Dr. Fernandez is a Clinical Assistant Professor of Surgery and Family Practice at the University of Texas Health Center at Tyler. He is also an Attending Teaching Staff in the Division of Surgery for Mother Frances Health System and East Texas Medical Center in Tyler. Dr. Fernandez obtained his residency training at Loyola University, the University of Illinois, the University of Chicago and Northwestern University, Chicago, Illinois, with special training in Trauma and Burns at Kings County Hospital, SUNY Down State System, Brooklyn, New York, NY. He is well published in multiple areas of research both in peer-reviewed articles and book chapters, and has made numerous oral and poster presentations at national and international conferences.
The art of wound healing always involves treating the whole patient. At times, wounds develop in patients who have poor nutrition, immune compromising diseases such as cancer or HIV, as well as co-morbidities involving obesity, diabetes and age. Fournier’s Gangrene is a rare, but life threatening disease, first described by Baurienne in 17641 and Avicenna in 1877.2 It is named after a French venereologist, Jean Alfred Fournier, who in 1883 described a rapidly progressive gangrene of the penis and scrotum without apparent cause in five previously healthy young men. Necrotizing fasciitis was first described by a Confederate Army surgeon, Joseph Jones, during the US Civil War.3 Necrotizing fasciitis has been classified into 3 types: Type 1 polymicrobial; Type II Group A Streptococcal; Type III –gas gangrene or clostridial myonecrosis.
Fournier’s gangrene is a type of necrotizing fasciitis (usually polymicrobial in nature, Type I Necrotizing Fasciitis) commonly affecting the perineum and lower abdominal wall of males and, to a lesser extent, females of all ages.5-6Classically, it is described as an idiopathic process with a predilection for patients who are immune-compromised, such as the elderly, with diabetes, on chronic corticosteroid therapy and/or chronic alcohol abuse; however, it can also be found in otherwise healthy individuals and in women and children who have been exposed to insect bites, trauma, burns, peri-rectal diseases and infections.2,7-8 The site of initial infection is usually located in the genitourinary tract, lower gastrointestinal tract, or skin and is caused by traumatic disruption of the protective skin envelope.
Fournier’s gangrene is a mixed infection caused by both aerobic and anaerobic bacterial flora. The development and progression of the gangrene is often fulminating and can rapidly cause multiple organ failure and death.6 Because of potential complications, it is important to diagnose the disease process as early as possible; although antibiotics and aggressive debridement have been broadly accepted as the standard treatment, the death rate remains high.
I present the following case to discuss diagnosis, treatment and treatment outcome.
CLINICAL CASE
This 45-year-old Caucasian female, who was admitted in severe sepsis and septic shock, was found to have a severe necrotizing fasciitis infection of the perineal area, the right thigh, and the right lower abdomen. She was seen in the emergency room, where she underwent a rapid sequence intubation, administration of broad-spectrum antibiotics and aggressive resuscitation. The patient was in acute diabetic ketoacidosis, acute respiratory failure and developed subsequent adult respiratory distress syndrome (ARDS).
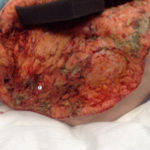
The patient was taken emergently to the operating room where she underwent aggressive radical debridement of her skin, subcutaneous tissue, fascia and muscle of the right thigh, perineum, bilateral inguinal areas, right gluteal area, and lower abdomen, with approximately 1500 cm2 of tissue being resected. (Fig 1)
The patient underwent multiple surgical re-evaluations under general anesthesia, with continued aggressive debridement and application of V.A.C.® Therapy (KCI, an Acelity Company, San Antonio, TX). (Fig 2) Due to adult respiratory distress syndrome, the patient underwent placement of a percutaneous tracheostomy tube and a percutaneous endoscopic gastrostomy (PEG) tube for ongoing nutritional management.
On hospital day 70, the patient’s wound underwent placement of ACell MatriStem® MicroMatrix™ (Acell Inc., Columbia, MD) to assist with skin grafting. (Fig 3) This was bolstered with a V.A.C.® Therapy Dressing. The patient subsequently improved and was discharged to a rehab facility on hospital day 96. (Fig 4)
CONCLUSION
The mainstay for treatment of Fournier’s gangrene entails an aggressive approach with frequent and often extensive soft tissue debridements with delayed wound coverage achieved once the infection has been controlled. The anatomy in this region (lower abdomen, perineal area) can make traditional dressing placement difficult, if not impossible, and traditional dressings are often ineffective in this area of a patient’s anatomy. Negative pressure wound therapy devices have proven beneficial in patients with large soft-tissue defects in the lower abdomen, perineum and scrotum. It is this author’s opinion that KCI V.A.C.® Therapy is the most effective of all of the alternatives available and represents the state-of-the-art in the application of negative pressure therapy. Certain techniques facilitate the application of V.A.C.® Therapy and have proven beneficial in these patients. As further clinical experience grows, V.A.C.® Therapy will become a more frequently utilized therapeutic regimen for the treatment of genitourinary wounds and many other challenging complex wounds.
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
References
1.Corman JM. Classic articles in colonic and rectal surgery. Dis Colon Rectum. 1988. 31:984-8.
2.Nathan B. Fournier’s gangrene: a historical vignette. (Letter). Can J Surg 19984172 [PubMed]
3.Quirk WF Jr, Sternbach G. Joseph Jones: infection with flesh eating bacteria. J Emerg Med. 1996 Nov-Dec. 14(6): 747-53.
4.Bratdorff D, Roemmele J. National Necrotizing Fasciitis Foundation (NNFF) 1997-2009. Available at http://www.nnff.org. Accessed: April 17, 2013.
5.Thwaini A, Khan A, Malik A, et al. (2006). “Fournier’s gangrene and its emergency management.” Postgrad Med J 2006;82(970):516–9.
6.Wagner. et al. Is Intensive Multimodality Therapy the Best Treatment for Fournier Gangrene? Evaluation of Clinical Outcome and Survival Rate of 41 Patients. Surgical Infections. 2011 12(5):379-383.
7.Smith GL, Bunker CB, Dineen MD. Fournier’s gangrene. Br J Urol 1998;81347–355.355
8.Ekelius L, Björkman H, Kalin M, Fohlman J. Fournier’s gangrene after genital piercing. Scand J Infect Dis. 2004; 36(8):610-2.