
Dr. Timothy Alton is a dual fellowship-trained orthopedic surgeon. He completed his first fellowship in fracture surgery at Harborview Medical Center in Seattle, WA then completed a second fellowship in adult reconstruction, hip and knee replacement. He trained directly under Dr. William Barrett at Valley Medical Center in Renton, WA, mastering the anterior approach for total hip replacement and primary knee replacements. He then traveled the country learning advanced arthroplasty and revision techniques from master surgeons at the Florida Orthopedic Institute in Tampa, FL and the world-renowned Mayo Clinic in Rochester, MN. Dr. Alton specializes in the management of primary and revision hip and knee replacement surgery, infections, and fractures of the upper and lower extremity. He has published in national and international journals, has written multiple book chapters, and presented his research at local, national, and international meetings. Dr. Alton teaches other orthopedic surgeons hip and knee replacement techniques at national courses and has a particular interest in revision surgery. He is also interested in direct anterior total hip replacement surgery and moving joint replacement surgery from the inpatient to outpatient setting. He practices at Proliance Orthopedic Associates in Renton, WA and Covington, WA locations.
Alton_Current-Dialogues-in-Wound-Management_2021_Article 12
TJA surgery is moving to the Ambulatory Surgical Center setting
With the emergence of COVID-19 in 2020, the healthcare system of the United States (US) was significantly impacted. Major hospital systems were overflowing with critically ill patients, death rates and COVID-19 cases climbed, and medical resources were, at times, sparse. Elective surgeries were halted in most US cities in the spring of 2020, and some continued to see further restrictions throughout the year. Hospitals, where many patients often spent 1-2 nights after total hip or total knee replacement surgeries, did not have the capacity to support elective joint replacement surgery patients.
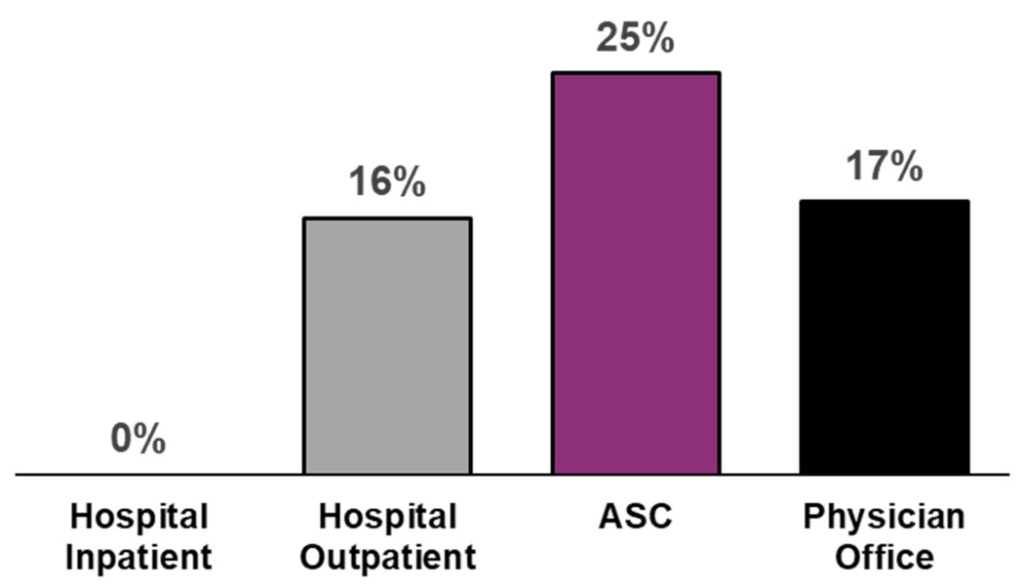
Orthopedic surgeons adapted to these stresses, and the trend of transitioning elective total joint replacement cases to the ambulatory surgery center (ASC) rose dramatically. At many times in 2020, outpatient ASC settings were the only locations total joint arthroplasty (TJA) could be performed. While this trend had already started before COVID-19 (Figures 1-2), it was accelerated in 2020 as orthopedic surgeons became more and more comfortable performing TJA surgery in the ASC setting. By 2028, it is estimated that 53% of all TJA in the US will be performed in outpatient settings with an estimated increase of 1105% for knee arthroplasty and 712% for hip arthroplasty in outpatient volumes.1
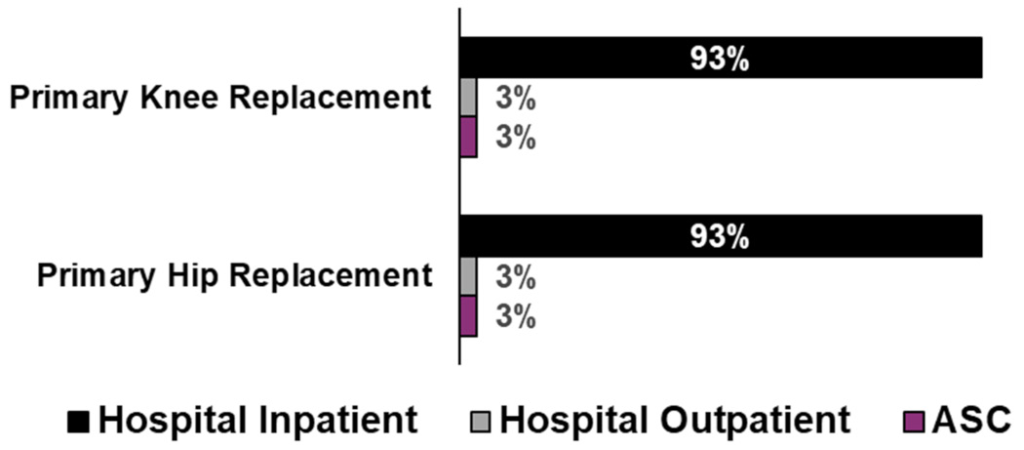
performed. Adapted from Sg2.1
An additional force driving TJA to the ASC setting is physician reimbursement, which is now being linked to the cost associated with the episode of care in “bundles.” If surgeons can find ways to provide care for less cost, they are incentivized by increased reimbursements. TJAs performed in an ASC setting are often less expensive than a hospital setting. Entrepreneurial orthopedic surgeons, who often own part or all of an ASC, may benefit financially by doing more TJA surgeries in their ASC. Additionally, previous restrictions placed by Medicare regarding where TJAs can be performed have been lifted.2
The stress of COVID-19 on the health care system with a changing reimbursement market combined with costs becoming critical and physician reimbursement more and more commonly linked to the cost of the episode of care have caused a significant change in the way TJAs are performed in the US. TJA in the ASC setting is here to stay.
The argument for 3M™ Prevena™ Therapy use in hip and knee arthroplasty
In general, total hip arthroplasty (THA) and total knee arthroplasty (TKA) are very successful operations.3 Unfortunately, complications (e.g., surgical site infections [SSI], seromas and dehiscence) can occur. These complications have been extensively studied and many risk factors have been identified.4 Some risk factors, such as smoking, diabetes and obesity, are considered modifiable. Patients are often required to quit using tobacco, control their blood sugar and lose weight before they are offered TJA. Other risk factors, such as hypercoagulability or autoimmune disease, are not modifiable and must be managed around the time of surgery. A great deal of time and effort is spent optimizing patients before elective TJA.3
However, one tool that has become available to help decrease the risk of postoperative complications is 3M™ Prevena™ Therapy. Clinical studies have been published supporting the use of Prevena Therapy after TJA surgery to reduce postoperative complications.5-7 Additional studies have shown significant improvement in reducing rates of SSI, dehiscence, and reoperations after hip and knee replacement revision surgery and after fixation of periprosthetic fractures.8,9 When patient optimization before surgery is not feasible, Prevena Therapy can be especially useful. Significant benefits are being reported in these patient populations in the literature. A recent randomized controlled clinical trial showed reduced rates of 30-, 45- and 90-day surgical site complications and 90-day readmissions with Prevena Therapy after knee revision surgeries and was stopped at the mid-study evaluation point due to the remarkable differences between the two treatment arms and the obvious benefit with the use of Prevena Therapy.7
Many orthopedic surgeons are now using Prevena Therapy in their primary hip and knee replacement patients in selective, higher risk clinical situations and have observed clinical improvements as a result.10 As more clinical evidence emerges supporting the use of Prevena Therapy, its use may become more widespread across surgical care settings.
Support for Prevena Therapy
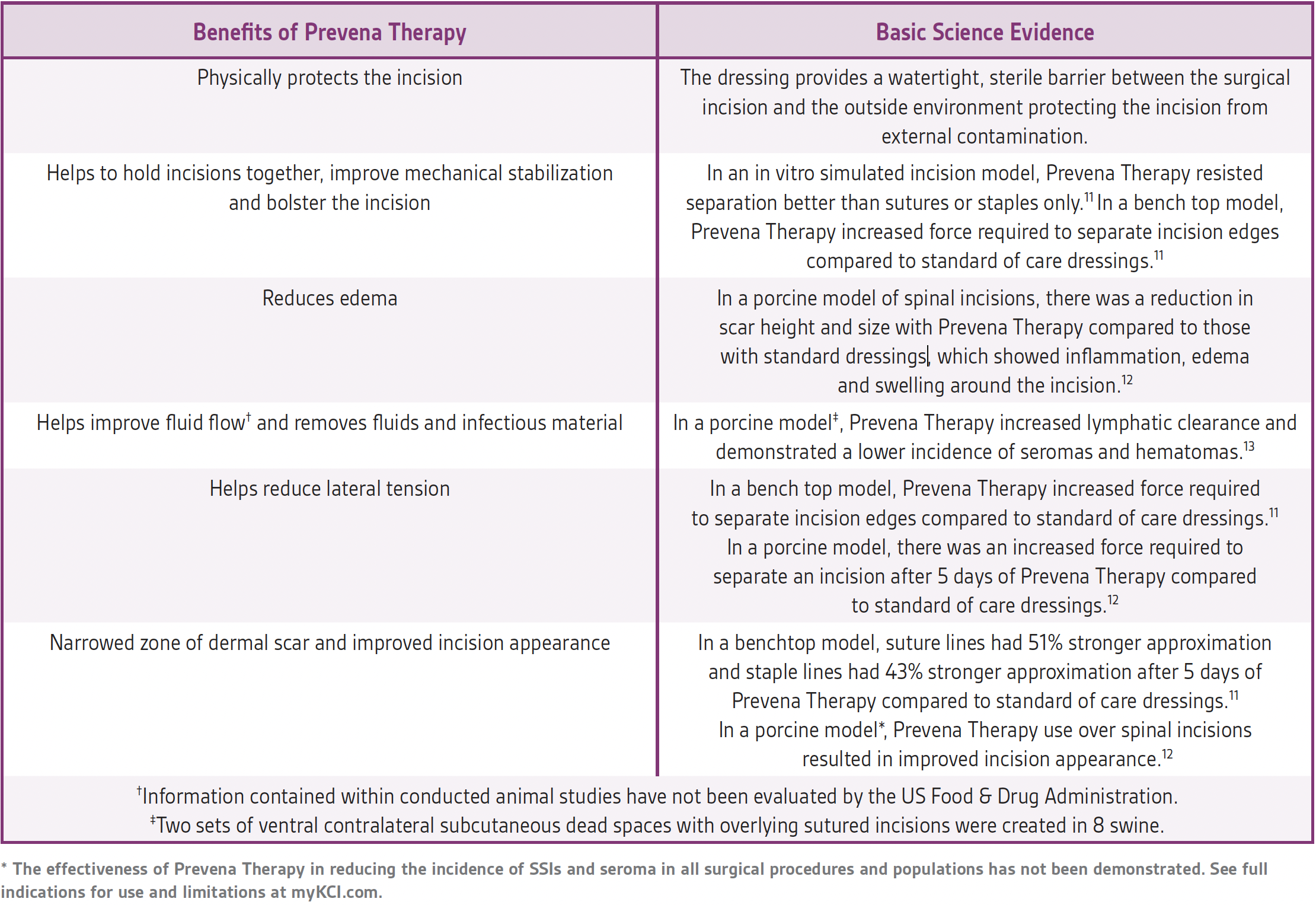
3M™ Prevena™ 125 and 3M™ Prevena™ Plus Therapy Units manage the environment of closed surgical incisions and remove fluid away from the surgical incision via the application of -125 mmHg continuous pressure to the closed incision. When used with legally marketed compatible dressings, Prevena 125 and Prevena Plus Therapy Units are intended to aid in reducing the incidence of seroma; in patients at high risk for postoperative infections, the therapy units aid in reducing the incidence of superficial surgical site infection in Class I and Class II wounds. Furthermore, Prevena Therapy is the first medical device indicated by the FDA to help reduce superficial SSIs in high risk patients with Class I and Class II wounds.*
Prevena Therapy can provide patients many well- established clinical benefits. The benefits can be explained by understanding the basic science of how the incision environment is potentially altered by the negative pressure dressing (Table 1). These basic science benefits may translate to patient care. In fact, Prevena Therapy may be most beneficial to specific patient populations. Patients with a low or high body mass index (BMI), type 2 diabetes, immunodeficiency, active tobacco use, anticoagulation therapy use and prior surgeries have been found to be at higher risk for developing surgical site complications.10 In these patients, Prevena Therapy use following surgical incision closure is recommended.
Prevena Therapy use in the ASC setting
Bundle payments are present in most major medical systems and a reality facing orthopedic surgeons. If care can be delivered for a lower cost, physician reimbursement can be greater. This motivates orthopedic surgeons to optimize patients before surgery and limit postoperative complications as much as possible. Additionally, as of May 2021, the Centers for Medicare and Medicaid Services are requiring ASCs to report quality metrics or see a reduction in payment.14 Complications, such as infections and return admissions to the hospital, will have a significant negative impact on the bundle and have been labeled “bundle busters.”15 Modifiable risk factors should be addressed before surgery, while non- modifiable risk factors are to be managed. When used in the patient at high-risk for complications, Prevena Therapy may help decrease the chance for postoperative complications and potentially improve patient outcomes and patient satisfaction, thus reducing “bundle busters”, increasing physician reimbursement, and decreasing overall cost of care.
Orthopedic surgeons may be comfortable increasing the BMI cutoff for their ASC patients if Prevena Therapy is used. This expands the number of TJA patients seen in the ASC, which may provide opportunities for treating more complex patients. They may be more comfortable operating on the patient who cannot stop smoking or the patient who has rheumatoid arthritis and is on strong immune modulating medications in the ASC setting.
Although there are additional costs associated with utilizing Prevena Therapy, these dressings can potentially decrease complication rates in higher risk patients and “bundle busters” can be avoided. With this in mind, the judicial use of Prevena Therapy in ASC settings would seem reasonable.10 Additionally, Prevena Therapy may positively impact the overall cost of care, which may decrease with TJA patients.
There is a lack of published literature regarding health economic analysis for the use of Prevena Therapy in TJA. However, health economic analyses have been published for Prevena Therapy use following elective vascular surgery, open ventral hernia repair, and breast reconstruction.16-18 Following elective vascular surgery, a $6,045 cost reduction in the Prevena Therapy group compared to a high-risk control group was reported by Kwon et al, though this was not statistically significant (p=0.11).16 Similarly, Licari et al reported lower costs among patient receiving Prevena Therapy compared to control dressings (€4,230 vs €5,695) in patients undergoing open ventral hernia repair.17 This equates to ~$4623 US vs $6224 US dollars (based on an average exchange rate from May 2020).19 Gabriel et al applied an economic model to a previous retrospective cohort.18 An estimated cost savings of $218 per patient was observed following Prevena Therapy use in postoperative breast reconstruction.18 While future studies are needed to assess the potential cost-effectiveness of Prevena Therapy use in TJA, the published reduction in SSI rates, reoperations, and dehiscence strongly indicate that cost-savings may also exist for Prevena Therapy use in TJA.5,7,8
Representative case of Prevena Therapy use in an ASC
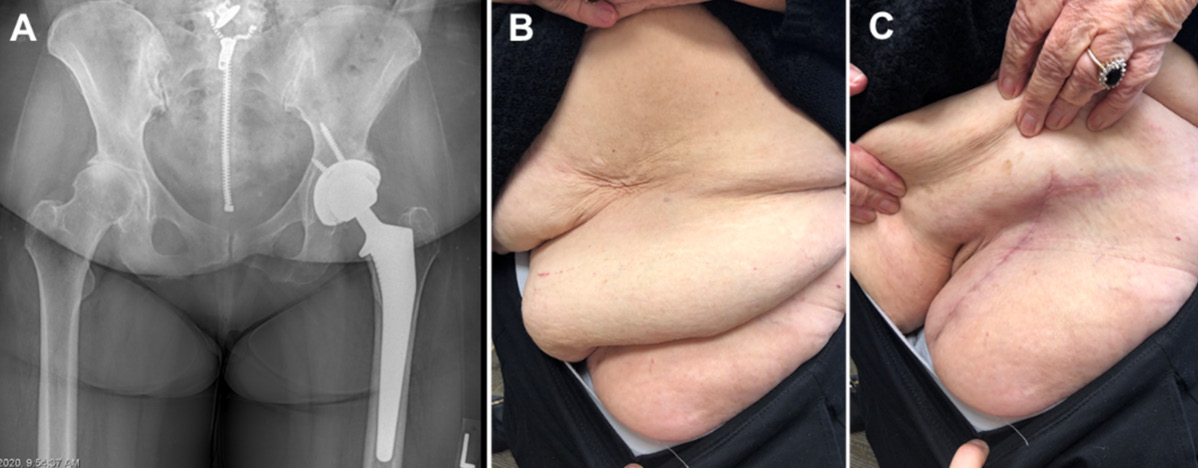
A 58-year-old female presented for care with 2 years of left hip pain, which worsened over the prior 6 months and severely limited her daily living activities (Figure 3). Her past medical history included type 2 diabetes (A1C 8.4), Factor V Leiden with unprovoked deep vein thrombosis, obesity (BMI: 41.2 kg/m2), and current cigarette smoker (1 pack per day).

Further examination revealed an antalgic gait, with very painful and limited hip rotation due to the presence of an anterior pannus. The patient showed an intact, normal neurovasculature of the distal left leg.
The patient was initially seen in the office, where a hip arthritis diagnosis was made, and treatment of total hip replacement was agreed upon. However, before surgery, patient was optimized with regards to modifiable risk factors. Her A1C level was reduced to 6.7 (goal <7). She lost weight until her BMI was 37 kg/m2 and her nutrition labs were reported as normal. The patient quit smoking for 6 weeks and passed a serum cotinine test to prove smoking cessation.
The patient underwent anterior approach total hip replacement at a surgeon-owned ASC after medical optimization. Intra-operative pannus retraction techniques, double prep and standard iodine dressings were used in addition to application of Prevena Therapy over the clean, closed incision (Figure 4). The patient was discharged to home 2 hours after surgery, having completed a physical therapy session and with good pain control. The Prevena Therapy Dressing was removed after 7 days and a standard dry gauze dressing was then applied for an additional week.
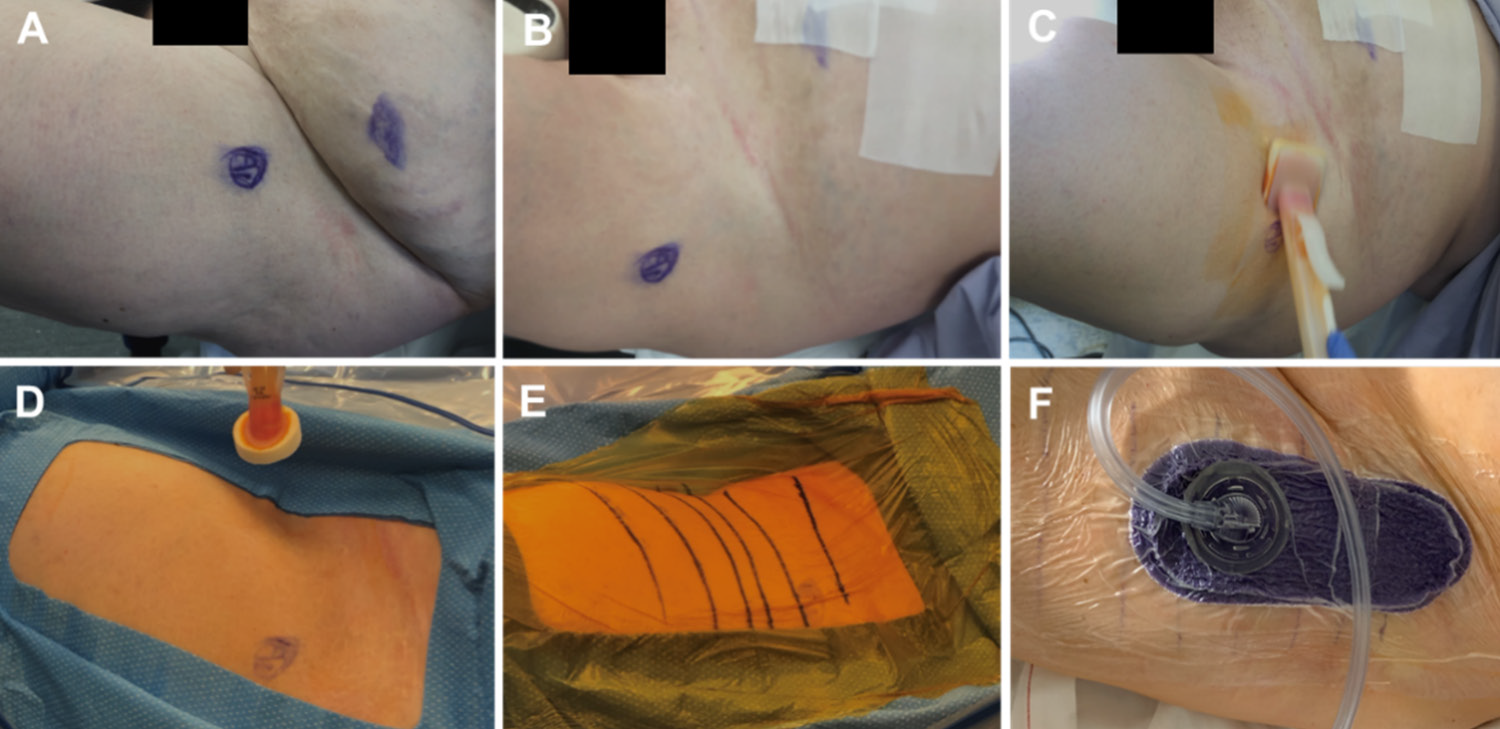
Six weeks after surgery, the patient returned to the office for routine follow-up care with no postoperative complications. Her wound was healed, and her pain was much improved compared to before surgery. She reported no issues with her surgical dressing or incision during the 7 days of Prevena Therapy use and was very satisfied with her result. There were no additional/ unexpected clinic or Emergency Room visits after surgery (Figure 5).
Conclusion:
Prevena Therapy can be used in the ASC in specific patient populations to decrease risk of postoperative complications and “bundle busters.”10 Such factors to consider are diabetes, inflammatory arthritis on immune modulating medications, elevated BMI (greater than 35), patients on anticoagulants at increased risk of postoperative bleeding, those with immune compromise such as HIV/AIDS, and smokers.4 The benefits of Prevena Therapy in the hospital operating room setting are well documented in the literature, along with reports of patient care cost reductions associated with Prevena Therapy usage. These benefits are now being observed in the ASC setting. In my experience, the judicious use of Prevena Therapy in the ASC setting may provide orthopedic surgeons with confidence to drive even more volume to the ASC, potentially decreasing the cost of TJA surgery.
References
References:
- Procedure Sites of the Future: Transitions and Growth Across HOPDs, ASCs. Skokie, IL 2019.
- Edwards PK, Milles JL, Stambough JB, Barnes CL, Mears SC. Inpatient versus Outpatient Total Knee Arthroplasty. J Knee Surg. 2019;32(8):730-735.
- Rutherford RW, Jennings JM, Dennis DA. Enhancing Recovery After Total Knee Arthroplasty. Orthop Clin North Am. 2017;48(4):391-400.
- Alamanda VK, Springer BD. The prevention of infection: 12 modifiable risk factors. Bone Joint J. 2019;101-B(1_Supple_A):3-9.
- Cooper HJ, Bas MA. Closed-Incision Negative-Pressure Therapy Versus Antimicrobial Dressings After Revision Hip and Knee Surgery: A Comparative Study. J Arthro. 2016;31(5):1047-1052.
- Pachowsky M, Gusinde J, Klein A, et al. Negative pressure wound therapy to prevent seromas and treat surgical incisions after total hip arthroplasty. Inter Ortho. 2012;36(4):719-722.
- Higuera-Rueda C, Emara AK, Nieves-Malloure Y, et al. The Effectiveness of Closed Incision Negative Pressure Therapy versus Silver-Impregnated Dressings in Mitigating Surgical Site Complications in High-Risk Patients after Revision Knee Arthroplasty: The PROMISES Randomized Controlled Trial. J Arthro. 2021;36(7S):S295-S302.
- Cooper HJ, Roc GC, Bas MA, et al. Closed incision negative pressure therapy decreases complications after periprosthetic fracture surgery around the hip and knee. Injury. 2018;49(2):386-391.
- Newman JM, Siqueira MB, Klika AK, Molloy RM, Barsoum WK, Higuera CA. Use of Closed Incisional Negative Pressure Wound Therapy After Revision Total Hip and Knee Arthroplasty in Patients at High Risk for Infection: A Prospective, Randomized Clinical Trial. J Arthro. 2019;34(3):554-559.
- Anatone AJ, Shah RP, Jennings EL, Geller JA, Cooper HJ. A risk-stratification algorithm to reduce superficial surgical site complications in primary hip and knee arthroplasty. Arthro Today. 2018;4(4):493-498.
- Wilkes RP, Kilpadi DV, Zhao Y, Kazala R, McNulty A. Closed incision management with negative pressure wound therapy (CIM): biomechanics. Surg Innov. 2012;19(1):67-75.
- Glaser DA, Farnsworth CL, Varley ES, et al. Negative pressure therapy for closed spine incisions: A pilot study. Wounds. 2012;24(11):308-316.
- Kilpadi DV, Cunningham MR. Evaluation of closed incision management with negative pressure wound therapy (CIM): hematoma/seroma and involvement of the lymphatic system. Wound Repair Regen. 2011;19(5):588-596.
- Orthopedic Measure (ASC-17). [Website]. Centers for Medicare & Medicaid Services. https://qualitynet.cms.gov/asc/measures/orthopedic. Published 2021. Updated 2021 Jun 9. Accessed 2021 Jun 9, 2021.
- Wodowski AJ, Pelt CE, Erickson JA, Anderson MB, Gililland JM, Peters CL. ‘Bundle busters’: who is at risk of exceeding the target payment and can they be optimized? Bone Joint J. 2019;101-B(7_Supple_C):64-69.
- Kwon J, Staley C, McCullough M, et al. A randomized clinical trial evaluating negative pressure therapy to decrease vascular groin incision complications. J Vasc Surg. 2018;68(6):1744-1752.
- Licari L, Campanella S, Carolla C, Viola S, Salamone G. Closed Incision Negative Pressure Therapy Achieves Better Outcome Than Standard Wound Care: Clinical Outcome and Cost-Effectiveness Analysis in Open Ventral Hernia Repair With Synthetic Mesh Positioning. Cureus. 2020;12(5):e8283.
- Gabriel A, Maxwell GP. Economic Analysis Based on the Use of Closed-Incision Negative-Pressure Therapy after Postoperative Breast Reconstruction. Plast Reconstr Surg. 2019;143(Suppl 1):36S-40S.
- Euro to US Dollar Spot Exchange Rates for 2020. www.exchangerates.org.uk Web site. https://www.exchangerates.org.uk/EUR-USD-spot-exchange- rates-history-2020.html. Published 2021. Updated 2021 Jun 23. Accessed 2021 Jun 23, 2021.
Patient data and images courtesy of Timothy B. Alton M.D., Renton, WA. He is a consultant for 3M.
© 2021 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. 3M Marks used under license in Canada. All other marks are property of their respective owners.PRP-PM-US-03261 (06/21) US_70-2013-1179-5

