
Dr. Robert Snyder is a podiatrist with over 30 years of experience; his practice is limited to wound management and limb preservation. He is Professor and Director of Clinical Research and Fellowship Director at Barry University SPM. Dr. Snyder is certified in foot and ankle surgery by the American Board of Podiatric Surgery and is also a board certified wound specialist. Dr. Snyder is immediate past-president of the Association for the Advancement of Wound Care and past-president of the American Board of Wound Management. In addition to his doctorate, he holds an MSc in Wound Healing and Tissue Repair from Cardiff University. Dr. Snyder has published several book chapters over 125 papers in peer reviewed and trade journals on wound care and has been a principal investigator on more than 30 randomized controlled trials.
Snyder_Current Dialogues in Wound Management_2015_Volume 1_Issue 4
ACUTE WOUND INFECTION
Acute wound infections, that is, wounds of short duration, such as several days, are common and occur in patients after surgery, lacerations, or trauma with delayed treatment; in contaminated sites after long operative procedures, necrotic tissue or foreign bodies; and in burns. The annual incidence of surgical site infections in the United States ranges from 2 to 5% of the more than 30 million patients undergoing surgical procedures each year.1Symptoms are often accompanied by fever, chills, nausea, vomiting, and an elevated white blood cell count with a left shift. Absent underlying comorbidities, patients with acute wound infections readily respond to local incision and drainage, if necessary; topical antimicrobials; and systemic antibiotics when required. Patients usually exhibit classic signs and symptoms of infection including heat, pain, redness, swelling, and loss of function (Figure 1). Clinicians should diagnose infection based on the presence of at least two classic symptoms or signs of inflammation or purulent secretions.
 Figure 1. Classic signs and symptoms of infection.
Figure 1. Classic signs and symptoms of infection.
However, many patients with diseases, such as diabetes, peripheral arterial disease, and anemia, among others, often fail to mount a physiologic response to infection. More subtle symptomology, such as wound deterioration and pain in an otherwise painless foot, are often the only signs present; some patients with diabetes may exhibit no signs at all. The only clue to the presence of infection may be an open wound that fails to respond to various therapeutic regimens (Figure 2).
Clinicians tend to undertreat infection and overtreat inflammation in immunocompromised patients. Treatment of acute infection is often delayed until it has seeded to bone and contiguous structures, possibly leading to sequelae, such as sepsis, limb loss, and death. There is broad support for the conclusion that acute infection may predispose to later onset of chronic diseases, which are likely caused by chronic microbial infection.5 Mild or asymptomatic infections sometimes trigger damaging immune system responses that are associated with development of chronic disease.
 Figure 2. Infection or inflammation?
Figure 2. Infection or inflammation?
The most common organism observed in wounds of patients with diabetes is Staphylococcus aureus.7 A study by Repine et al found that killing of S. aureus by neutrophils was higher in untreated patients with acute bacterial infection compared with the same patients after antibiotic treatment or uninfected controls.8 Neutrophils from patients with diabetes, however, did not increase their bactericidal activity in response to infection as much as neutrophils from patients without diabetes. These results support the hypothesis that defective neutrophil bactericidal activity may contribute to the increased susceptibility to bacterial infection seen in patients with diabetes.
Infectious Disease Society of America clinical practice guidelines for the diagnosis and treatment of foot infections in patients with diabetes can assist the clinician in determining appropriate treatment algorithms and situations in which these patients should receive treatment.2 The guidelines also state that every wound in a patient with diabetes should be considered potentially infected.
CHRONIC WOUND INFECTION
Individuals with chronic wounds, that is late, chronic, fastidious, or latent wounds often have at least one underlying disease.9The result is delayed healing, poor response to topical and systemic therapies, and high recurrence rates. Infection is usually observed in necrotic tissue, in wounds present for at least 2 to 4 weeks or even months, and in wounds near sites of potential contamination; these infections tend to proliferate when primary symptomology is not cleared by an adaptive immune response.10 Bacterial replication in chronic infection is likely less rapid than in acute infection, but bacteria involved in long-term infections can persist for extended periods of time and continue to shed planktonic, or free-swimming, bacteria and biologically active molecules into the host during the course of the persistent infection.
ACUTE OR CHRONIC?
Recent papers suggest that bacteria can choose either to cause an acute infection, growing and spreading rapidly in the host, or, alternatively, to adopt a chronic, biofilm infection strategy. Biofilm is difficult to culture, tolerant of biocides and antibiotics, and capable of regenerating.12 In response to uncharacterized signals, bacteria may initiate an acute infection using factors, such as type III secretion system, a protein appendage found in several gram-negative bacteria, and various toxins. Alternatively, bacteria may establish a chronic biofilm-like infection, wherein bacterial cells are surrounded by a matrix displaying properties, such as antibiotic resistance. Unfortunately, the mechanisms explaining why common bacteria, such as Pseudomonas, create acute infections or biofilms are still unknown.
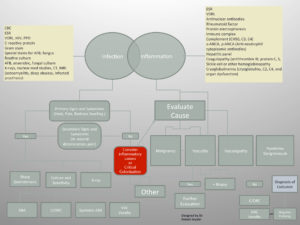 Figure 3. Algorithm to assist in differentiating between infection and inflammation.
Figure 3. Algorithm to assist in differentiating between infection and inflammation.
CONCLUSION
In summary, although differences exist between acute and chronic infections, the lines are blurred, and clinical diagnosis is often difficult, especially in the immunocompromised host. The clinician must be diligent in evaluationto help ensure an appropriate diagnosis and a good clinical outcome (Figure 3).
References
1.Surgical Site Infection (SSI) Event. Available at http://www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf Accessed 15 Aug 2015
2.Lipsky BA, Berendt AR, Cornia PB, et al. 2012 Infectious Disease of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54:132-73.
3.Gardner SE, Frantz RA, Doebbeling BN. The validity of clinical signs and symptoms used to identify localized chronic wound infection. Wound Repair Regen. 2001;9(3):178-86.
4.Serena TE, Hanft JR, Snyder RJ. The lack of reliability of clinical examination in the diagnosis of wound infection: preliminary communication. Int J Low Extrem Wounds. 2008;7(1):32-5.
5.Finch CE, Crimmins EM. Inflammatory exposure and historical changes in human life-spans. Science. 2004;305:1736-9.
6.Lober B. Infectious causes of chronic illness: an overview. Microbe. 2012;February.
7.Snyder R, Kirsner RS, Warriner RA, et al. Consensus recommendations on advancing the standard of care for neuropathic foot ulcers in patients with diabetes. Ostomy Wound Manage. 2012;56(Suppl 4):S1-S24.
8.Repine JE, Clawson CC, Goetz FC. Bactericidal function of neutrophil from patients with acute bacterial infections and from diabetics. J Infect Dis. 1980;142(6):869-75.
9.Lai ST Treatment of severe acute respiratory syndrome. Eur J Clin Microbiol Infect Dis. 2005; 24:583-91.
10.Persistent Infections Lecture Series. Spring 2012.
11.Zegans ME, Becker HI, Budzik J, et al. The role of bacterial biofilms in ocular infections. DNA Cell Biol. 2002;21:415-20.
12.Kania RE, Lamers GE, Vonk MJ, et al. Demonstration of bacterial cells and glycocalyx in biofilms on human tonsils. Arch Otolarngol Head Neck Surg. 2007;133(2):115-21.
13.Furkawa S, Kuchma SL, O’Toole GA. Keeping their options open: acute versus persistent infections. J Bacteriol. 2006;188(4):1211-7.

