
Dr. Orgill is Vice Chairman for Quality Improvement in the Department of Surgery at Brigham and Women’s Hospital and Professor of Surgery at Harvard Medical School. He is a reconstructive plastic surgeon and has a PhD from MIT in Medical Engineering. He is the Director of the Brigham and Women’s Hospital Wound Care Center and runs a tissue engineering and wound healing Laboratory. His lab at BWH is working to develop better technologies to treat wounds including work with artificial skin, micromechanical forces, platelets and stem cells. He has consulted for several medical device and start-up companies and is the inventor on several patents. He worked on the team that developed Integra®, a skin replacement therapy that has been commercially developed and used successfully on thousands of patients.
Orgill_Current Dialogues in Wound Management_2015_Volume 1_Issue 2
HIDRADENITIS SUPPURATIVA (HS) is a chronic disease of the skin thought to be related to inflammation of the apocrine glands. It is commonly seen in the axilla, underneath the breasts, in the perineum, and on the upper thighs. It is a frustrating disease for both patients and clinicians to manage; in part, because we do not totally understand the pathophysiology of the disease. In fact, there is a 20-fold range of the reported incidence of the disease ranging from 0.2 to 4.1% of the population.
Mild cases can be treated with antibiotics or acne drugs, moderate cases by incision and drainage. More severe cases are now being treated with anti-inflammatory drug infusions or surgery. Many patients, by the time they reach a surgeon, have tried many therapies for this disease. They are frustrated and worried about their disease. Each day having to deal with the unpleasant odor of draining wounds in generally covered areas of the body can be truly emotionally draining.
Surgical treatment of HS has been difficult for patients, nursing staff, and surgeons. Many surgeons have attempted to operate on these patients, had complications or unhappy patients,and given up. A traditional way of treating this is wide excision of the area followed by dressing changes and allowing the area to heal by secondary intent. Although effective, this method takes a long time for wounds to heal and can be quite painful. As a result, surgeons have proposed a number of therapies including direct skin closure, skin grafts and flaps for large lesions. In our experience, excision and direct closure at the same operation can be quite effective with small lesions (<70 cm2). Doing this with large lesions often resulted in infection or wound dehiscence.
With the advent of Negative Pressure Wound Therapy (NPWT) systems, we learned that they could remove excess fluid and also promote a rich vascular supply at the surface of the wounds. For large areas of HS, we began to excise the lesions, treat them with a NPWT device and then subsequently close the wound. In March of 2014 we reported our case series of 60 cases over 7 years showing our protocol in Figures 1 and 2.
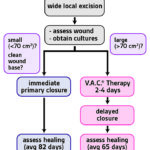 Figure 1. Treatment methods. All patients with hidradenitis suppurativa underwent wide local excision and had intraoperative wounds cultured for sensitivity-based antibiotic therapy. Small wounds underwent immediate primary closure. Healing times averaged 82 days for patients with immediate primary closure and 65 days for those with delayed primary closure
Figure 1. Treatment methods. All patients with hidradenitis suppurativa underwent wide local excision and had intraoperative wounds cultured for sensitivity-based antibiotic therapy. Small wounds underwent immediate primary closure. Healing times averaged 82 days for patients with immediate primary closure and 65 days for those with delayed primary closure Figure 2. Vacuum-assisted closure is thought to act in multiple ways, by increasing blood flow and granulation tissue formation, decreasing wound size, and assisting wound drainage.
Figure 2. Vacuum-assisted closure is thought to act in multiple ways, by increasing blood flow and granulation tissue formation, decreasing wound size, and assisting wound drainage.
For large excisions (>70 cm2), our patients have their first operation on the day of admission and then stay in the hospital 2 to 4 days for closure. We then return them to the operating room for a short surgery, where the sponge interface material is removed from the wound and the wound is closed. We use a drain for wounds with a substantial dead space. Overall, they have been happy with this technique once they are healed. They appreciate the fact that they do not have to have large dressing changes. It generally provides stable wound coverage with an acceptable aesthetic result. There still is a fair incidence of minor wound complications, (9/30 cases) based on my experience, which could be managed with conservative dressing changes. In all cases where we had wound complications, the dressing changes were substantially smaller than if we had left the wounds totally open.
For patients with severe HS, we recommend a team approach led by a dermatologist and a surgeon who are interested in this disease. We let our patients know that HS takes a long time to get better and that having a multidisciplinary approach can often be the best method. Being in the care of individuals that they trust, even when complications occur, is very helpful. Many surgeons and dermatologists are not well trained in this disease. There have been many recent advances and health care providers that take on these patients, and they should be well prepared to manage complications.
Despite the difficulties managing this disease, these can often be some of the most grateful patients that we treat. New technologies such as NPWT devices along with other medical management techniques2improved therapeutic options for HS. When successful, we can either cure or dramatically improve this disease and make a major change in their lifestyle and outlook on life.
References
1. Chen YE, Gerstle T, Verma K, Treiser MD, Kimball AB, Orgill DP. Management of hidradenitis suppurativa wounds with an internal vacuum-assisted closure device. Plast Reconstr Surg. 2014;133(3):370e-377e.
2.Scheinfeld N. Hidradenitis suppurativa: A practical review of possible medical treatments based on over 350 hidradenitis patients. Dermatol Online J. 2013;19(4):1.

