
Dr. Muneera is a consultant plastic & reconstructive surgeon specialized in reconstructive microsurgery and super-microsurgery. She did her plastic and microsurgery fellowship in Seoul/Korea at Asan Medical Center and is a fellow of American College of Surgeons (FACS). She is a member in many societies such as World Society for Reconstructive Microsurgery (WSRM), American Society for Reconstructive Microsurgery (ASRM), Association of Women Surgeon (AWS) and women surgeon of Kuwait (WSK). Dr. Muneera has more than 40 publications and posters and a reviewer for several journals such as Archives of Plastic Surgery. She participated in more than 50 national, regional and international conference as invited speaker and had chaired many conferences and workshops in gulf region. Dr. Muneera is a paid consultant for Solventum.
Ben_Nakhi_Current-Dialogues-in-Wound-Management_2025_Article-4
INTRODUCTION
Wound care is a complex and evolving field that demands tailored approaches based on the clinical setting, patient needs, and wound characteristics. Clinicians are challenged to continually adapt their expertise and use different strategies to promote optimal healing while addressing logistical and patient-specific factors. The availability of advanced wound care technologies has expanded the possibilities for personalized, efficient, and effective treatments.
This article presents three case studies that illustrate the varied applications of advanced wound dressings that are integrated into wound management across various clinical settings. Each case highlights the decision-making process of the treating clinicians, the specific challenges encountered, and the outcomes achieved.
CASES
Case 1: Full-thickness burn following ultrasound-assisted liposuction.
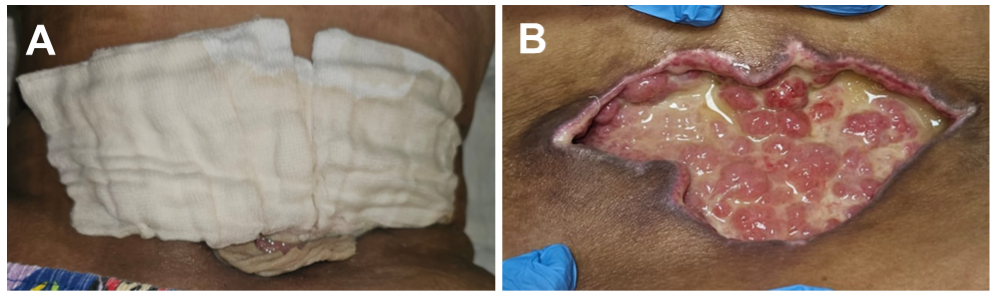
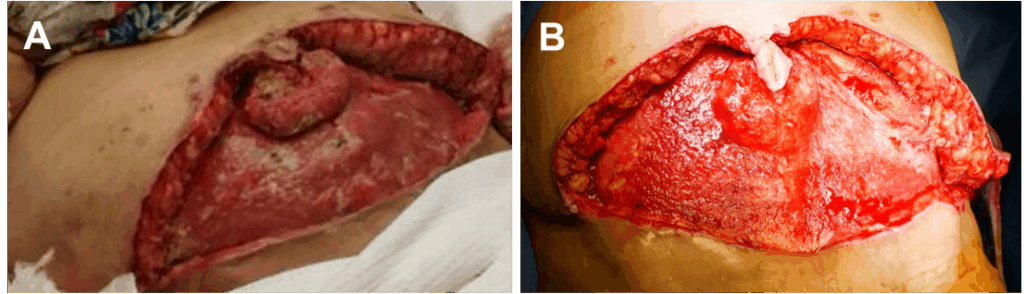
A 21-year-old woman with no prior medical or surgical history presented to the outpatient department one month after undergoing ultrasound-assisted liposuction of the abdomen, flanks and back. Clinical examination revealed a dry necrotic skin patch on the lower abdomen (Figure 1), showing early signs of separation. Initially the patient underwent bedside debridement, performed by a general surgeon and was subsequently referred to my care 10 days later for further management.

Upon re-evaluation, the wound revealed a deep, full-thickness defect with unhealthy granulation tissue at the wound bed. Current wound care was daily gauze packing dressings (Figure 2). However, it was clear that the wound was highly exudative, and simple gauze dressings were inadequate, as early maceration was observed along the wound edges (Figure 3).


Given the high level of exudate, and the patient’s upcoming exams, a one-week course of 3M™ Silvercel™ Antimicrobial Alginate Dressing was selected as a more suitable option (Figure 4).
However, the dressing was not effective for this patient, and she was admitted to the hospital for Solventum™ Veraflo™ Therapy with Solventum™ Veraflo Cleanse Choice™ Dressing use due to the presence of thick exudate and the need for wound cleansing. Therapy parameters included the instillation of 60 mL of normal saline, a 15-minute dwell time, and continuous negative pressure at -125 mmHg every 4 hours. Dressing changes occurred every 2-3 days. Due to the location of the wound and frequent blockage alarms (because of pressure from laying on the dressings), we advised the patient to lie in a prone position during the instillation phase, and alternate between lateral positions during the suction phase, avoiding the supine position entirely. After 8 days of therapy, the wound had become more shallow, with red healthy granulation tissue, indicating readiness for skin graft coverage (Figure 5).
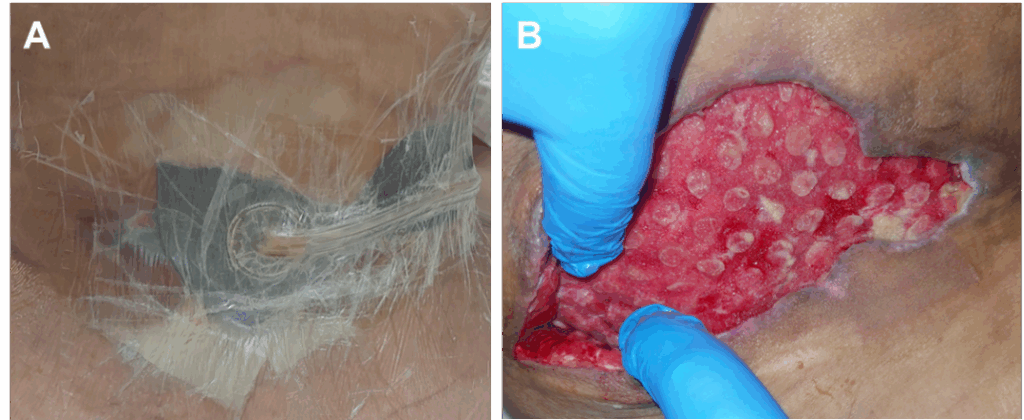
The patient underwent a split-thickness skin graft (STSG) procedure, which was bolstered with Solventum™ V.A.C.® Therapy. We applied 3M™ Adaptic™ Non-Adhering Dressing directly over the skin graft, followed by the Solventum™ V.A.C.® Granufoam™ Silver Dressing. Continuous negative pressure at -125 mmHg was utilized. The patient was discharged home with a portable Solventum™ ActiV.A.C.™ Therapy Unit. The first dressing change was performed in the outpatient department on postoperative day 7, where the lower portion of the graft appeared moist and mobile (Figure 6).

As graft lost was observed on the lower portion of the wound, 3M™ Promogran Prisma™ Collagen Matrix with ORC and Silver was applied twice weekly over a 12-day period (Figure 7).

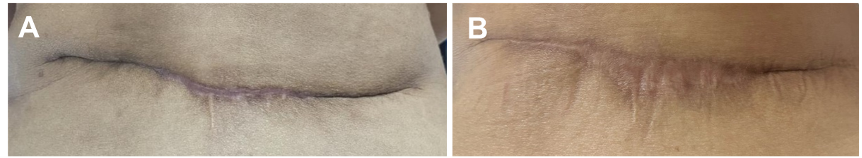
At the follow-up visit, the decision was made to continue wound care with Promogran Prisma Matrix and secondary wound dressings. Complete wound closure was observed within 3 weeks through secondary intention, with healing progressing from both the skin and skin graft edges (Figure 8).

Six months later, the patient was readmitted for skin graft scar excision and primary closure. Following a 16 kg weight loss, sufficient tissue redundancy had developed, allowing for tension-free closure (Figure 9), shown at 4 and 16 months postoperatively, respectively).
Case 2: Necrotizing fasciitis following abdominoplasty
A 58-year-old obese woman with a medical history of diabetes mellitus and hypertension presented for care 25 days after undergoing abdominoplasty abroad. Her postoperative course was complicated by lower flap gangrene, for which she underwent debridement and primary closure. She later presented with fever and an infected, dehisced lower abdominoplasty wound (Figure 10).

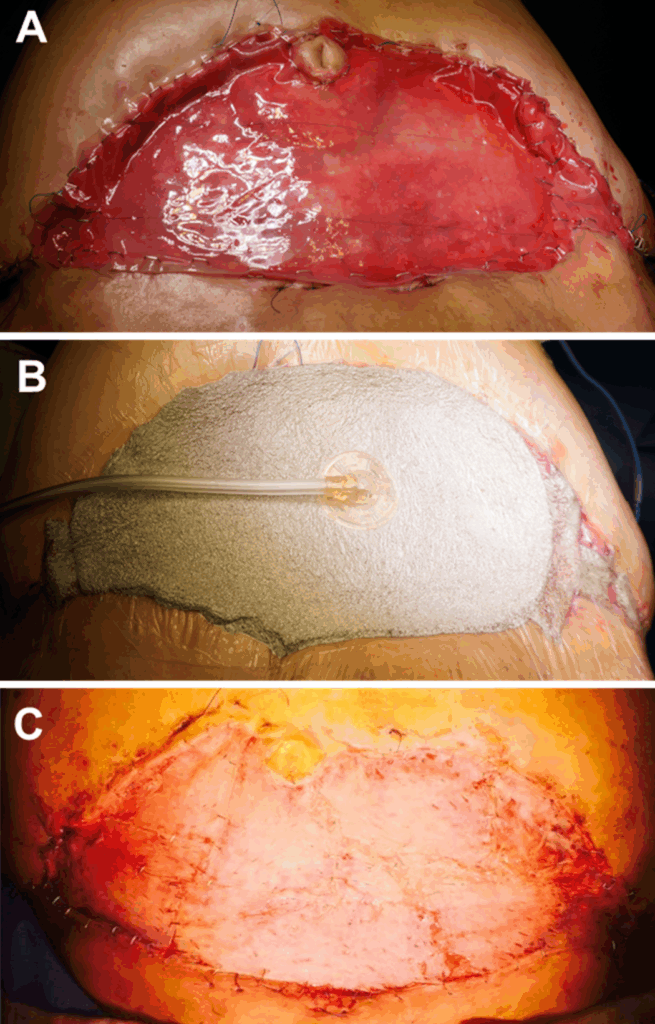
The patient was admitted and underwent two sessions of aggressive sharp surgical debridement to eradicate any remaining necrotizing fasciitis within the wound bed (Figure 11). Intravenous antibiotics were administered alongside good glycemic control to optimize uncomplicated wound healing and closure.
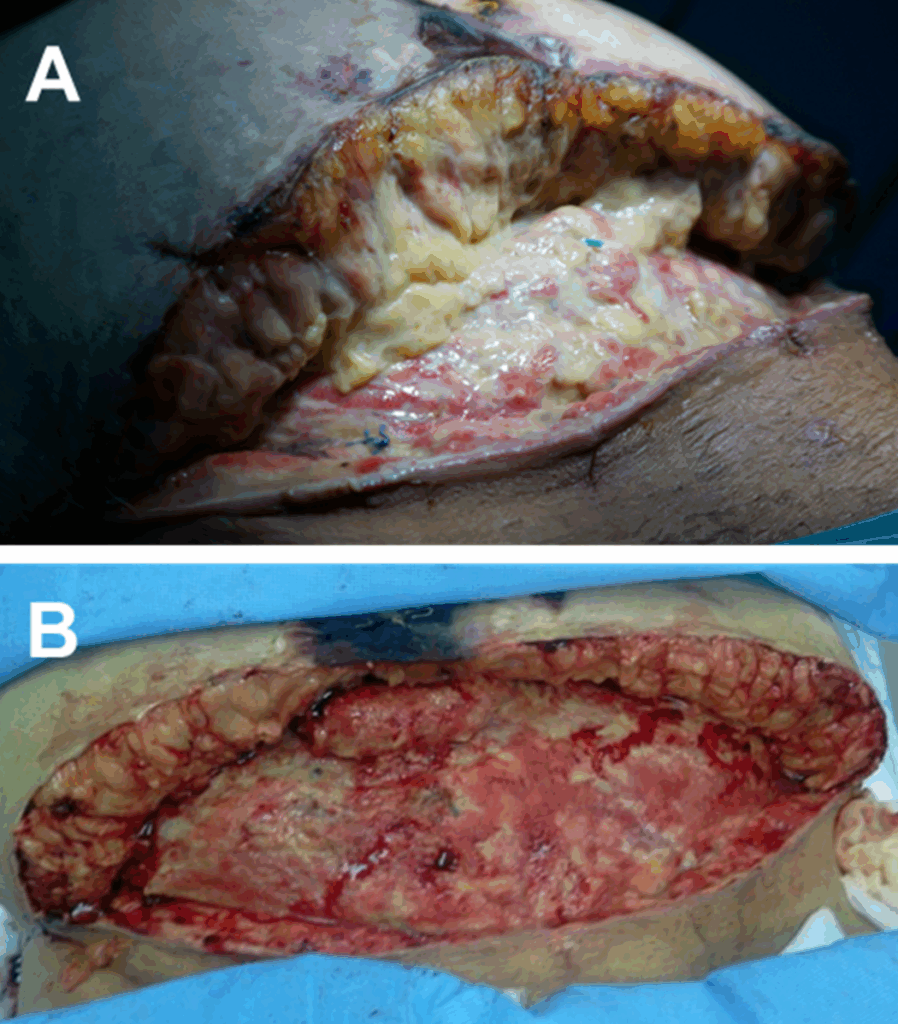
Due to the presence of a large, deep defect with a potentially contaminated wound bed, Veraflo Therapy was initiated to cleanse the wound and promote granulation tissue formation, thus optimizing wound healing. The instillation of 100 mL of an antiseptic solution, a 20-minute dwell time, and continuous negative pressure at -125 mmHg every 4 hours was utilized. Dressing changes occurred every 2-3 days. Remarkably, the wound was ready for graft coverage after just 11 days (Figure 12).
The patient underwent staged wound coverage, beginning with a dermal substitute followed by a thin STSG. V.A.C.® Therapy was applied after each stage as a bolster, using continuous negative pressure at -100 mmHg and with dressing changes once per week. V.A.C.® Therapy was used for 2 weeks after application of thedermal substitute and for 1 week after application of the split-thickness skin graft (Figure 13).
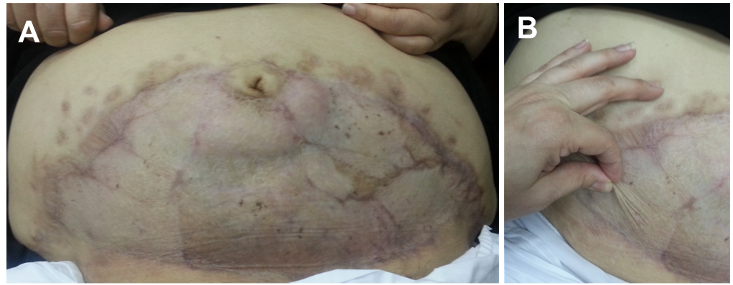
Despite the patient’s obesity and diabetes, we achieved complete (100%) take of both the dermal substitute sheet and the split thickness skin graft, aided by the use of V.A.C.® Therapy. The negative pressure wound therapy ensured optimal contact between the wound bed and the graft by removing exudate and infectious material, reducing edema, promoting perfusion, and drawing wound edges together. The use of Veraflo Therapy and V.A.C.® Therapy enabled closure of this extensive, infected woundin less than one month. In addition, fewer dressing changes wererequired, and no complications were observed. At the 7-yearfollow-up, the patient exhibited pliable skin and an acceptableaesthetic result (Figure 14).
Case 3: Post hysterectomy infected wound necrosis
A 69-year-old morbidly obese woman with multiple medical illnesses presented on postoperative day 5 following a hysterectomy, with dehiscence of the Pfannenstiel scar. Examination revealed necrosis of the upper wound edge and deep fat necrosis was observed inside the wound bed (Figure 15).

The patient underwent sharp surgical debridement followed by the application of Veraflo Therapy. To minimize potential bleeding issues, therapy was applied 48 hours after surgical debridement to ensure appropriate hemostasis had been achieved. We selected the Veraflo Cleanse Choice Dressing, in conjunction with Veraflo Therapy to initiate hydromechanical removal of infectious material, non-viable tissue, and wound debris. The rational for avoiding the operating room and having the patient undergo further sharp surgical debridement was because of the exposure of the rectus sheath, as additional surgical debridement could have led to evisceration of abdominal contents (Figure 16).

Following five applications of Veraflo Therapy (40 ml instillation of an antiseptic solution, with a 15-minute dwell time and -125 mmHg negative pressure applied every 6 hours), the wound was ready for coverage using either advancement flaps or an STSG (Figure 17).

The patient refused further surgical intervention and opted for conservative management using advanced dressings aiming for secondary intention wound closure. Upon discharge, the patient was provided with a portable ActiV.A.C. Therapy Unit set to intermittent mode at -100 mmHg for a total of 24 days. Dressing changes were performed approximately every 3 days. Negative pressure was discontinued and Silvercel Dressing applied with dressing changes every 2 days. Once Silvercel Dressing use was discontinued, foam dressings were utilized with dressing changes every 3 days until complete wound closure was achieved (Figure 18). The entire journey to achieve complete wound healing was completed on an outpatient basis over three and a half months, without any complications, hospital readmissions, or need for return to the operating room.

References
Patient data and images courtesy of Muneera Ben Nakhi, MD, KSB, FACS, MRCS (Ireland)
NOTE: Specific indications, contraindications, warnings, precautions and safety information exist for these products and therapies. Please consult a clinician and product instructions for use prior to application. Rx only.
As with any case study, the results should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
© Solventum 2025. Solventum, and S logo are trademarks of Solventum or its affiliates. 3M is a trademark of 3M. All other trademarks are owned by their respective owners.

