Dr. Fernandez is a Clinical Professor of Surgery and Family Practice at the University of Texas Health Center at Tyler. Dr. Fernandez obtained his residency training at Loyola University, the University of Illinois, the University of Chicago and Northwestern University, Chicago, Illinois, with special training in trauma and burns at Kings County Hospital, SUNY Down State System, Brooklyn, New York. He is well published in multiple areas of research both in peer-reviewed articles and book chapters, and has made numerous oral and poster presentations at national and international conferences.
Fernandez_Current Dialogues in Wound Management_2020_Article_5
The traditional surgical approach to managing abdominal injuries has several specific goals:1
1) to assess the extent of trauma
2) repair the damaged organs
3) close the abdomen in one definitive procedure
Recent advances in critical surgical care and the development of the damage control surgery paradigm has led to the more liberal use of temporary abdominal closure (TAC) methods to manage the open abdomen (OA) when closure is not possible.2-4 Damage control surgery concepts, and modern negative pressure wound therapy (NPWT)/TAC methods, have been very successful in the trauma patient setting.5-7 This experience has been translational, and these methods have been extended and applied successfully in the management of the septic patient.8-11
The surgeon who is faced with these often-difficult cases will require a comprehensive knowledge of this complex subject. The purpose of this article is to provide guidance to the acute care and general surgeon on the use of OA negative pressure therapy (OA-NPT; ABTHERA™ Open Abdomen Negative Pressure Therapy for OA management). Clinical recommendations on managing the OA, and a case study demonstrating OA management using OA-NPT have been included.
INDICATION: THE OPEN ABDOMEN
The indications for OA include patients at risk of developing intra-abdominal hypertension (IAH) as seen in Figure 1.9-12 The OA technique is used to prevent the development of abdominal compartmental syndrome (ACS) and all involved in the care of critically ill patients should be aware of its incidence, how to identify high-risk patients, and how to prevent and treat IAH and ACS.5-12;12 The management of ACS is based on goal-directed therapy, which relies on quick diagnosis and rapid surgical decompression, while actively optimizing the patient’s physiologic response to result in the earliest definitive closure possible.11 In order to achieve these goals, a combination of therapeutic interventions, including NPWT and dynamic closure, may be used to minimize complications associated with the OA, such as incisional hernia (IH) or enteroatmospheric fistula (EAF).9-11;13

TAC With Negative Pressure Wound Therapy – ABTHERA ADVANCE™ Open Abdomen Dressing:
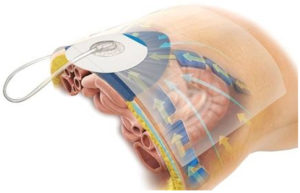
The ABTHERA ADVANCE™ Open Abdomen Dressing, when used with a compatible therapy unit, forms a temporary abdominal closure system (Figure 2) that helps surgeons more effectively manage a challenging OA and helps achieve primary fascial closure.6-8
The ABTHERA ADVANCE™ Dressing features the ABTHERA ADVANCE™ Perforated Foam. The unique configuration of the foam is designed to collapse medially when negative pressure is applied, actively drawing wound edges together.

POTENTIAL ADVANTAGES:
The ABTHERA ADVANCE™ Dressing is designed to:
• Actively remove fluid, helping to reduce edema14;15 (Figure 3)
• Provide medial tension, which helps minimize fascial retraction and loss of domain 15
• Help protect abdominal contents from the external environment
• Provide separation between the abdominal wall and viscera, protecting abdominal contents
• Allows for rapid access for re-entry and does not require sutures for placement
The ABTHERA ADVANCE™ Dressing utilizes proprietary SENSAT.R.A.C.™ Technology, which facilitates fluid removal from the dressing and monitors negative pressure during therapy.
TECHNIQUE AND TIPS:
APPLICATION:
The application of the ABTHERA ADVANCE™ Dressing is, for the most part, similar to the technique used in the ABTHERA™ Open Abdomen Negative Pressure Therapy Dressing (Figure 4). The visceral protective layer is placed between the viscera and abdominal wall, tucked into the pericolic gutters. The ABTHERA ADVANCE™ Dressing is then cut to size and placed over the visceral protective layer, followed by application of the drape over the periwound skin and ABTHERA ADVANCE™ Dressing. A 2.5 cm hole is cut in the drape and the interface pad is placed directly over the hole.

Given our early clinical experience and to maximize the biomechanical properties of the device, the author suggests some minor modifications in how the newly configured perforated foam layer is applied. This is illustrated in the following case presentation.
CLINICAL CASE:
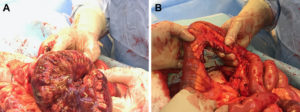
A 21-year-old male, motor vehicle accident /rollover victim, presented to the emergency department with mild tachycardia, transient and recurrent hypotension, a seatbelt sign, and diffuse abdominal pain/distention, with a superficial laceration to the left arm. The patient was immediately taken to the operating room where intraoperative findings included a necrotic sigmoid colon, a bucket handle injury of the small bowel with diffuse intraabdominal content edema, consistent with early abdominal compartment syndrome (Figure 5).
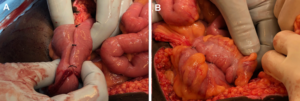
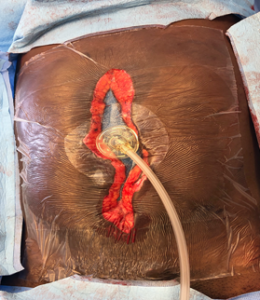
Due to the patient’s physiologic condition, damage control surgery (DCS) with small and large bowel prepared for side-to-side functional end-to-end, stapled anastomosis was performed (Figure 6).
To place the ABTHERA ADVANCE™ Dressing using the Fernandez Tuck Technique, the visceral protective layer is placed between the viscera and abdominal wall and tucked into the pericolic gutters. The ABTHERA ADVANCE™ Dressing is cut to size and placed over the visceral protective layer with a 2-3 cm circumferential overlap beneath the peritoneal lining of the abdominal wall. The drape is then applied over the periwound skin and the ABTHERA ADVANCE™ Dressing. A 2.5 cm hole is cut in the drape and the interface pad is placed directly over the hole. This was done to take advantage of the biomechanical properties of the OA NPT and maximize the medial migration of the fascia (Figure 7).

The patient was reexamined within 48 hours. Inspection of the intraabdominal contents showed viable bowel and no delayed injury. Abdominal washout with Vashe® Wound Solution (Urgo Medical, Fort Worth, TX) and a side-to-side/functional end-to-end, linear-cutter stapled small bowel, and colo-colonic anastomosis was performed. Debridement and drainage of the subcutaneous (Morel-Lavallée lesion) seat belt injury was performed with primary abdominal wall closure and placement of a PREVENA PEEL & PLACE™ Incision Management System-20cm.
CONCLUSION:
The ABTHERA ADVANCE™ Dressing is easy to apply, and its handling characteristics are similar to the standard ABTHERA™ Dressing. Based on early clinical experience, it is the author’s opinion that when the ABTHERA ADVANCETM Dressing foam is tucked 2-3 cm in the subfascial plane, this may assist in medial migration of the midline wound fascial edges in a more effective manner compared to the standard ABTHERA™ Therapy technique. Further studies will be required to fully assess the use of the ABTHERA ADVANCE™ Dressing. This device is an additional tool that may prove to be effective in achieving a higher rate of primary abdominal wound closure in open abdomen patients.
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
NOTE: Specific indications, contraindications warnings, precautions and safety information exist for these products and therapies. Please consult a clinician and product instructions for use prior to application. Rx only.
References
- De Waele JJ, Kaplan M, Sugrue M, Sibaja P, Bjorck M. How to deal with an open abdomen? Anaesthesiology Intensive Therapy 2015;47(4):372-378. doi:10.5603/AIT.a2015.0023.
- Rotondo MF, Schwab CW, McGonigal MD et al. ‘Damage control’: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma 1993;35(3):375-383.
- Kaplan M, Banwell P, Orgill DP et al. Guidelines for the Management of the Open Abdomen. Wounds 2005;17(Suppl1):S1-S24.
- Fabian TC. Damage control in trauma: laparotomy wound management acute to chronic. Surg Clin North Am 2007;73-93.
- Demetriades D. Total management of the open abdomen. Int Wound J 2012;9(Suppl 1):17-24.
- Cheatham ML, Demetriades D, Fabian TC et al. Prospective Study Examining Clinical Outcomes Associated with a Negative Pressure Wound Therapy System and Barker’s Vacuum Packing Technique. World J Surg 2013;37(9):2018-2030.
- Frazee RC, Abernathy SW, Jupiter DC et al. Are commercial negative pressure systems worth the cost in open abdomen management? J Am Coll Surg 2013;216(4):730-733.
- Atema JJ, Gans SL, Boermeester MA. Systematic Review and Meta-analysis of the Open Abdomen and Temporary Abdominal Closure Techniques in Non-trauma Patients. World J Surg 2015;39(4):912-925. doi:10.1007/s00268-014-2883-6.
- Fernandez LG. Management of the open abdomen: clinical recommendations for the trauma/acute care surgeon and general surgeon. Int Wound J 2016;13(Suppl 3):25-34. doi:10.1111/iwj.12655.
- Coccolini F, Biffl W, Catena F et al. The open abdomen, indications, management and definitive closure. World Journal of Emergency Surgery 2015;10:32. doi:10.1186/s13017-015-0026-5.
- Coccolini F, Roberts D, Ansaloni L et al. The open abdomen in trauma and non-trauma patients: WSES guidelines. World Journal of Emergency Surgery 2018;13:7. doi:10.1186/s13017-018-0167-4.
- Reintam Blaser A, Regli A, De Keulenaer B et al. Incidence, Risk Factors, and Outcomes of Intra-Abdominal Hypertension in Critically Ill Patients-A Prospective Multicenter Study (IROI Study). Crit Care Med 2019;47(4):535-542. doi:10.1097/CCM.0000000000003623.
- Miller RS, Morris JA, Diaz JJ, Herring MB. Complications after 344 damage-control open celiotomies. J Trauma 2005;59(6):1365-1374.
- Schmidt M, Hall C, Mercer D, Kieswetter K. Novel foam design actively draws wound edges together under negative pressure: benchtop and pre-clinical assessment [abstract]. Presented at the SAWC Fall 2018 Meeting, November 2-4, 2018, Las Vegas, Nevada 2018.
- Schmidt M, Mercer D, Kieswetter K. Novel Foam Design Actively Draws Wound Edges Together Under Negative Pressure (NP): Pre-Clinical Assessment. Presented at the 41st Annual John A Boswick Burn & Wound Care Symposium, February 2-7, 2019, Maui, HI 2019.
- Roberts DJ, Jenne CN, Ball CG et al. Efficacy and safety of active negative pressure peritoneal therapy for reducing the systemic inflammatory response after damage control laparotomy (the Intra-peritoneal Vacuum Trial): study protocol for a randomized controlled trial. Trials 2013;14:141. doi:10.1186/1745-6215-14-141.
©Copyright 2020 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. PRA-PM-US-02367 (04/20).

