
Dr. Laura Swoboda is a translational scientist, family nurse practitioner, and practicing wound specialist in Milwaukee, Wisconsin. In addition to providing direct patient care, Dr Swoboda serves as principal investigator for quality improvement, evidence-based practice, and research projects in complex wound care. They serve on the board of directors for the WOCNCB and the AAWC, on the NPIAP’s prophylactic dressing standards initiative task force, and the American Heart Association’s Peripheral Arterial Disease National Action Plan. Laura Swoboda is a paid consultant of Solventum.
Swoboda_Current-Dialogues-in-Wound-Management_2024_Article-2
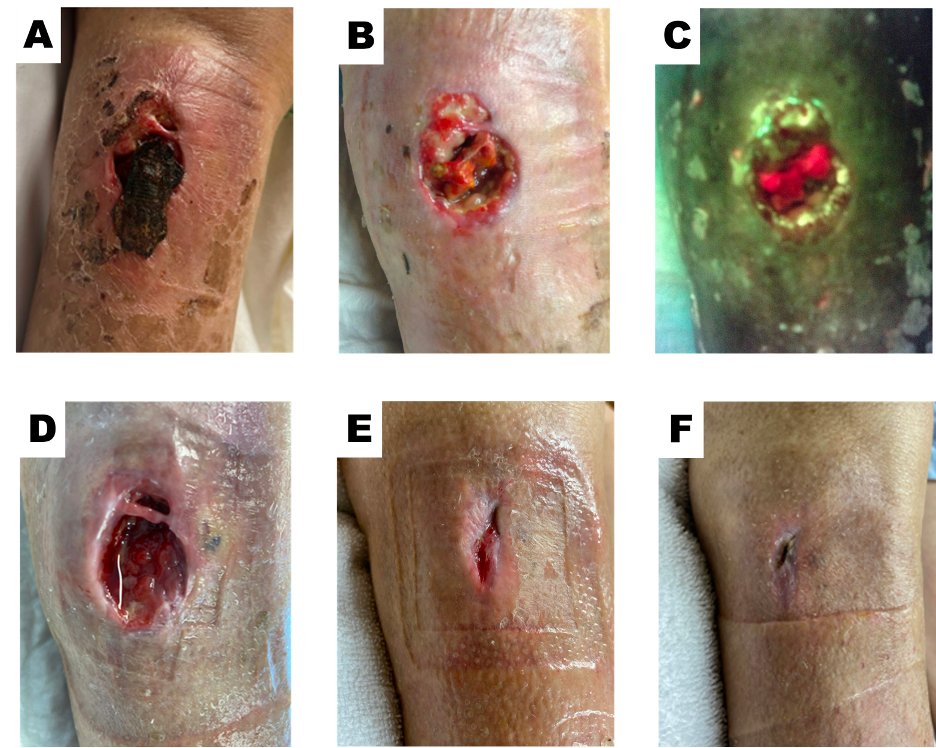
CASE REPORT: An 88-year-old female with a medical history that includes atrial fibrillation, chronic anticoagulation treated with rivaroxaban, rosacea keratitis, rheumatoid arthritis, immunocompromised status, long-term methotrexate use, hypertension, and hepatocellular carcinoma with bone involvement, sustained a traumatic ulcer on her right leg after a fall at home, resulting in a hematoma. The ulcer persisted for 8 weeks before the patient sought care at the wound center in the hospital’s outpatient department in Southeastern Wisconsin. Prior to presenting, the patient had been under the care of her primary care provider who had been treating the ulcer with silver sulfadiazine cream and zinc oxide-coated adhesive compression bandages. Upon her presentation to the wound center, the wound dimensions were 3 cm x 2.2 cm x 1.5 cm, with 3.3 cm of undermining from the 6 o’clock to the 3 o’clock position (Figure 1A). The wound contained adherent wet and dry necrotic tissue and a hematoma, which obscured the wound bed, prevented wound edge migration, and fomented inflammation due to necrosis and bioburden. The wound treatment plan was adjusted to address and overcome common barriers to healing. The wound, peri-wound tissues, and the entire extremity below the knee joint were cleansed with mild soap and water. Hypochlorous acid was applied to the wound and periwound tissues, ensuring a consistently wet surface, and was allowed to soak for a minimum of 3 minutes per treatment. During visits with the wound specialist, the patient underwent sharp debridement to remove necrotic tissue and bioburden, address biofilm, refashion the wound edges to allow for centripetal epithelium migration, and expose the endothelium of blood vessels to reinitiate the healing cascade. Following the initial debridement (Figure 1B), which removed the loose necrotic material as tolerated, the patient was evaluated using fluorescence imaging. Fluorescence imaging uses violet light to assess the wound and periwound tissues for heavy bacterial loads. Under fluorescence, bacterial loads exceeding 104 colony-forming units (CFU) will fluoresce cyan or red, depending on the microbial species. Fluorescence imaging of the wound revealed red fluorescence within the wound cavity, within nonviable necrosing primarily adipose tissue, indicating a continued bioburden at 104 CFU (Figure 1C). The patient then started using a combination of 3M™ Promogran Prisma™ Matrix with ORC and Silver and 3M™ Coban™ 2 Two-Layer Compression System. During nursing assessments and follow-up appointments, the patient received non-contact low-frequency ultrasound treatments and mechanical debridement using gauze. At 2 weeks, undermining decreased while granulation increased (Figure 1D). At 8 weeks, the wound size decreased by 90% with no undermining (Figure 1E). Treatment with the Promogran Prisma Matrix was discontinued because the wound was flush, filled with granulation tissue, and nearly epithelialized. The patient was then switched to a foam dressing and Coban 2 Compression System, which was changed weekly. At 12 weeks, the wound was fully epithelialized (Figure 1F).
DISCUSSION: This case exemplifies the positive outcomes achieved by applying wound bed preparation and treatment best practices in the real-world challenges of wound management. Chronic disease management was optimized by adhering to these best practices. The patient’s wound healing was supported without requiring medication adjustments to methotrexate or anticoagulation therapies. To limit wound healing impairment, providers must be cognizant of complications and plan mitigation strategies. Delivering care according to a protocol can prevent many common causes of chronic wounds. This protocol often addresses wound healing inhibitors such as unhealthy granulation or swelling. Edema and inflammation, which are common and well-known wound healing inhibitors, can be addressed using a combination of Promogran Prisma Matrix and Coban 2 Compression System.
The extensive necrotic soft tissue and old hematoma contents contributed to the wound’s stagnation in the inflammatory stage, requiring thorough and repeated debridement. Chronic bacterial load, known to be associated with delayed wound healing, was demonstrated in this case through the fluorescence of necrotic tissue within the wound bed. This case also highlights how an inflamed wound can mask a heavy bioburden without exhibiting signs or symptoms of infection.
Promogran Prisma Matrix was chosen for its ability to promote a moist wound environment which is conducive to the development of granulation tissue, re-epithelialization, and optimal wound healing.1,2 The ionically bound silver component within the dressing, has been shown to provide an effective antimicrobial barrier in vitro. Edema, which can decrease lower extremity circulation and contribute to inflammation in wound tissues, also increases the risk of infection. Coban 2 Compression System provides consistent, dependable therapeutic compression below the knee, aiding the calf muscle in pumping lymphatic peri-wound edema into the next interstitial watershed.3 In this case of a complex lower extremity wound, the combined use of Promogran Prisma Matrix and Coban 2 Compression System was both effective and safe.
SUMMARY: This case highlights the successful use of the Promogran Prisma Matrix and Coban 2 Compression System in concert to achieve durable wound healing. These versatile tools enable healthcare providers to address complex wound management, ultimately benefiting patients.
References
- Gottrup F, Cullen BM, Karlsmark T, Bischoff-Mikkelsen M, Nisbet L, Gibson MC. Randomized controlled trial on collagen/oxidized regenerated cellulose/silver treatment. Wound Repair Regen. 2013;21(2):216-225. doi:10.1111/wrr.12020
- Shu H, Xia Z, Qin X, et al. The clinical efficacy of collagen dressing on chronic wounds: A meta-analysis of 11 randomized controlled trials. Front Surg. 2022;9:978407. doi:10.3389/fsurg.2022.978407
- Schuren J, Bernatchez SF, Tucker J, Schnobrich E, Parks PJ. 3M Coban 2 Layer Compression Therapy: Intelligent Compression Dynamics to Suit Different Patient Needs. Adv Wound Care (New Rochelle). 2012;1(6):255-258. doi:10.1089/wound.2011.0283
NOTE: Specific indications, contraindications, warnings, precautions and safety information exist for these products and therapies. Please consult a clinician and product instructions for use prior to application. Rx only.
As with any case study, the results should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
Patient data and images courtesy of Laura Swoboda, DNP, APNP, FNP-BC, CWOCN-AP.
© Solventum 2024.

