Dr. Robert Klein completed podiatric medical school in Chicago at the Rosalind Franklin University of Medicine and Science, Scholl College of Podiatric Medicine. Dr. Klein continued his surgical training as the Chief Resident at Michigan Health Center in Detroit. Dr. Klein is a Clinical Assistant Professor in the Department of Surgery at the University of South Carolina School of Medicine (USCSOM) Greenville and specializes in wound care, limb preservation, and surgery.
Klein_Current Dialogues in Wound Management_2020_Article_8
Introduction
Diabetic foot ulcerations (DFUs) can be very challenging to heal. DFUs in many instances have longer healing times, require aggressive offloading to decrease shear and pressure to plantar foot wounds, and are at increased risk for infection and/or amputation.1
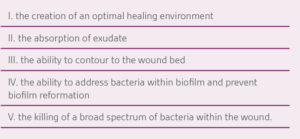
Wound bed preparation is essential to wound healing. Debridement and offloading are critical components to wound bed preparation — as is the selection of an advanced wound care dressing (AWD). In our center, AWD product selection is determined by the patient’s needs and dressing features such as:
Silver oxysalts (Ag OXYSALTS™ Technology, Argent Limited Partnership, Knutsford, UK ) have been shown to be effective in promoting wound healing, while at the same time combating infection and bioburden within a wound.2
Case Study
A 64-year-old male with a past medical history of Type II diabetes mellitus, chronic kidney disease, and diabetic peripheral neuropathy presented to the emergency department (ED) with concerns for a left foot wound and left foot/leg infection. The patient was walking barefoot across a hot concrete dock and stated that he sustained a superficial burn to the bottom of his left foot. Later that evening, he noticed that the skin on the burn area was peeling off. The patient reported worsening of the redness of his left foot and left lower extremity. He became febrile and fatigued. The patient was admitted to the hospital with a diagnosis of cellulitis and an infected diabetic foot wound. He received one dose of intravenous (IV) vancomycin while in the ED, followed by IV cefazolin during his hospital admission. The patient’s treatment, while in the hospital, consisted of the application of a hydrogel to his left foot wound, along with a sterile secondary dressing which was changed daily. Bacterial culture and sensitivity results of the left foot wound was positive for Staphylococcus aureus and the patient was discharged from the hospital after receiving three days of IV antibiotics, along with local wound care. The patient’s discharge medications included 10 days of amoxicillin/clavulanic acid, and hydrogel for his left foot wound. The patient was referred to our wound care center (WCC) for out-patient treatment of his left foot wound.
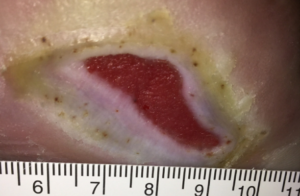
The patient was seen in our WCC three days after discharge from the hospital. A large plantar forefoot wound was noted and x-rays were negative for any bony destruction, periosteal reaction, and/or lysis; however, bounding foot pulses were observed. The patient’s feet were insensate, with complete loss of protective sensation. Devitalized tissue, slough, exudate, and biofilm were noted in the patient’s left foot wound (Figure 1).

Treatment options were discussed with the patient, and a plan of care was formulated. After a sterile prep, sharp debridement of the patient’s left foot wound was performed with a dermal curette (Figure 2) – no anesthesia was needed. KERRACEL™ Ag Gelling Fiber Dressing (Systagenix Wound Management Ltd., Knutsford, UK) was selected for use due to the dressing’s ability to create an optimal healing environment, ability to contour to the wound bed, and its antimicrobial properties. Dressing changes occurred every three days, and the patient was prescribed a controlled ankle movement (CAM) walker for off-loading of the left foot. The patient returned to the clinic weekly for re-check and debridement of the wound. The KERRACEL™ Ag Dressing was used for a total of 21 days.

The patient’s wound responded extremely well to debridement, the KERRACEL™ Ag Dressing, and offloading. We estimated that a 35% reduction was seen in the patient’s wound size after 21 days of treatment. At the follow-up visit, we noted a robust, healthy, red granulation tissue in the wound bed, as well as a significant decrease in slough, exudate, and biofilm (Figure 3).

On day 35, the patient was counseled on advanced wound care modalities, including total contact casting, and/or the use of a cellular tissue product to aid in closure. The patient was very pleased with his progress and declined the aforementioned wound care modalities.
The use of PROMOGRAN PRISMA™ Matrix (Systagenix Wound Management Ltd., Gargrave, UK) has been demonstrated to be effective in closing DFUs.3;4 Our center has extensive experience using PROMOGRAN PRISMA™ Matrix in complex wounds – including its use for DFUs, traumatic wounds, and plantar surface burns.5 As a result of our experience and our approach to clinical management, the patient’s wound care regimen was changed to PROMOGRAN PRISMA™ Matrix with instructions to change the AWD every other day, cover with gauze, and to continue offloading in the CAM walker. The patient was followed weekly at the WCC with serial x-rays of the patient’s left foot remaining unchanged and with no radiographic findings for osteomyelitis. The patient’s inflammatory markers, erythrocyte sedimentation rate and C-reactive protein, were noted as being in the normal reference range during the course of his treatment.
At Day 56, the patient’s wound had decreased in size by 72% from initial presentation to the WCC (Figure 4). The patient was very pleased with his progress – no changes were made to his care plan. The patient was last seen at Day 84 with a 90% decrease in wound size (Figure 5) and, in our clinical judgement, it is anticipated that the patient will be completely closed within the next three to four weeks.

Discussion
We presented a case study of an extensive diabetic foot wound secondary to a thermal burn that was successfully treated with sequential wound therapy of KERRACEL™ Ag Dressings and PROMOGRAN PRISMA™ Matrix to near full closure. The patient is still under care with the anticipation of full closure. However, due to the COVID-19 pandemic, in-person clinic visits have been switched to follow-up though telemedicine.
Patient data and photos courtesy of Dr. Robert Klein.
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
NOTE: Specific indications, contraindications, warnings, precautions, and safety information exist for these products and therapies. Please consult a clinician and product instructions for use prior to application. Rx only.
References
- Frykberg RG, Zgonis T, Armstrong DG et al. Diabetic foot disorders. A clinical practice guideline (2006 revision). J Foot Ankle Surg 2006;45(5 Suppl):S1-S66.
- Thomason HA, Lovett JM, Spina CJ, Stephenson C, McBain AJ, Hardman MJ. Silver oxysalts promote cutaneous wound healing independent of infection. Wound Repair Regen 2018;26(2):144-152. doi:10.1111/wrr.12627.
- Gottrup F, Cullen BM, Karlsmark T, Bischoff-Mikkelsen M, Nisbet L, Gibson MC. Randomized controlled trial on collagen/oxidized regenerated cellulose/silver treatment. Wound Repair Regen 2013;21(2):216-225. doi:10.1111/wrr.12020.
- Griffin L, Carter MJ, D’Agostino R, Jr., D’Agostino McGowan L. Comparative Effectiveness of Two Collagen-containing Dressings: Oxidized Regenerated Cellulose (ORC)/Collagen/Silver-ORC Dressing Versus Ovine Collagen Extracellular Matrix. Wounds 2019;31(11):E73-E76.
- Klein RJ. Use of Oxidized Regenerated Cellulose (ORC)/Collagen/Silver-ORC Dressings Alone or Subsequent to Advanced Wound Therapies in Complex Wounds. Wounds 2020;32(2):37-43.
©Copyright 2020 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. PRA-PM-US-02432 (05/20).