Dr. Orgill is Vice Chairman for Quality Improvement in the Department of Surgery at Brigham and Women’s Hospital and Professor of Surgery at Harvard Medical School. He is a reconstructive plastic surgeon and has a PhD from MIT in Medical Engineering. He is the Director of the Brigham and Women’s Hospital Wound Care Center and runs a tissue engineering and wound healing Laboratory. His lab at BWH is working to develop better technologies to treat wounds including work with artificial skin, micromechanical forces, platelets and stem cells. He has consulted for several medical device and start-up companies and is the inventor on several patents. He worked on the team that developed Integra®, a skin replacement therapy that has been commercially developed and used successfully on thousands of patients.
Orgill_Current Dialogues in Wound Management_2016_Volume 2_Issue 3
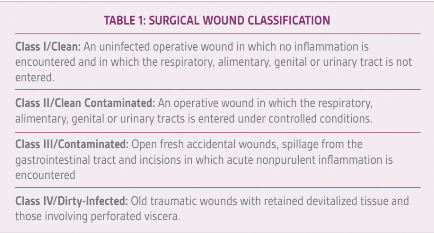
Wound infections are the second most common type of nosocomial infection in hospitals and add tremendous costs to our healthcare system. Wound infections are more common in wounds that are contaminated with bacteria, but can sometimes occur in clean cases where there is little anticipation that a wound infection could occur. The classification of wound type and the relation to infection risk have been well publicized by the Centers for Disease Control (Table 1).
We will focus our attention on best practices that can prevent the occurrence of wound infections in clean cases (Figure 1). Skin covers an area of nearly two square meters in adults, and a very thin layer of dead keratinocytes form the stratum corneum that prevents transit of bacteria from the environment into the wound. Cultures of skin surface show that a number of bacteria normally reside and generally do not cause problems for humans. Gastrointestinal tract locations such as the mouth and colon have very high levels of bacteria present, and there are natural mucosal barriers that prevent bacterial invasion.
ENVIRONMENT
According to our current theory, wound infections occur because bacteria are able to proliferate within the host faster than the host is able to kill them. The inflammatory response to the bacteria results in the recruitment of white blood cells, and pus is formed. When these inflammatory mediators go into the bloodstream they can induce a fever and eventually sepsis. Preparation for surgery today has a host of environmental factors regulated to prevent bacteria from entering the surgical field. This includes sterilization of instruments, skin preparation, laminar air flow within the operating rooms and cleaning surfaces between patients. Having the patient bathe with anti-bacterial soap the day before the surgery can help reduce the number of bacteria present on the skin surface. Hand washing has been shown to be a very effective method to prevent the transmission of bacteria from patient to patient, while placing various protective clothing may help spread the transmission of resistant bacteria. We also know that keeping patients warm and well oxygenated can reduce infections. Under general anesthesia it is easy for the core temperature to decrease. Efforts to keep the temperature normal, including keeping the room warm, warming fluids and using warming devices, can help reduce infection rates.
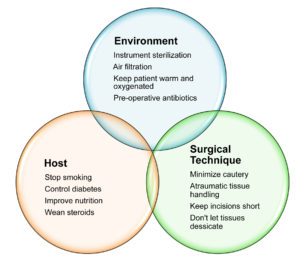 Figure 1: Simple measures to reduce infections in clean elective surgery cases.
Figure 1: Simple measures to reduce infections in clean elective surgery cases.
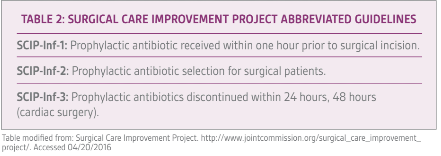
Pre-operative antibiotics have been shown to lower wound infections in many types of surgery. Evidence suggests that having a high serum level of antibiotics at the time of incision will reduce infection risks. Guidelines for the administration, timing and selection of antibiotics have been promoted by the Surgical Care Improvement Project (SCIP) and have been adopted by most healthcare institutions in the US (Table 2). Surgeons implant a number of medical devices into most patients on whom we perform surgery. These can range from simple sutures to hemostatic clips to large implants. If contaminated, these devices can develop infections that are difficult to treat, in many cases requiring removal of the foreign body. Particularly, materials with complex surfaces, such as braided permanent sutures, allow areas for bacteria to proliferate where they are not exposed to adequate levels of antibiotics. Bacteria can often form biofilms on these surfaces, which also become difficult to treat.
HOST
The human body has developed an elaborate immune system to fight off bacteria. Antibiotics have been available for around one hundred years. Prior to that, infections were generally treated by surgery (incision and drainage). Blood flow is critical to prevention of infection. Tissues that have high capillary
blood flow, such as the skin in the head and neck, rarely become infected. Even in heavily contaminated areas such as the mouth or anus, the high rates of blood flow through tissues make infections in these areas relatively unusual. Yet, in people with inflammatory bowel disease, the response to injury is impaired and localized areas of infection and fistulas can develop.
Patients that are neutropenic also are at high risk for infection. Similarly, in patients on immunosuppressive drugs, such as chemotherapy for cancer and medications to stop rejection after organ transplantation, make patients even more susceptible to infection. Pediatric patients and young adults appear to be able to fight off bacteria and heal faster than elderly patients. The nutritional status of patients is also critical. A number of other factors, such as diabetic control, smoking status and steroid use, also relate to the probability of wound infections. The risk of sternal wound infections has been reduced significantly by peri-operative control of glucose levels, often with insulin drips.
Patients are naturally colonized with bacteria, and certain patients have pathogenic bacteria present. For example, some patients harbor Methacillin resistant Staphylococcus aureus (MRSA) in their skin or nares. For certain procedures, such as total joint replacement and median sternotomy, altering the peri-operative antibiotics to treat these resistant bacteria can be helpful.
SURGICAL TECHNIQUE
Surgical technique clearly is an important contributor to wound infection. We know that using techniques that minimize trauma or desiccation of tissue are critical. Dead tissue provides a nidus for infection and bacterial proliferation by being a source of nutrients without any anti-infective abilities. Energy devices such as electrocautery are very helpful in controlling bleeding, but create areas of necrotic tissue that can be at risk for developing an infection. Surgeons that can perform operations through short incisions and shorter time periods will also reduce infection risks.
Pre-operative prophylactic antibiotics that are properly selected and given within one hour prior to the surgical incision have been shown to reduce infection rates in major surgical cases. Continuing antibiotics past 24, or in some cases, 48 hours has not been shown to improve infection rates and have a risk of selecting out resistant bacteria. These measures have been reported in many US centers through Surgical Care Improvement Project (SCIP) and Outpatient Quality Reporting.
CONCLUSION
Wound infections can be attributed to various causes and can be particularly bothersome in clean cases where they are rare. Being aware of environmental, host and surgical technique factors that contribute to infections can be useful in their prevention.
References
http://www.medscape.org/viewarticle/531895_2, http://www.aqaf.com/perch/resources/library/2014-oqr-quick-reference-booklet-for-clinicians-pub.pdf