Liz McElroy is a Nurse Practitioner in Wound, Ostomy, and Continence Care at the Reading Health System in West Reading, PA. She graduated from Gwynedd Mercy University with her MSN in Adult Nurse Practitioner in 2009, became a Certified Wound Specialist (CWS) in 2010, and certified in Wound, Ostomy, and Continence (CWOCN) in 2012. She serves as an in-patient wound, ostomy, and continence specialist for a 647-bed Level II Trauma Center. She focuses on care of the perioperative, post-operative, cardiac and critical care patients, with an interest in nursing and physician education and V.A.C. VERAFLO™ Therapy. She also has two years experience in an outpatient wound care center prior to her acute care position.
McElroy_Innovations in Addressing Non-Viable Tissue_2018_Volume 1_Issue 1
Often times, we as clinicians are aware of what the best treatment for a diagnosis would be, but patient factors stand as a barrier to utilizing the treatment recommended using evidence-based medicine. We are all given a wound care tool box that we can pull from. Within the last year, clinicians were given a new tool for their wound care toolbox, the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing Kit that is used with V.A.C. VERAFLO™ Therapy. The dressing’s unique three-layer design facilitates removal of thick wound exudates, such as thick fibrin (wet slough), and other infectious material, to provide a wound cleansing option for clinicians when surgical debridement must be delayed or is not possible or appropriate.
Recently, I was consulted to see a 75-year-old female with a past medical history of obstructive sleep apnea, Type 2 diabetes mellitus with hyperglycemia, hypothyroidism, hypertension, and anemia, Stage IV endometrial cancer with peritoneal carcinomatosis status post recent surgery by Gynecologic Oncology for tumor debulking and total abdominal hysterectomy with bilateral salpingo-oophorectomy. She was diagnosed in April with Stage IV endometrial cancer and was scheduled for tumor staging surgery in early May. At the time of surgery, she was found to have over 3.5 L of ascites in her abdomen. She had a primary closure utilizing staples. Her recovery from surgery was slow but uneventful. She was transferred to an acute care rehabilitation hospital on postoperative Day 11. However, during the next weeks the patient’s condition deteriorated due to the increasing development of ascites, with respiratory and kidney complications. On day 25 she was FIGURE 1. Initial WOCN wound evaluation on postoperative Day 28. V.A.C.® Therapy was applied with V.A.C® GRANUFOAM SILVER™ Dressing.readmitted to the acute care hospital with shortness of breath and an acute kidney injury. The surgical team ordered V.A.C.® Therapy at that time. The nursing staff applied the therapy, and then the wound, ostomy, and continence nurse (WOCN) was consulted for further management. On postoperative Day 28, the WOCN saw the patient to reapply V.A.C.® Therapy. The inferior aspect of the wound was open, and the superior aspect of the wound was closed with steristrips. The dehisced portion measured 13.2 x 4.1 x 4cm with over half of the wound with non-viable tissue in the base. A cyanoacrylate sealant was applied to the periwound, and then a V.A.C.®GRANUFOAM SILVER™ Dressing was applied. V.A.C.® Therapy continued over the weekend at -125mmHg continuous pressure
(Figure 1). The surgical team was aware of all the non-viable tissue. The patient was on bilevel positive airway pressure therapy with no escalation of care. She currently was not a candidate for surgical debridement in the operating room or at the bedside. Her pain was controlled, requiring additional narcotic coverage for dressing changes.
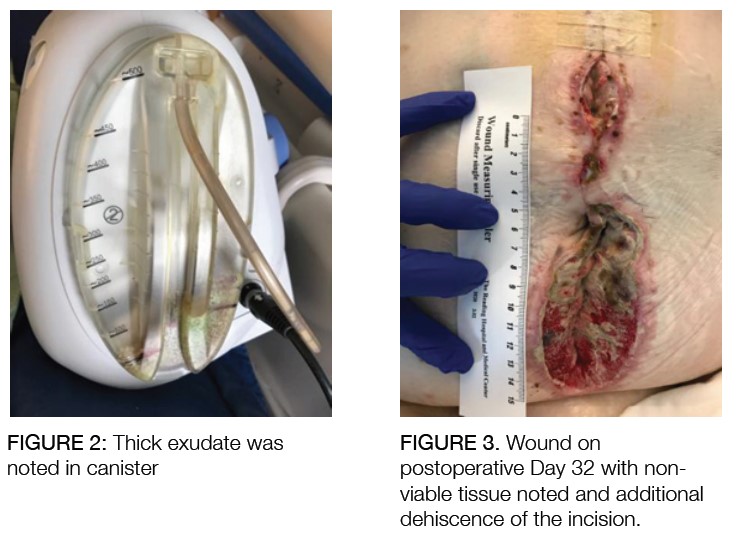
On postoperative Day 32, the WOCN came back to evaluate the patient and found thick exudate in the canister (Figure 2).
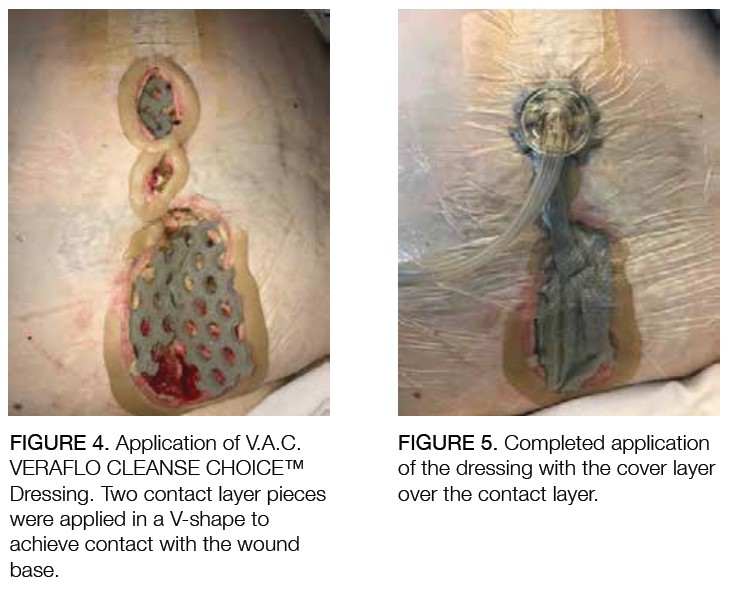
The WOCN decided to explore additional options in her toolkit and decided to utilize the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing with V.A.C. VERAFLO™ Therapy. Upon assessment of her abdomen, the patient had an extension of her midline dehiscence (Figure 3).
The V.A.C. VERAFLO CLEANSE CHOICE™ Dressing was applied to the wound. Barrier rings were used on the peri-wound skin to aid in seal adherence and prevent any moisture-associated skin damage to the peri-wound (Figures 4 and 5).
The fill assist function of V.A.C. VERAFLO™ Therapy was used, and 20 mL of normal saline was instilled into the dressing before it pooled in the inferior aspect. The V.A.C. ULTA™ Negative Pressure Wound Therapy System was reprogrammed to instill 16mL of normal saline with a dwell time of 10 minutes, and the cycle was set for negative pressure at -125 mmHg every 30 minutes. There were no leaks, and the patient tolerated the therapy over the next two days. The patient underwent routine dressing changes every 48-72 hours (Figures 6 and 7).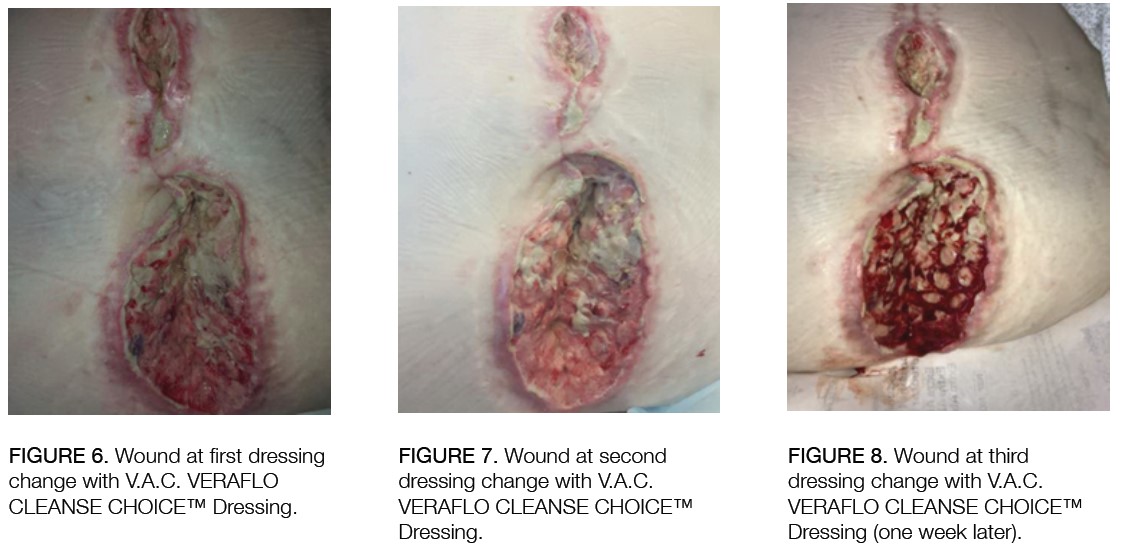 One week after the start of V.A.C. VERAFLO™ Therapy using the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing, the patient had robust granulation tissue in the wound base (Figure 8). The patient was then transferred to a skilled nursing facility with V.A.C.®Therapy. She has not been re-admitted since.
One week after the start of V.A.C. VERAFLO™ Therapy using the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing, the patient had robust granulation tissue in the wound base (Figure 8). The patient was then transferred to a skilled nursing facility with V.A.C.®Therapy. She has not been re-admitted since.
The V.A.C. VERAFLO CLEANSE CHOICE™ Dressing provided the wound care team with a non-surgical option for improving the tissue quality of her wound in a controlled environment. The patient was palliative in the sense that no aggressive therapies were to be implemented, and her focus was on quality of life, which included pain control, infection management and discharge from the acute care facility. We were able to address her palliative needs while using this innovative therapy. For this patient, and for many more patients to come, this new therapy is a game changer for our wound care toolbox.