Kirketerp-Møller_Current Dialogues in Wound Management_2015_Volume 1_Issue 2
DIABETIC foot ulcers (DFUs) are considered to be one of the major complications of diabetes. They occur in 15% of all diabetic patients and are the cause of 84% of major amputations in diabetic patients. The definition of a DFU is not as straightforward as it may seem, but the Danish National Health Board has defined it as “a lesion in the skin of the foot in a diabetic patient.” This is a very broad definition but the purpose of this is to emphasize that no lesion is insignificant if it is not healing; any DFU should be referred to a specialized unit if not healed within 3 weeks.
This is a very important statement. This indicates that nonhealing DFUs need specialized treatment. Additionally, the patients should be referred for specialized treatment in case of infection or insufficient blood supply.
The aim of the present paper is to emphasize that, if basic principles are used at all times in the treatment of DFU and when adhering to a very simple model, in fact most DFUs will heal.
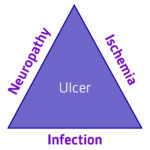
The diabetic foot triangle identifies the three main contributing factors to nonhealing of the DFU. There has been a delusion that diabetic patients have very low healing potential. This is not true. It is the complications of diabetes that affect wound healing and not diabetes itself. By identifying each contributing factor and eliminating the effects, healing will occur. The diabetic foot triangle will help in identifying the contributing factors. The task is then to eliminate them, and the wound will heal in most cases.
NEUROPATHY
Neuropathy is the main cause of the DFU. There are several ways to diagnose neuropathy. Vibration threshold, 10-g monofilament, heat and cold discrimination, and sweat secretion are some of the methods most commonly used. Combined methods and scoring systems like The Neuropathy Symptom Score are valuable in research and longitudinal studies, but in treating the ulcer, presence of neuropathy is presumed. If a foot ulcer can be acquired by walking, or a stone in the shoe is not recognized, then neuropathy is present. Treatment of neuropathy is restricted to symptomatic treatment of pain. No medical treatment will improve sensation. It is also important to accept that patients can have neuropathy despite normal vibration threshold and monofilament examination. The treatment option for the neuropathy side of the triangle is offloading. The challenge is that loss of sensation is not perceived and perception is a prerequisite for recognition. Hence, offloading may be prescribed but not followed.
ISCHEMIA
Ischemia is the main reason for major amputation in diabetic patients and the most important factor for the outcome of the DFU. The evaluation of the blood supply can, to some extent, be done by clinical signs: skin temperature and color and palpation of pedal pulses. Evaluation in case of signs of decreased blood supply includes distal blood pressures, like ankle and toe pressures, and/or transcutaneous oxygen pressure (TcPO2). However, sometimes the clinical signs and TcPO2 are difficult to interpret. It is important that symptoms of ischemia, such as pain and claudication, may be absent in diabetic patients due to neuropathy. Distal ankle pressure is frequently falsely elevated due to calcifications of the greater vessels, and sometimes this also complies to toe pressure. The skin temperature and color do not always reflect the real perfusion. Due to neuropathy, the skin can be relatively warm because of dilated skin vessels, and redness of the skin in ischemia can be misinterpreted to infection.
In my clinical practice we use the toe pressure and every patient with a toe pressure below 30 mm Hg should be evaluated for vascular intervention. In addition, DFU patients with higher toe pressures are referred if they do not heal or worsen despite adequate treatment as described here.
INFECTION
Infection in the DFU is very difficult to diagnose. A positive culture from a swab or biopsy will give little evidence of infection, as every chronic wound will be contaminated with bacteria. A positive culture with Staphylococcus aureus does not necessarily lead to antibiotic treatment. The classical signs of infection, skin erythema, pain, fever, swelling, and impaired function (rubor, dolor, calor, tumor, and functio laesa) will often be absent due to neuropathy.
However, when these signs are present, the infection is often very severe and requires that the patient is admitted and evaluated for surgery. When should you consider infection with absent signs of infection? If a probe can reach bone, joint capsule or tendons, antibiotic treatment is needed despite absence of signs of infection. If a DFU has been present for more than 3 months, a chronic infection and especially chronic osteomyelitis should be considered and treated.
HOW TO USE THE DIABETICFOOT ULCER TRIANGLE
The diabetic foot triangle should be used in every encounter with the DFU patient. At the first contact it helps to identify possible obstacles to healing and to plan the workup and the treatment. At the following visits, the triangle if healing is not progressing as expected. It is my experience that in 80% of all secondary visits I discover that the patients do not adhere to the offloading regimen. They do not use the prescription shoes at all times, they walk barefoot inside their house, or use ordinary footwear for special occasions. Walking to the bathroom two or three times per night barefoot is not unusual. The neuropathy makes these small “field-trips” insignificant for the patient, and unless we address the importance of these unprotected footsteps, they will not alter behavior. I often tell my patients that these few steps without protective footwear easily can disrupt whatever healing occurred during the whole day.
TAKE-HOME MESSAGE
By using this simple triangle you can work yourself around what is important in treating DFUs: Identify obstacles in the healing process!
Remember that the diabetic foot ulcer heals, not because of the things we put in, but what we take off. –David Armstrong
This is what you can remove:
1.Load
2.Ischemia
3.Infection