
Ms. Milne is an Advanced Practice WOC Nurse providing care to patients across the continuum in acute care, long-term care, home health and outpatient settings. Employed by Connecticut Clinical Nursing Associates, she also provides consulting to organizations wishing to improve wound outcomes, conducts clinical research, lectures nationally and internationally, is the Co-Editor of the text Wound, Ostomy, Continence Secrets and provides clinical support to Wound Reference.com. She currently serves as the Co-chair of the Post-Acute Care Symposium. Additionally, she serves as a Nurse Board Member of the Association for the Advancement of Wound Care and an Associate Clinical Professor at the Yale School of Nursing. Ms. Milne is a paid consultant for Solventum.
Milne_Current-Dialogues-in-Wound-Management_2025_Article-3
In the field of wound care, one of the most critical challenges is effectively managing exudate—the fluid that leaks from wounds during the healing process. Wound exudate consists of water, electrolytes, dead host cells, bacteria, and elevated levels of matrix metalloproteases. The latter two components contribute to poor wound health, local and systemic infection, and elevated levels of inflammation. Achieving moisture balance, with a wound bed that is not too wet or too dry, is crucial for cell migration and tissue regeneration.
When exudate is excessive, it can lead to infection, delay tissue healing, compromise tissue integrity, and cause pain and social isolation for patients. Over the years, medical science has developed various dressing materials to address this challenge, among which superabsorbent dressings (SADs) have emerged as a game-changer. Under-utilized in most healthcare settings, these dressings are designed to absorb large amounts of exudate while maintaining a moist wound environment conducive to healing. Compared to foam dressings, SADs offer unique properties, benefits, and clinical applications.
SADs are indicated for managing highly exuding acute and chronic wounds, such as diabetic foot ulcers, pressure injuries, venous leg ulcers, and surgical wounds. These dressings are contraindicated for dry or minimally exuding wounds, wounds with heavy bleeding, or third-degree burns. Typically designed as flat dressings, SADs are meant to be placed over the wound’s surface and are not appropriate for insertion into wound tunnels or sinus tracts.
PROPERTIES OF SADS
SADs are characterized by their remarkable capacity to absorb and retain large volumes of wound exudate, often many times their own weight. Their construction typically focuses on an inner absorptive layer and an outer protective covering. The inner core contains materials that have the ability to swell and absorb moisture without leaking or disintegrating Figure 1A-C. The interior is surrounded by a barrier layer to prevent the exudate from seeping onto the surrounding skin, thereby reducing the risk of maceration and further loss of tissue integrity Figure 1D.
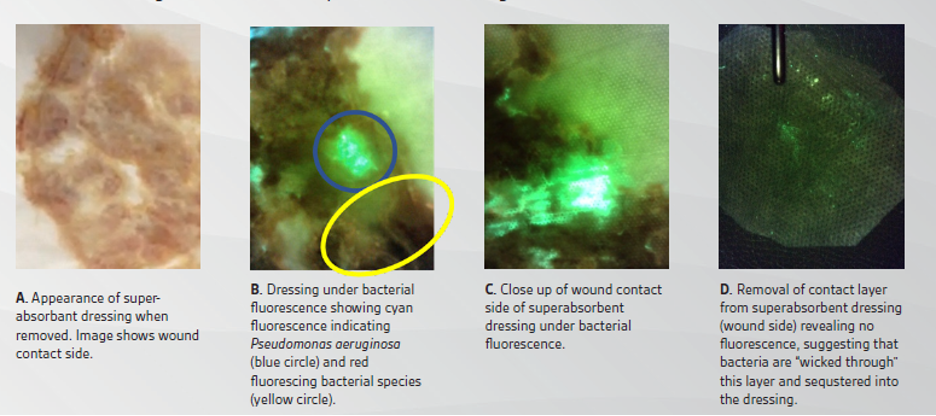
Some SADs include added features to enhance clinical utility. For example, a specially designed wicking layer positioned between the outer shell and the absorbent core enables exudate to be vertically drawn into the dressing. This mechanism prevents exudate from seeping over the edge of the wound causing maceration. In addition, the upward movement of the fluid off of the wound allows for an even distribution and subsequent gelling of the drainage throughout the entire dressing.
Wound contact layers in SADs also vary in both physical materials and the manner in which they adhere to the core. It is imperative that this contact layer be soft and non-adherent to minimize pain during dressing changes. The SAD should be designed to accommodate passthrough of exudates with different consistencies from the wound bed to the absorbent core. If these dressings are not well constructed or glued, they can split at the seams, possibly releasing their congealed, odorous contents out onto the patient. Heat-sealed edges have shown promise in meeting these requirements.
In addition to absorbing exudate, SADs also transmit moisture vapor away from the wound. This is usually not an issue in non-adherent dressing designs where the outermost layer is often similar to the contact layer. However, other wound types, including sacral or heel pressure injuries, as well as a variety of surgical wounds, require dressings with an adhesive border. In these situations, it is preferable to use an adhesive that conforms to various anatomical contours of the patient and remains secure as the dressing swells with exudate, while allowing a simultaneous transmission of moisture vapor. Figure 2 depicts a common SAD and its features.
However, not all SADs have the ability to bind the exudate. Their performance can vary depending on the amounts and types of materials used in the manufacturing process. Some SADs may allow the drainage to return to the wound and its surrounding skin when subjected to pressure. This is particularly relevant for patients with chronic wounds, where sources of pressure may not always be appreciated. For example, compression therapy, commonly used to manage venous insufficiency through wraps or garments, can exert pressure on the wound. In addition, temporary, but intense forces on the buttocks or spine during transfers with a mechanical lift from a chair to a bed can impact dressing performance. These compressive forces can limit the fluid-handling capacity of some SADs.2,3
BENEFITS OF SADS
The value of SADs lies in their ability to manage wound drainage. They are widely used across the continuum of care to manage acute, chronic wounds and those that are hard to heal.
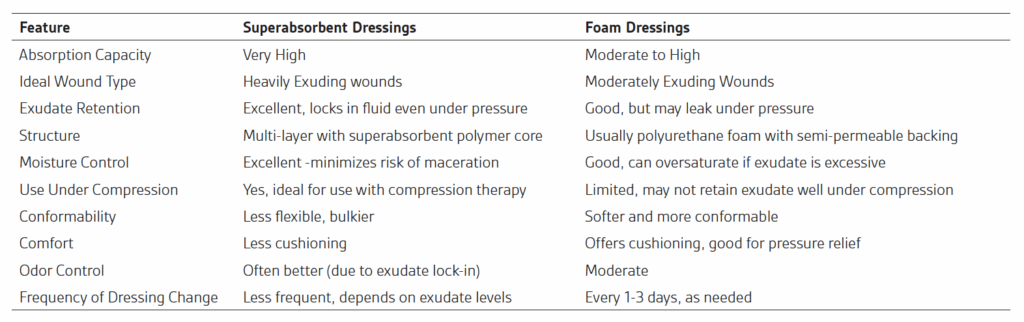
Unfortunately, many clinicians are unfamiliar with the differences between traditional foam dressings and SADs. Compared to foam dressings, SADs offer better fluid management, which can lead to fewer dressing changes and a reduction in medical waste. Table 1 compares these two dressing types.
CLINICAL APPLICATIONS
SAD can be utilized in the management of moderate to highly exuding wounds. This includes chronic wounds such as leg ulcers, pressure injury, and diabetic foot ulcers. Additionally, SADs are increasingly being adopted in acute wound management. Their versatility and high absorbency make them suitable for a variety of clinical scenarios, from traumatic injuries to surgical incisions.
TIPS FOR APPLYING SADS:
- Always cleanse the wound before applying.
- Select a dressing size that extends beyond the wound margins.
- If the dressing does not have an adhesive border, secure it with a secondary dressing or bandage.
- Change the dressing according to exudate levels or manufacturer recommendations (often every 1–3 days),though most can be left in place for up to seven days.
- Do not cut dressing.
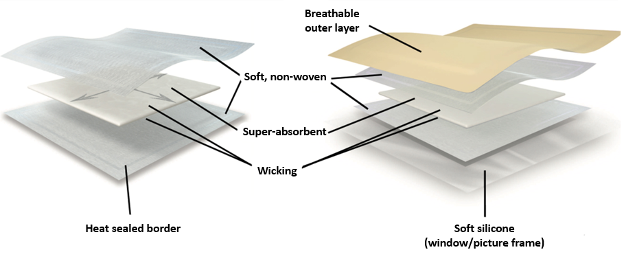
Table 1. Comparison of Superabsorbent Dressings and Traditional Foam Dressings
CONCLUSION
SADs represent a significant advancement in wound care, offering solutions for managing excessive levels of exudate while promoting an optimal healing environment. Their high absorbency, non-adherent properties, and patient comfort benefits make these dressings indispensable tools in modern wound care. Their versatility in treating both chronic and acute wounds continue to make them a crucial component of wound management strategies, improving patient outcomes and quality of life. As research into wound care materials advances, the potential for further innovations in SAD technology is immense, paving the way for even more effective treatment options.
References
- Milne C. Superabsorbent Dressing Impact on Fluorescing Bacteria in the Real-World Setting. Poster presented at Wound, Ostomy, Continence Nurses Society Virtual Conference. June 7-10, 2020. Available from: https://www.hmpgloballearningnetwork.com/site/woundcare/poster/superabsorbent-dressing-impact-fluorescing-bacteria-real-world-setting
- Veličković VM, Macmillan T, Lones E, et al. Systematic review and quality assessment of clinical and economic evidence for superabsorbent wound dressings in a population with chronic ulcers. Int Wound J. 2024; 21(3):e14750. Doi:10.1111/iwj.14750
- Ousey K, Atkin L, White R. Superabsorbent wound dressings: a review of the literature. Wounds UK.2013;9(3):52-60.
- 3M™ Kerramax Care™ Super-Absorbent Dressings Quick Guide. Wounds International .London UK; 2021 [updated 23 September 2021, cited 14 May 2025] Available from: https://woundsinternational.com/quick-guides/quick-guide-3m-kerramax-care-super-absorbent-dressings/
- Jaspar A, Balduyck B, Strapp H. 3M Kerramax Care Super-Absorbent Dressing and 3M Coban 2 Two-Layer Compression System case series supplement. Wound International, London UK; 2023 [updated 14 June 2023, cited 14 May 2025] Available from: https://woundsinternational.com/en-us/uncategorized-en-us/case-series-3m-kerramax-care-super-absorbent-dressing-and-3m-coban-2-two-layer-compression-system-2/
NOTE: Specific indications, contraindications, warnings, precautions and safety information exist for these products and therapies. Please consult a clinician and product instructions for use prior to application. Rx only.
Images courtesy of Catherine Milne, Connecticut Clinical Nursing Associates
©Solventum 2025. Solventum and the S logo are trademarks of Solventum or its affiliates.

