Dr. Fernandez is a Clinical Assistant Professor of Surgery and Family Practice at the University of Texas Health Center at Tyler. He is also an Attending Teaching Staff in the Division of Surgery for Mother Frances Health System and East Texas Medical Center in Tyler. Dr. Fernandez obtained his residency training at Loyola University, the University of Illinois, the University of Chicago and Northwestern University, Chicago, Illinois, with special training in Trauma and Burns at Kings County Hospital, SUNY Down State System, Brooklyn, New York, NY. He is well published in multiple areas of research both in peer-reviewed articles and book chapters, and has made numerous oral and poster presentations at national and international conferences.
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
A BRIEF REVIEW OF ACUTE COMPARTMENT SYNDROME
Compartment syndrome was first described by Richard von Volkmann first in 1881 1.There are two main types of compartment syndrome: acute and chronic
Acute compartment syndrome (ACS) occurs when the tissue pressure within a closed muscle compartment exceeds the perfusion pressure and results in muscle and nerve ischemia. It typically occurs subsequent to a traumatic event, most commonly after prolonged vascular obstruction (arterial, venous or both) due to either intrinsic peripheral vascular disease or extrinsic (compressive) pressure, blunt trauma (e.g. a closed extremity fracture, although it can also be occasionally present in an open extremity fracture as well)
The events leading to acute compartment syndrome begin when the tissue pressure exceeds the venous pressure and impairs blood outflow. Lack of oxygenated blood and accumulation of waste products result in pain and decreased peripheral sensation secondary to nerve irritation7-8. These various etiologic events create a setting of decreased circulation leading to local tissue ischemia, cellular apoptosis and the release of various agents (cytokines, intracellular potassium, end products of necrotic striated muscle, such as myoglobin)9. This toxic milieu leads to the formation of edema of adjacent cells, increased extracellular fluid within the compartment due to several mechanisms (such as venous /lymphatic obstruction / insufficiency which synergistically causes an increase in the pressure of the compartment. This results in insufficient blood supply to muscles and nerves. Acute compartment syndrome is a medical emergency that requires surgery to correct. If untreated, the lack of blood supply leads to permanent muscle and nerve damage and can result in the loss of function of the limb
COMMON SIGNS AND SYMPTOMS OF ACUTE COMPARTMENT SYNDROME
The first and most common clinical signs of compartment syndrome are numbness, tingling and loss of two-point discrimination and paresthesia6,11,12. These are known as the five Ps (pain, pallor, pulselessness, paralysis and paraesthesia). This author would add poikiliothermia (a cool near room temperature extremity that is present in delayed presentations) as a sixth clinical sign.
Paresthesia in the distribution of the nerves traversing the affected compartment has also been described as relatively early sign of compartment syndrome, and later is followed by anesthesia Pain is usually ‘out of proportion’ to the injury requiring increasing doses of strong opiates. The pain is commonly a deep, burning type, which worsens with passive stretching of the muscles in the compartment. Pain out of proportion to the injury’ and ‘pain with passive stretching of the muscles in the compartment’ are the earliest, most reliable indicators of ACS
In severe trauma or when the patient is unconscious pain may, however, be difficult to assess. Pain is also subjective and has a poor sensitivityLoss of function and decreased pulses or no pulses on physical examination are late clinical manifestations.
•Pain is reported early in most cases. The patient will often describe a deep, persistent, diffuse pain out of proportion with the physical examination .The pain is aggravated by passive flexion and extension of the involved muscle group within the compartment and responds poorly to analgesic agents.
•Paresthesia of the affected limb is common.
•Paralysis of the limb is a late finding.
•The compartment may feel tense and firm on physical examination. On inspection the skin may appear swollen, shiny; bruising of the skin may also be present.
•Congestion of the digits with prolonged capillary refill (greater than 2 seconds) time is common.
•A loss of pulses occurs late if the artery being examined is contained within the affected compartment.
DIAGNOSIS OF ACUTE COMPARTMENT SYNDROME
ACS is a clinical diagnosis; early recognition and emergent surgical intervention are associated with the best clinical outcomes13,19.Once the clinical diagnosis has been made, the treatment is emergent surgical fasciotomy.
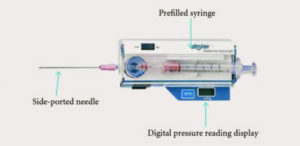
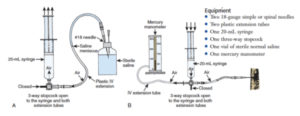
When in doubt (e.g. poor clinical exam, obtunded / non- communicative patient), a measurement of the intra-compartmental pressures can be done at the patient bedside or in the operating room. Utilizing aseptic technique a puncture site is selected from an area within 5-6 cm from the site of injury into the relevant compartment. Commercial devices such as the Stryker monitor may be used (e.g. Stryker monitor20, Fig.1) or a transducer can be fashioned from standard hospital equipment such as the Mercury Manometer System (Whitesides method, inaccurate /overestimates compartment pressure (Figure 2)21, or Arterial Line System (in vitro excellent correlation between actual pressure / measured pressure (Figure 3) which can be assembled from suppliestypically found in the Emergency Room
All compartments in the affected limb should be measured 24.Inconclusive readings should be rechecked along with a serial physical exam.
The normal intra-compartmental pressure is 10 mmHg25. Hargens et al. in his study in the dog model described the absolute intra-compartmental pressure values of 30 mmHg, 45 mmHg and 50 mmHg “as the critical threshold above which circulation is compromised”. Based on multiple animal models, 30 mmHg has been shown to be the earliest threshold in which blood flow is impeded and the fascia of the involved muscle group is maximally stretched
INDICATIONS FOR FASCIOTOMY
Fasciotomy wounds contribute to increase in-patient length of stay and can present a difficult reconstructive challenge. Once the compartment pressure has been relieved, the wound should be closed as quickly and early as possible to avoid further complications. Skin grafting carries its’ own inherent morbidity with cosmetic considerations at both the donor and fasciotomy site and increased metabolic healing burden to the patient. Primary closure results in a more functional and esthetic outcome with less morbidity for the patient, but can often be difficult to achieve secondary to edema, skin retraction, and skin edge necrosis
Wall27 further defined the indications for fasciotomy:
1. Clinical signs of acute compartment syndrome
2. Absolute compartment pressure > 30 mm Hg
3. Perfusion pressure < 30 mm Hg
 Figure 5. Fig 4,5 show ischemic upper extremity compartment syndrome due to venous and arterial outflow compression.outflow compression.
Figure 5. Fig 4,5 show ischemic upper extremity compartment syndrome due to venous and arterial outflow compression.outflow compression.
In a recent retrospective study by Zannis J1, Angobaldo J et al. the authors summarized their experience. Their series included 458 patients who underwent 804 fasciotomies. Of these, 438 received exclusively standard V.A.C.® Dressings, 270 received only normal saline wet-to-dry dressings, and 96 were treated with a combination of both. Of the sample, 408 patients were treated with exclusively V.A.C.® Therapy or wet-to-dry dressings and 50 patients were treated with a combination of both. In comparing all wounds, there was a statistically significant higher rate of primary closure using the V.A.C.® Therapy versus traditional wet-to-dry dressings (P < 0.05 for lower extremities and P < 0.03 for upper extremities). The authors found that the time to primary closure of wounds was shorter in the V.A.C.® Therapy group in comparison with the non-V.A.C.® Therapy group.
This study shows that the use of the VAC for fasciotomy wound closure results in a higher rate of primary closure versus traditional wet-to-dry dressings. The authors also noted that the time to primary closure of wounds and the time to skin grafting were shorter when V.A.C.® Therapy was employed.
 Figure 7. 17 y.o. Female Heroin addict was found unconscious with her left leg dangling over a chair. No other co- morbidities. The patient underwent fasciotomy, after popliteal artery thrombectomy.
Figure 7. 17 y.o. Female Heroin addict was found unconscious with her left leg dangling over a chair. No other co- morbidities. The patient underwent fasciotomy, after popliteal artery thrombectomy.
The use of V.A.C.® Therapy in this series was found to decrease length of hospital stay, allowed for earlier rehabilitation, and ultimately lead to increased patient satisfactionIn a study by Yang et al. the authors reviewed the records of a consecutive series of 34 patients who had compartment syndrome of the leg requiring the standard two-incision release of all four compartments and received the application of VAC therapy until the time of definitive wound closure or coverage. A matched series of 34 consecutive antecedent patients with the same entry criteria, except for the use of the VAC, were also studied and served as a control group. The main parameter measured was the time to “definitive closure” (delayed primary closure with sutures or skin graft coverage) of the wounds. Of the 68 wounds in 34 patients managed with V.A.C.® Therapy, the average time to definitive closure for both the lateral and the medial wounds was 6.7 days. For the 70 wounds in the 34 control patients, the average time to definitive closure was 16.1 days. This difference in time to wound closure between the V.A.C.® Therapy group and the non-V.A.C.® Therapy group was statistically significant (p < .05). The authors concluded “sub atmospheric treatment for compartment syndrome of the leg after fasciotomy theoretically increases resolution of tissue edema that are components of this clinical entity. Experimental work has shown vacuum-assisted wound management to be effective in hastening the resolution of wound edema, enhancing local blood flow, promoting granulation tissue, and thwarting bacterial colonization. These factors may account for its utility in the management of fasciotomy wounds in the setting of compartment syndrome of the leg
CONCLUSION
There are currently numerous techniques described in the literature that attempt to optimize wound closure following fasciotomy including simple elevation through strict adherence as described by Bengezi and Vo.30Each has its advantages and optimal clinical indications. Although ideal, primary and or definitive closure of fasciotomy wounds continues to be a challenge due to multiple factors (e.g. difficult anatomical topography, edema). The literature shows that with the use of VAC therapy primary / definitive closure can more frequently be achieved. This brief review of the literature suggests that the application of negative pressure therapy is versatile, efficient, and cost effective and could be an important part of a surgeon’s armamentarium.
References
1.Volkmann R. Die ischämischen Muskellähmungen und Kontracturen. Centralblatt für Chirurgie. Leipzig. 1881; 8:801–83.
2.Abraham T Rasul, Jr, MD; Chief Editor: Consuelo T Lorenzo, MD. Acute Compartment Syndrome Emedicine: http://emedicine.medscape.com/article/307668-overview#a3
3.Critical closing pressure in human peripheral vascular beds. ASHTON H Clin Sci. 1962 Feb; 22(): 79-87.
4.Ashton H. The effect of increased tissue pressure on blood flow. Clin Orthop Relat Res. 1975;(113): 15–26. [PubMed]
5.Matsen FA, 3rd, Krugmire RB JR. Compartmental syndromes. Surg Gynecol Obstet. 1978; 147:943–9. [PubMed]
6.Matsen FA 3rd. Compartmental syndrome. An unified concept. Clin Orthop Relat Res. 1975 Nov-Dec. 8-14. [Medline].
7.Hartsock LA, O’Farrell D, Seaber AV, Urbaniak JR. Effect of increased compartment pressure on the microcirculation of skeletal muscle. Microsurgery. 1998; 18:67–71. [PubMed]
8.“Compartment Syndrome: Fractures, Dislocations, and Sprains: Merck Manual Professional
9.Lawendy, Abdel-Rahman, “Pathophysiology of Compartment Syndrome” (2014). Electronic Thesis and Dissertation Repository. Paper 2053. http://ir.lib.uwo.ca/etd/2053
10.Muscles Ligaments Tendons J. 2015 Jan-Mar; 5(1): 18–22. Published online 2015 Mar 27. PMCID: PMC4396671
11.Elliott KG, Johnstone AJ. Diagnosing acute compartment syndrome. J Bone Joint Surg. – British Volume 2003; 85: 625–32.
12.Köstler W, Strohm PC, Südkamp NP. Acute compartment syndrome of the limb. Injury 2004; 35:1221.
13.Olson SA, Glasgow RR. Acute compartment syndrome in lower extremity musculoskeletal trauma. J Am Acad Orthop Surg. 2005; 13(7): 436–44. [PubMed]
14.Ulmer T. The clinical diagnosis of compartment syndrome of the lower leg: are clinical findings predictive of the disorder. J Orthop Trauma. 2002; 16:572–7. [PubMed]
15.Whitesides TE, Heckman MM. Acute compartment syndrome: update on diagnosis and treatment. J Am Acad Orthop Surg. 1996; 4(4): 209–18. [PubMed]
16.Ulmer T. The clinical diagnosis of compartment syndrome of the lower leg: are clinical findings predictive of the disorder. J Orthop Trauma. 2002; 16:572–7. [PubMed]
17.Beraldo S, Dodds SR. Lower limb acute compartment syndrome after colorectal surgery in prolonged lithotomy position. Dis Colon Rectum 2006; 49:1772.
18.Figueras Coll G, Albortí Fitó G, Iborra Gonzàlez M, et al. Bilateral compartment syndrome in thighs and legs by methanol intoxication: a case report. Emerg Med J 2008; 25:540.
19.Mabee JR, Bostwick TL. Pathophysiology and mechanisms of compartment syndrome. Orthop Rev. 1993; 22(2): 175–81. [PubMed]
20.Stryker Corporation. Kalamazoo MI. United States of America
21.Ullasz A et al. Comparing the methods of measuring compartment pressures in acute compartment syndrome. Am J Emerg Med 2003; 21: 143-5. PMID: 12671817
22.Boody AR, Wongworawat MD. Accuracy in the measurement of compartment pressures: a comparison of three commonly used devices. J Bone Joint Surg 2005; 87: 2415-2422. PMID: 16264116
23.Rockwood CA JR, Green DP, Bucholz RW, Heckman JD, editors. 4th ed. Lippincott-Raven: Philadelphia PA: 1996. Rockwood and Green’s Fractures in Adults.
24.Matsen FA 3rd, Clawson DK. The deep posterior compartmental syndrome of the leg. J Bone Joint Surg Am. 1975; 57-A: 34–9. [PubMed]
25.Giannoudis PV, Tzioupis C, Pape HC. Early diagnosis of tibial compartment syndrome: continuous pressure measurement or not. Injury. 2009; 40:341–2. [PubMed]
26.Hargens AR, Akeson WH, Mubarak SJ, et al. Fluid balance within the canine anterolateral compartment and its relationship to compartment syndromes. J Bone Joint Surg Am. 1978; 60-A: 499–505. [PubMed]
27.Wall CJ et al. Clinical practice guidelines for the management of acute limb compartment syndrome following trauma. ANZ J Surg 2010; 80: 151-6. PMID: 20575916
28.Zannis J1, Angobaldo J, Marks M, DeFranzo A, David L, Molnar J, Argenta L. Comparison of fasciotomy wound closures using traditional dressing changes and the vacuum-assisted closure device. Ann Plast Surg. 2009 Apr; 62(4): 407-9. doi: 10.1097/SAP.0b013e3181881b29.
29.Yang CC1, Chang DS, Webb LX. Vacuum-assisted closure for fasciotomy wounds following compartment syndrome of the leg. J Surg Orthop Adv. 2006 Spring; 15(1): 19-23.
30.Omar Bengezi, MBBS MD FRCSC1 and Anthony Vo. Elevation as a treatment for fasciotomy wound closure. Can J Plast Surg. 2013 Autumn; 21(3): 192–194.