
Dr. Subhas Gupta is the Chairman of the Department of Plastic Surgery at Loma Linda University in Southern California where he holds the academic rank of Professor and is the director of research. He is an innovative plastic surgeon who holds a PhD in Medical Informatics focused on the introduction of new technologies to clinical care. He is the director of the Loma Linda University Soft Tissue Reconstruction Team and directs a bio-investigative cell biology and wound healing laboratory.
Gupta_Current-Dialogues-in-Wound-Management_2019_Article_2
Plastic surgeons have used the reconstructive ladder for four decades as a guiding principle for wound reconstruction with the aim of restoring form and function to patients. This includes healing by less complex methods such as secondary intention and direct tissue closure, as well as more complex methods such as local tissue transfer, distant tissue transfer, and free tissue transfer (Figure 1).
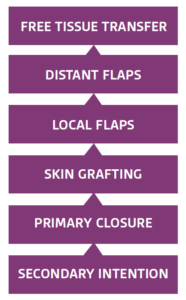
The reconstructive ladder represents the closure options available for wounds, with closure being achieved using the simplest effective technique possible.1 The wound-closure ladder concept has an extensive history having first been described in ancient Egyptian medical texts. As medical advances occurred, reconstruction, flaps, and skin grafting were added to the reconstruction ladder.2
Options for reconstruction have grown. Advanced technologies, such as hyperbaric oxygen therapy, skin substitutes, and negative pressure wound therapy, have been developed that offer additional “rungs” on the reconstructive ladder to incorporate a more holistic, patient-based approach with improved outcomes and cost efficiencies such as allowing care to be transitioned from an inpatient site to lower cost settings. The traditional reconstructive ladder does not account for these new paths of care. In contrast, the modern, holistic reconstructive ladder is wound and patient-based, focusing on affordability, sustainability, time effectiveness, and patient quality of life. As such, it is important to consider the patient, the defect, aesthetics, and any potential impediments to healing along with the economics of the care delivered and the setting of the care.
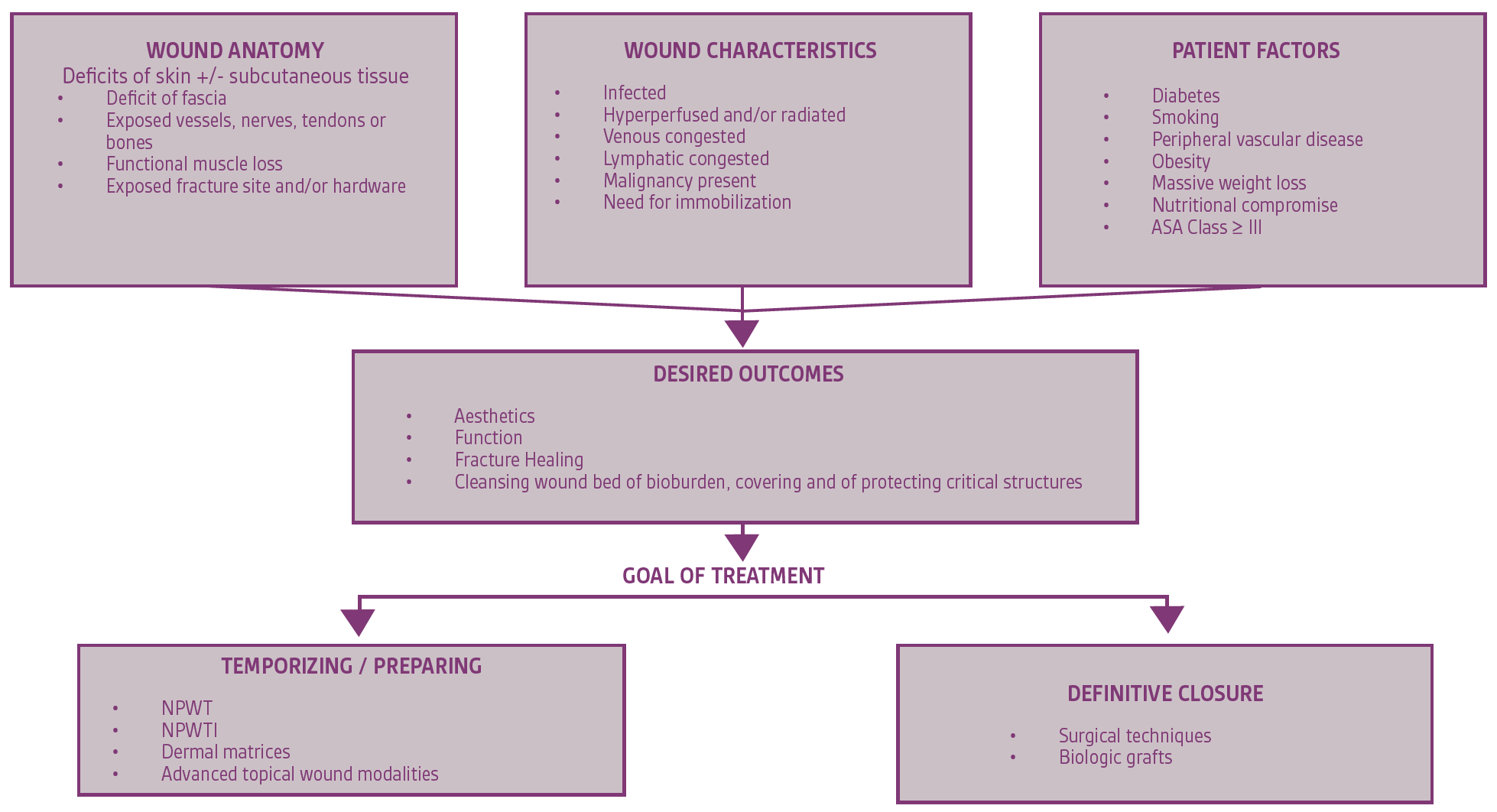
In order to establish a practical, up-to-date reconstructive pathway, innovative methods of wound reconstruction were assessed for their benefit to surgical reconstruction, considering the clinical effectiveness, innovation, and practicality of each considered method.3,4 To best utilize the reconstructive pathway (Figure 2), treatment modalities should be selected based on wound anatomy, wound characteristics, and patient factors. The goal of treatment (closure versus temporizing care to bridge to closure), helps provide context to determine the setting for care delivery and should be considered in the overall care plan.
Most methods of reconstruction can be managed in any of the care settings once initial wound healing and stabilization has occurred. The optimal care setting for wound patients depends upon several factors including pain control, infection management, frequency of reassessment, complexity of dressing changes, and geographical location (remote versus urban settings).
Determining the appropriate care setting is a choice between acute care hospitals, nursing facilities (skilled nursing, long term acute acute care, rehabilitation centers), or home.
To illustrate the use of the updated reconstructive ladder, we present a case study following wound care after a traumatic injury. A 68-year-old diabetic female in acute heart failure presented with a traumatic degloving injury to the right lower leg (Figure 3).

(14 x 11-cm2)
Her wound measured 14 x 11-cm2 with surrounding cellulitis noted. There was insufficient tissue to allow for local tissue closure, and her increased risk for perioperative complications did not permit immediate flap closure. The wound was surgically debrided, and a dermal regeneration template was placed along with negative pressure wound therapy (NPWT) after 48 hours of hospital admission for intravenous antibiotics (Figure 4).

The remainder of this patient’s care was performed on an outpatient basis using home health nursing for NPWT dressing changes. A second ambulatory procedure was performed 12 days later when a stromal vascular fraction of autologous fat was injected to the deepest contour deformity of the wound (Figure 5) and NPWT reapplied. Complete wound closure was noted on post-operative day 46. The wound remained closed without complications 5 months after the patient’s initial injury (Figure 6). In this case study, patient comorbidities and wound characteristics directed the initial use of NPWT rather than surgical closure. Signs of wound healing with the presence of an anatomical defect lead to the decision to utilize autologous fat grafting rather than full surgical closure. As the wound continued to resolve, no further reconstruction techniques were needed.


To truly deliver optimal patient outcomes, clinicians need to be keenly aware of all factors that contribute to wound healing (both patient-driven and otherwise). The evolution of the reconstructive ladder to include holistic care components can provide guidance for treatment plans and care setting decisions facing health care providers today. With the push for more effective and holistic models of care, the updated reconstructive pathway may help achieve the goal of improved wound outcomes while examining the economics of care, assessing care efficiency, and applying innovative technologies in order to better serve patients.
References
- Simman R. Wound closure and the reconstructive ladder in plastic surgery. J Am Col Certif Wound Spec. 2009;1(1):6–11. doi:10.1016/j.jcws.2008.10.003
- Gottlieb LJ, Krieger LM. From the Reconstructive Ladder to the Reconstructive Elevator. Plast Reconstr Surg. 1994;93(7):1503-1504. doi:10.1097/00006534-199406000-00027.
- Janis JE, Kwon RK, Attinger CE. The New Reconstructive Ladder: Modifications to the Traditional Model. Plast Reconstr Surg. 2011;127:205S-212S.
- Rahmati M., Pennisi CP, Budd E, Mobasheri A, Mozafari M. Biomaterials for Regenerative Medicine: Historical Perspectives and Current Trends. In: Turksen K, ed. Cell Biology and Translational Medicine, Volume 4. Advances in Experimental Medicine and Biology, vol 1119. Springer Nature, Switzerland;1-19.
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
Specific indications, contraindications, warnings, precautions and safety information exist for KCI products and therapies. Please consult a clinician and production instructions for use prior to applications. This material is intended for healthcare professionals.

