
A transplant from North Carolina to Minnesota in 2013. Michael Kalos graduated as a nurse in 2002. He started in the ICU and spent most of his early career as an “in-house” float at the University of North Carolina Chapel Hill, NC. He received his CWOCN training from Emory University in Atlanta, Ga in 2010. He completed his DNP-NELI degree from Medical University of South Carolina in 2020.
Michael Kalos is currently employed by Regions Hospital in St. Paul, MN. He has been part of the inpatient CWOCN consult services since 2014. Since this time was able to implement a skin integrity and pressure injury campaign that led to a 69% reduction in reported HAPIs in 2018. Michael established a Skin Wound Resource RN (SWRRN) program, spearheaded the change-out of support surfaces in all Med-Surg and ICU units and is currently working to have units electronically complete monthly skin surveys.
Michael Kalos has published abstracts and presented posters for WOCN Society’s annual conference and Wild on Wounds.
Michael Kalos spoke nationally for CMS Webinar on Wounds in 2019 and locally for the MHA in 2016. Mr. Kalos is a consultant for 3M.
Kalos_Current-Dialogues-in-Wound-Management_2021_Article-17
BACKGROUND
Within a midwestern metropolitan Level I trauma center, the certified wound, ostomy, and continence nurse (CWOCN) services set out to implement use of a novel hybrid drape for 3M™ Veraflo™ Therapy. Currently, an acrylic drape is used with the negative pressure wound therapy systems; however, removal of the acrylic drape can be painful. The new silicon and acrylic 3M™ Dermatac™ Drape provides the ability to maintain a seal, has increased flexibility and is easier to remove.1,2
With the increased need to maintain a moist wound environment and promote granulation tissue development along with the removal of infectious material and debris, the use of Veraflo Therapy remains a clinically important aspect of wound care. Wound locations such as the lower and upper extremities have traditionally allowed for less challenging utilization of Veraflo Therapy. More challenging anatomical locations including the groin, ischial tuberosity, and sacral coccyx have required multiple barrier rings, skin preparation, and paste to maintain a tight seal when traditional acrylic drape was utilized. Veraflo Therapy applications across such anatomically challenging areas may benefit from the use of Dermatac Drape. Several cases will follow to highlight our use and experience with Veraflo Therapy and Dermatac Drape in anatomically difficult areas.
CASE #1
A 64-year-old individual was found by friends at home after a suspected fall and was last known to be healthy seven days prior. The patient’s previous medical history included alcohol abuse, hypotension, acute kidney injury, failure to thrive, malnutrition, and COPD with hypoxia.
Upon examination, areas of non-viable tissue had begun to take hold on the sacral, coccyx, bilateral lower extremity posterior heels, and right ischial tuberosity encompassing the posterior thigh, trochanter and buttocks. The prognosis was poor, and the patient declined initiation of comfort care. Conservative care was then started due to poor nutrition, failure to thrive, and hemodynamic instability. The patient’s overall care was further complicated by frequent and loose fecal incontinence which created incontinence-associated dermatitis resulting in broken skin.
On Day 35, it was determined that the patient had stabilized with proper nutrition and physical therapy. This wound measured 27 cm x 15 cm x 0.1 cm and had an area of non-viable tissue present. Since the patient was not a surgical candidate, our center decided to initiate Veraflo Therapy with 3M™ V.A.C. Veraflo Cleanse Choice™ Dressing (Figure 1). Hypochlorous acid solution (42 mL) was instilled into the wound bed with a 5 minute dwell time, followed by 2.5 hours of continuous negative pressure at -125 mmHg. Due to the anatomically challenging areas involved with this case, a Dermatac Drape was placed along with a barrier ring due to areas of moist skin, limited range of motion, and limited skin real estate. Initiation of therapy demonstrated a positive seal and no leakage of the instillation fluid. Veraflo Therapy was utilized for 11 days with dressing changes every 2-3 days (Figure 2). After 11 days, the patient was discharged to a transitional care unit (TCU) with 3M™ V.A.C.® Therapy, Dermatac Drape, and dressing changes every 2-3 days.

CASE #2
A 63-year-old individual presented with left lower extremity ulcers and diabetic ulcers from poor atrial perfusion. The patient’s history included right lower extremity osteomyelitis with below the knee amputation (BKA), hypertension, type I diabetes, poor nutrition, and opioid abuse. We were initially requested to assess and provide treatment for the left lower extremity. However, the patient’s right lower extremity BKA wound was non-healing and orthopedics requested assistance.
At the time of assessment, the patient was at post-operative day 2 from a debridement. The certified wound ostomy continence nurse assessed the wound and determined that Veraflo Therapy with V.A.C. Veraflo Cleanse Choice Dressing would be the best option to provide additional wound cleansing. Given the nature of the wound and the amount of ‘roundness’ up and over the wound edges, Dermatac Drape was chosen for its flexibility and skin friendly properties.
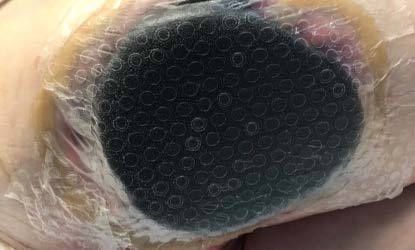
Veraflo Therapy with V.A.C. Veraflo Cleanse Choice Dressing was initiated to an open area that measured 15.6 cm x 25.1 cm x 0.4 cm. Hypochlorous acid solution (30 mL) was instilled into the wound bed with a 5 minute dwell time, followed by 3 hours of continuous negative pressure at -125 mmHg. The wound edges were unstable and contained significant edema. The therapy was continued for 20 days with dressing changes every 2-3 days (Figure 3). No accessories were required to maintain the seal. After 20 days, the patient was discharged to TCU. Veraflo Therapy was discontinued and V.A.C.® Therapy was initiated with Dermatac Drape and dressing changes every 2-3 days.

CASE #3
A 35-year-old individual with a history of incomplete quadriplegia from a gunshot wound 18 years prior, depression, and substance abuse presented at our facility with a sacral unstageable pressure injury measuring 12.6 cm x 17 cm x 0.1 cm. The patient was not a surgical candidate at the time and our team worked with the acute care surgery team and developed a plan of care. The patient’s wound was well demarcated and displayed an area of non-viable tissue. There was no erythema or induration at the time of the initial assessment. Given the nature of the wound and the location around the anus through the buttocks it was decided that Veraflo Therapy with V.A.C. Veraflo Cleanse Choice Dressing and utilization Dermatac Drape was warranted. Hypochlorous acid solution (40 mL) was instilled into the wound bed with a 5 minute dwell time, followed by 3 hours of continuous negative pressure at -125 mmHg. Accessories to maintain the seal included skin prep, a moldable ring, and paste. The patient’s Veraflo Therapy was bridged from the anterior thigh alternating between left and right at each dressing change. There were no issues with the seal or any leaking of installation fluid. The patient remained on therapy for 15 days, during which time dressings were changed every 2-3 days (Figure 4). The patient was turned and repositioned often by the nursing staff and the Dermatac Drape held its position without loss of adhesion. After 15 days of Veraflo Therapy, the patient was discharged to a TCU with V.A.C.® Therapy using Dermatac Drape with dressing changes every 2-3 days.

CONCLUSION
Our CWOCN service set out to utilize the novel hybrid acrylic – silicone drape (Dermatac Drape) with Veraflo Therapy and V.A.C. Veraflo Cleanse Choice Dressing. These three cases highlight that difficult, time consuming, and anatomically challenging locations with creases, folds, and limited skin real estate are common and require novel therapies in order to achieve complete wound management. The Dermatac Drape and Veraflo Therapy with V.A.C. Veraflo Cleanse Choice Dressing were critical in supporting wound management and contributing to optimal patient outcomes in the three cases described here. In these 3 patients, the Dermatac Drape easily conformed to the difficult anatomical areas without compromising the negative pressure and instillation seal. The use of Veraflo Therapy with V.A.C. Veraflo Cleanse Choice Dressing allowed for wound cleansing and the removal of infectious material and debris in patients with anatomically difficult wounds and/or were not candidates for surgical intervention. CWOCN services will continue to utilize Dermatac Drape as the primary drape for all Veraflo Therapy patients in our facility.
References
Patient data and images courtesy of Michael D. Kalos, DNP, RN, CWOCN.
As with any case study the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
NOTE: Specific indications, contraindications, warnings, precautions and safety information exist for these products and therapies. Please consult a clinician and product instructions for use prior to application. Rx only.
©2022 3M. All rights reserved. 3M and other marks shown are marks and/or registered marks. Unauthorized use prohibited. Used under license in Canada. All other marks are property of their respective owners.
References
1. Fernandez LG, Matthews MR, Benton C, et al. Use of a novel silicone-acrylic
drape with negative pressure wound therapy in anatomically challenging wounds. Int Wound J. 2020.
2. Greenstein E, Moore N. Use of a Novel Silicone-Acrylic Drape With Negative Pressure Wound Therapy in Four
Patients With Periwound Skin Breakdown. Wounds. 2021.

