
Dr. Jayesh B. Shah is an award-winning wound care and hyperbaric physician in active clinical practice. He is Columbia trained and certified in Wound Management, Board Certified in Undersea and Hyperbaric Medicine and Internal Medicine. He is a Fellow of Undersea and Hyperbaric Medicine, American College of Physicians and American College of Clinical Wound Specialist. He is a superb educator with extensive speaking experience. He is the President of South Texas Wound Associates, where he provides clinical wound care services in San Antonio since past 22 years. He is the President of TIMEO2 Healing Concepts, LLC, which provides consulting and education services in wound care and hyperbaric medicine; Medical Director of Wound Healing Center at Northeast Baptist Hospital and Mission Trail Baptist Wound Healing Center in San Antonio, Texas; Past President of the American College of Hyperbaric Medicine; Past President American Association of Physicians of Indian Origin; Past President of Bexar County Medical Society; Current Board of Trustees Member of Texas Medical Association, Current American Medical Association Delegate from Texas; Current Board Member and Regional Director of International Skin Tear Advisory Panel. Dr. Shah is a paid consultant for Solventum.
Shah_Current-Dialogues-in-Wound-Management_2025_Article-5
Venous leg ulcers (VLUs) are prevalent affecting 1-2% of the U.S. population.1 Risk factors include trauma, obesity, venous insufficiency, previous deep vein thrombosis, advanced age, smoking, diabetes, and other metabolic issues.2 These ulcers often become chronic and may require extensive surgical and medical treatment, often involving multiple procedures and operations over many months. Standard treatment often entails surgical or enzymatic debridement, compression, and treating both the underlying cause and associated risk factors. A product that has become a mainstay for VLU treatment is 3M™ Coban™ 2 Two-Layer Compression System. These compression wraps are designed to help reduce edema while remaining secure and comfortable during patients’ daily activities. A study reported that 72% of patients preferred the two-layer Coban 2 Compression System over a four-layer compression therapy with reduced slippage and comparable healing rates.3 Other studies have shown that Coban 2 compression system is cost-effective and slightly improved healing rates compared to other wrapping options.4,5 The current standard management of VLUs varies. Ulcers should be cleansed at each dressing change and debridement, either surgical or enzymatic, should be performed depending on the complexity of the ulcer.6 Additionally, enzymatic debridement should be performed with every subsequent dressing change. Systemic antibiotics are indicated when the ulcer is infected.6 A dressing should be applied to manage exudate and help maintain a moist wound environment. If ulcers have failed to respond to more conservative treatment options within 4-6 weeks, skin grafting with compression stockings should be considered. Compression therapy is appropriate for most cases of leg ulcers, unless arterial insufficiency is evident.6 Coban 2 compression system is an effective option for compression in these clinical scenarios. Three case studies are presented showing the successful treatment of large, complicated, chronic VLUs managed with the Coban 2 compression system along
with standard of care practices, including skin grafts, surgical and enzymatic debridement, and antibacterial foam. Each case involved multi-month treatment until the wounds were considered clinically healed. Care was delivered in an outpatient clinical setting, along with procedures, such as skin grafts and surgical debridement, which were performed in the operating room. Prior to Coban 2 compression system application, all patients underwent vascular assessments, including a mini-vascular exam and measurement of the Ankle-Brachial Pressure Index (ABPI); each patient had an ABPI greater than 0.8.
CASE STUDIES
Case 1: Chronic Lymphedema and Statis Dermatitis in a Patient with Obesity
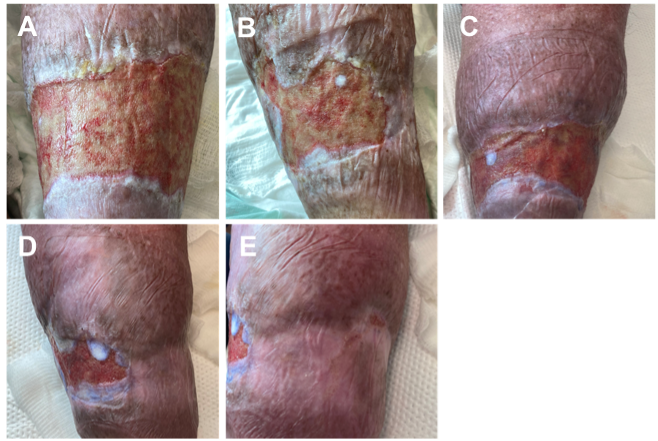
A 46-year-old female with morbid obesity and a medical history of hypertension, presented with a chronic lymphedema-related wound that had started with trauma seven years earlier. Despite multiple evaluations at various wound centers and several unsuccessful treatment attempts, the ulcer persisted. A biopsy of the lesion confirmed the presence of stasis dermatitis. The patient declined surgical debridement and was instead managed with a regimen that included antibacterial foam, enzymatic debridement with collagenase, and serial compression bandaging with Coban 2 compression system. Dressing changes were performed on a weekly basis. Coban 2 compression system was selected for its ease of application and its ability to provide consistent compression therapy. Progression of wound healing throughout the treatment course is shown in Figure 1.
Case 2: Traumatic Leg Injury in an Elderly Male on Anticoagulation
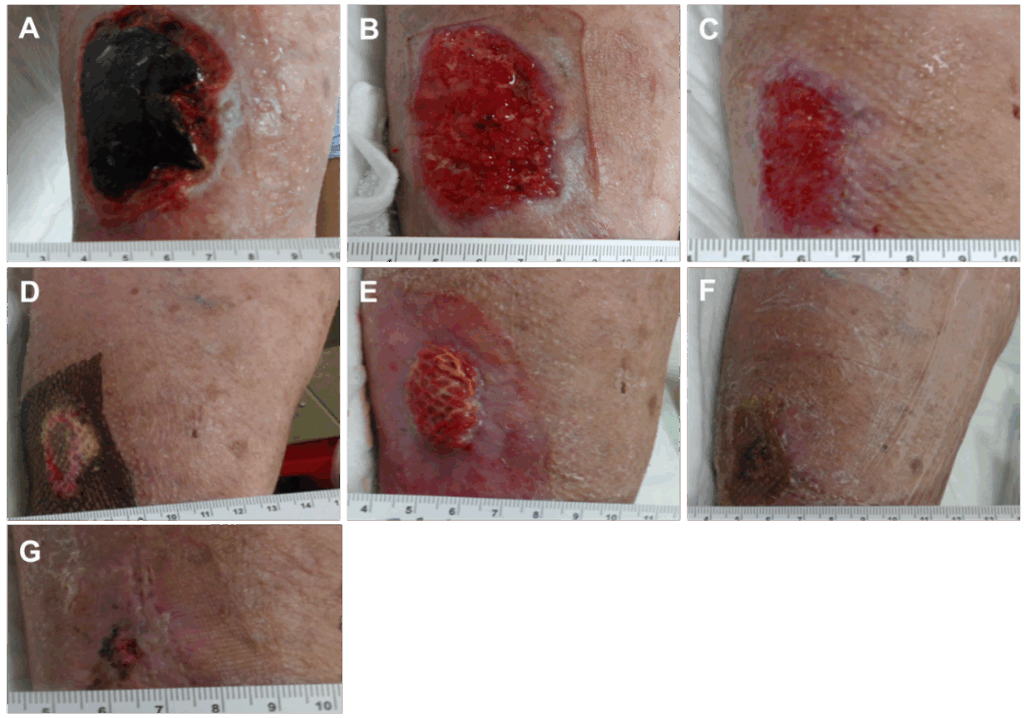
An 80-year-old male presented with a traumatic injury to the left leg sustained during a lawn mower accident (Figure 2a). Previous medical history included venous insufficiency, atrial fibrillation treated with warfarin, chronic obstructive pulmonary disorder, asthma, congestive heart failure, hypertension, hypothyroidism, and a history of prostate and lung cancer. The resulting chronic wound was treated with a combination of treatments, including surgical debridement, enzymatic debridement, antibacterial foam for antibacterial coverage, and Coban 2 compression system. Dressing changes were performed weekly. Figure 2 shows the progression of wound healing throughout the treatment course. Three months after treatment initiation, the wound had fully epithelialized and was subsequently transitioned to compression stocking therapy.
Case 3: Chronic Wound in a Middle-Aged Female with Immunosuppression
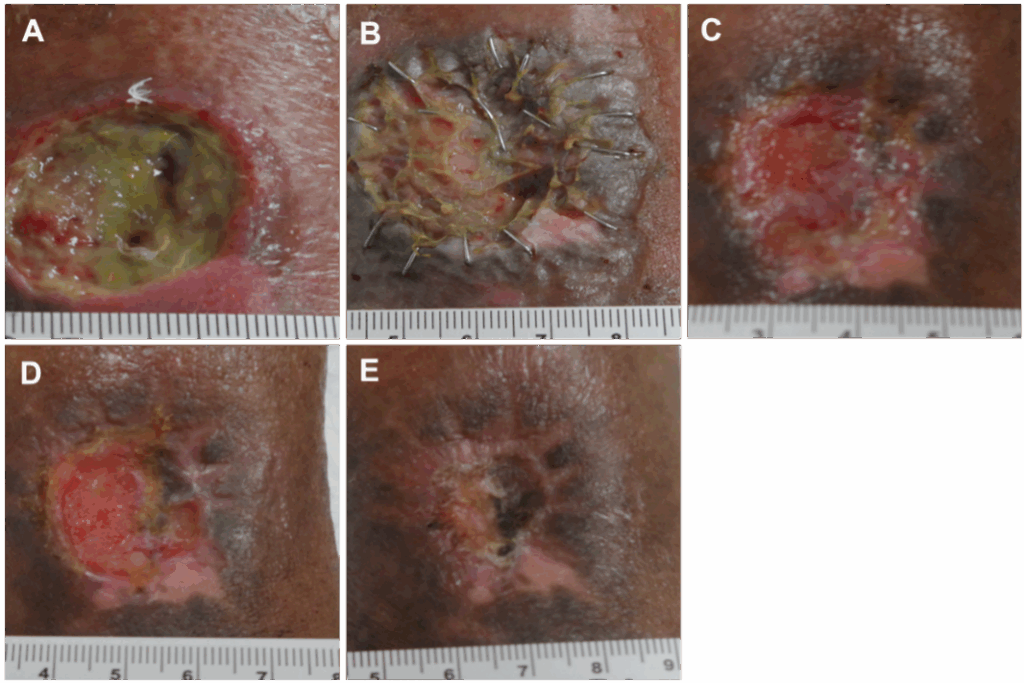
A 55-year-old female presented with an open chronic wound on the left lower leg (Figure 3A). A biopsy of the wound confirmed vasculitis as the underlying pathology. Patient’s medical history included rheumatoid arthritis treated with immunosuppressive therapy and corticosteroids. Wound healing progressed throughout the treatment course of debridement, skin graft application, and use of Coban 2 compression system (Figures 3B-D). Coban 2 compression system was utilized to manage edema. A split-thickness skin graft (STSG) procedure was performed 45 days after presentation. A non-adherent dressing and secondary dressing were used to cover the newly placed graft. Dressing changes occurred once per week. As partial take of the graft occurred, a second skin graft procedure using an STSG and human skin allograft was performed approximately 3 months after presentation. The wound was fully healed 120 days after the second graft procedure.
The combined use of debridement techniques with various advanced modalities, paired with consistent edema control using Coban 2 compression system was successful in promoting healing of chronic VLUs in these three patients. The compression and coverage provided by the compression system were essential for ensuring proper long-term placement of the antibacterial foam and contributed to reducing local edema. Its ease of use and ability to remain in place for continued periods without adjustment contributed to patient compliance with treatment. However, Coban 2 compression system should not be used in patients with arterial insufficiency, as its compression may impede arterial blood flow. As such, all patients should undergo a mini-vascular exam and a measurement of ABPI prior to starting compression therapy. Coban 2 compression system provides compression for patients with ABPI greater than or equal to 0.8.
Coban 2 compression system has emerged as an effective and patient-friendly compression system for managing leg ulcers, especially VLUs. Multiple studies have shown that it matches or outperforms traditional multi-layer systems in terms of healing outcomes, slippage control, patient comfort, and adherence.4-6 Coban 2 compression system should be considered a first-line compression therapy for leg ulcers across acute care and community-based wound management settings.
References
- Schul MW, Melin MM, Keaton TJ. Venous leg ulcers and prevalence of surgicallycorrectable reflux disease in a national registry. J Vasc Surg Venous Lymphat Disord. 2023;11(3):511–516. doi:10.1016/j.jvsv.2022.11.005
- NHS. Causes venous leg ulcer UK: NHS; 2022: [updated 16 November 2022]. Available from: https://www.nhs.uk/conditions/leg-ulcer/causes/.
- Moffatt CJ, Edwards L, Collier M, Treadwell T, Miller M, Shafer L, et al. A randomised controlled 8-week crossover clinical evaluation of the 3M Coban 2 Layer Compression System versus Profore to evaluate the product performance in patients with venous leg ulcers. Int Wound J. 2008;5(2):267–279. doi:10.1111/j.1742-481X.2008.00487.x
- Guest JF, Gerrish A, Ayoub N, Vowden K, Vowden P. Clinical outcomes and cost-effectiveness of three alternative compression systems used in the management of venous leg ulcers. J Wound Care. 2015;24(7):300, 302–305, 307–308. doi:10.12968/jowc.2015.24.7.300
- Guest JF, Fuller GW, Vowden P. Clinical outcomes and cost-effectiveness of three different compression systems in newly-diagnosed venous leg ulcers in the UK. J Wound Care. 2017;26(5):244–254. doi:10.12968/jowc.2017.26.5.244
- O’Donnell TF, Jr., Passman MA, Marston WA, Ennis WJ, Dalsing M, Kistner RL, et al. Management of venous leg ulcers: clinical practice guidelines of the Society for Vascular Surgery ® and the American Venous Forum. J Vasc Surg. 2014;60(2 Suppl):3s–59s. doi:10.1016/j.jvs.2014.04.049
Patient data and images courtesy of Jayesh B. Shah, MD.
NOTE: Specific indications, contraindications, warnings, precautions and safety information exist for these products and therapies. Please consult a clinician and product instructions for use prior to application. Rx only.
As with any case study, the results should not be interpreted as a guarantee or warranty of comparable results. Individual results may vary depending on the patient’s circumstances and condition.
©Solventum 2025. Solventum, and S logo are trademarks of Solventum or its affiliates. 3M and the 3M logo are trademarks of 3M. All other trademarks are owned by their respective owners.

