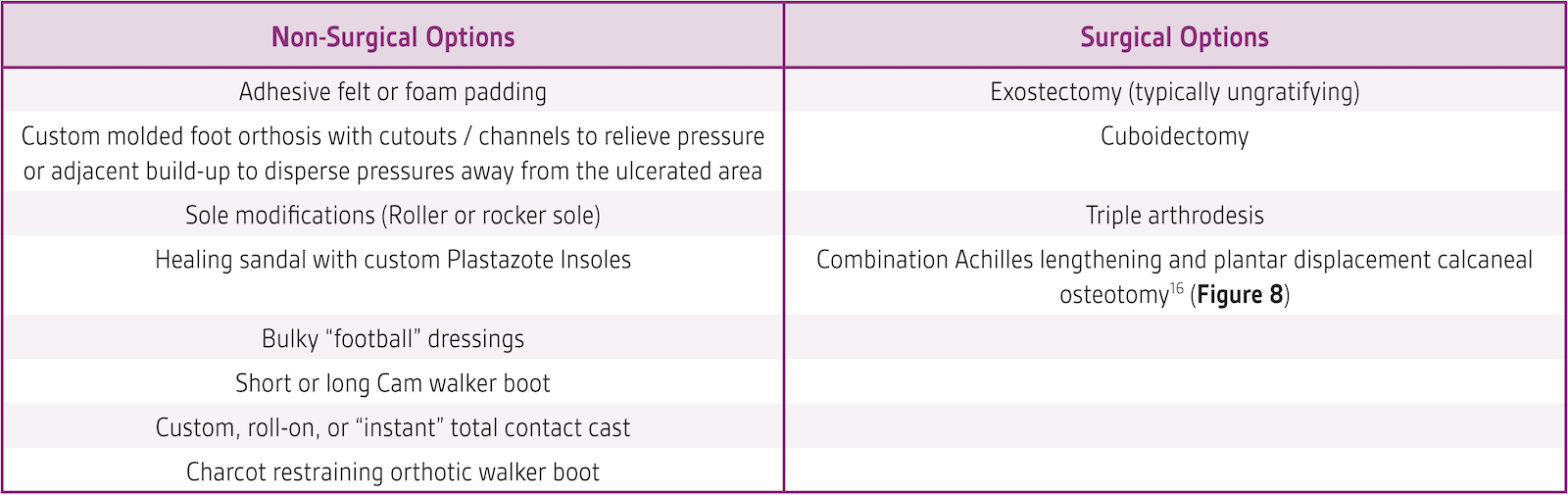
Plantar Heel
The plantar heel ulceration is one of the most difficult to heal. These lesions can result from inappropriate posterior muscle group lengthening in the presence of a cavus foot type. In these cases, pseudoequinus can masquerade as true equinus, leading the surgeon to perform Achilles tendon or gastrocnemius recession, resulting in a calcaneus gait. These lesions can be frustrating to heal non-surgically.
Posterior Heel
The posterior heel lesion is most common after periods of prolonged immobilization in a supine position. Offloading must primarily address the supine (bedbound) position, with adjunctive ambulatory offloading a somewhat more secondary concern as pressure when ambulatory is less direct.

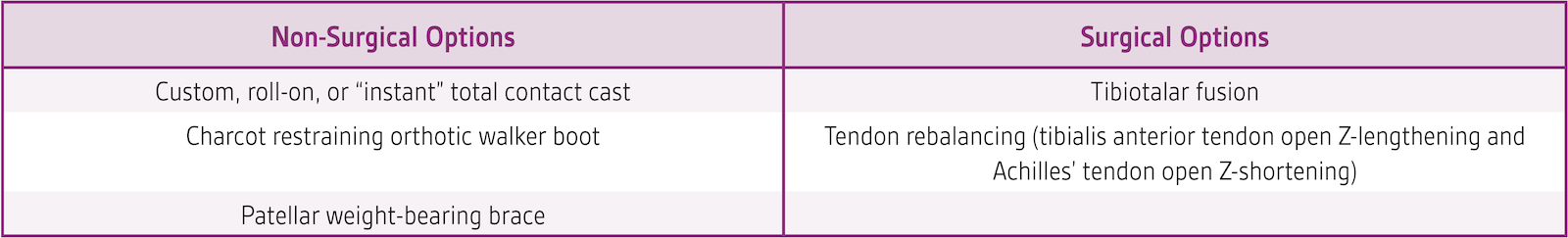
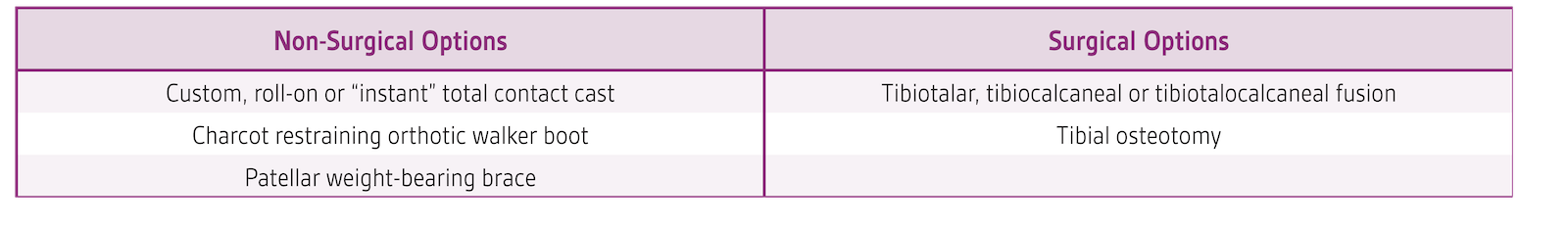
Medial/Lateral Malleolus
These lesions are typically associated with valgus or varus ankle deformities that are either iatrogenic, traumatic, neuromuscular, or secondary to neuroarthropathy. Non-surgical offloading can be ungratifying and surgical stabilization is the more likely successful treatment.
Special Situations
Lower Leg Ulcerations with Tendon Involvement
Clinicians may encounter patients with wounds over the posterior, anterior or lateral lower leg muscle compartments with exposed tendon that can be seen “pistoning” during range of motion of the foot and ankle. These are known amongst wound care clinicians as mobile wound bed situations. These lesions can be difficult to manage with standard wound care modalities and are at high risk for migrating infection into the tendon sheaths. Clinicians may have success applying a rigid cast on the extremity and creating a “window” in the cast overlying the lesion, through which a negative pressure dressing is applied. The limitation of joint excursions combined with the wound edge stabilization via a negative pressure wound therapy dressing can have a powerful synergistic effect.
Bathroom
Clinicians go to great lengths to ensure offloading and immobilization, but many times healing can be undone during unprotected weightbearing in showers and bathroom areas. Clinicians may consider a thick closed cell foam pad be cut to fit both the shower floor as well as the floor immediately adjacent to the shower so the patient can ingress/egress the area without developing high pressures on the hard tile floor. Commercially available pressure relief mats are available or a “pool floatation” mat can be cut to shape to serve the same purpose.
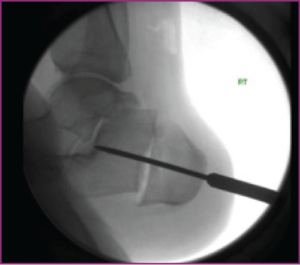
Severe non-compliance and flaps
In extreme cases (such as deformities that are too severe or too unstable to be braced or casted, patients who have demonstrated repeated unwillingness to remain non-weightbearing or after extensive flap procedures) external fixation can be utilized to “float” the heel or plantar foot utilizing either a tripod technique for posterior heel lesions/flaps, or a secondary ring below the foot ring for plantar foot lesion/flaps. However, this is an invasive and expensive modality, so its use should be recommended judiciously.18
References
- Margolis DJ, Kantor J, Berlin JA. Healing of diabetic neuropathic foot ulcers receiving standard treatment. A meta-analysis. Diabetes Care. 1999;22(5):692-695.
- Sheehan P, Jones P, Caselli A, Giurini JM, Veves A. Percent change in wound area of diabetic foot ulcers over a 4-week period is a robust predictor of complete healing in a 12-week prospective trial. Diabetes Care. 2003;26(6):1879-1882.
- Armstrong DG, Lavery LA, Stern S, Harkless LB. Is prophylactic diabetic foot surgery dangerous? J Foot Ankle Surg. 1996;35(6):585-589.
- Finestone AS, Tamir E, Ron G, Wiser I, Agar G. Surgical offloading procedures for diabetic foot ulcers compared to best non-surgical treatment: a study protocol for a randomized controlled trial. J Foot Ankle Res. 2018;11:6.
- Frykberg RG, Bevilacqua NJ, Habershaw G. Surgical off-loading of the diabetic foot. J Vasc Surg. 2010;52(3 Suppl):44S-58S.
- Todd N, Jennings M, Rush S. Current concepts in surgical offloading of the diabetic foot. Podiatry Today. 2012;25(5).
- Elmarsafi T, Kim PT. Digital flexor tenotomy: an emerging answer for surgical offloading. Podiatry Today. 2016;29(9).
- Rosenblum BI, Giurini JM, Chrzan JS, Habershaw GM. Preventing loss of the great toe with the hallux interphalangeal joint arthroplasty. J Foot Ankle Surg. 1994;33(6):557-560.
- Dayer R, Assal M. Chronic diabetic ulcers under the first metatarsal head treated by staged tendon balancing: a prospective cohort study. J Bone Joint Surg Br. 2009;91(4):487-493.
- Hamilton GA, Ford LA, Perez H, Rush SM. Salvage of the neuropathic foot by using bone resection and tendon balancing: a retrospective review of 10 patients. J Foot Ankle Surg. 2005;44(1):37-43.
- Brodsky JW, Rouse AM. Exostectomy for symptomatic bony prominences in diabetic charcot feet. Clin Orthop Relat Res. 1993(296):21-26.
- Catanzariti AR, Mendicino R, Haverstock B. Ostectomy for diabetic neuroarthropathy involving the midfoot. J Foot Ankle Surg. 2000;39(5):291-300.
- Laurinaviciene R, Kirketerp-Moeller K, Holstein PE. Exostectomy for chronic midfoot plantar ulcer in Charcot deformity. J Wound Care. 2008;17(2):53-55, 57-58.
- Grant WP, Garcia-Lavin S, Sabo R. Beaming the columns for Charcot diabetic foot reconstruction: a retrospective analysis. J Foot Ankle Surg. 2011;50(2):182-189.
- Lamm BM, Gourdine-Shaw MC, Thabet AM, Jindal G, Herzenberg JE, Burghardt RD. Distraction osteogenesis for complex foot deformities: Gigli saw midfoot osteotomy with external fixation. J Foot Ankle Surg. 2014;53(5):567-576.
- Bernstein BH, Seiler D. Inferior calcaneal slide osteotomy for the treatment of a sagittal plane dominant charcot foot deformity. Paper presented at: Presented at the American Colllege of Foot and Ankle Surgeons Annual Conference, February 27 – March 2, 2014, Orlando, FL; 2014 Feb-Mar, 2014.
- Perez ML, Wagner SS, Yun J. Subtotal calcanectomy for chronic heel ulceration. J Foot Ankle Surg. 1994;33(6):572-579.
- Roukis TS, Landsman AS, Weinberg SA, Leone E. Use of a hybrid “kickstand” external fixator for pressure relief after soft-tissue reconstruction of heel defects. J Foot Ankle Surg. 2003;42(4):240-243.
©2021 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. 3M marks used under license in Canada. All other marks are property of their respective owners. [PRA-PM-US-03434 (09/21)]

