
Rosemary Hill has been a nurse for over 35 years and is the recipient of the Award of Excellence in Practice from the Association of Registered Nurses of British Columbia (ARNBC). She works at Lions Gate Hospital as a Nurse Specialized in Wound Ostomy and Continence (NSWOC). Her past volunteer activities include the role of President for Nurses Specialized in Wound Ostomy Continence Canada (2016-2018). As well, she participates as a member on the BC provincial Skin and Wound committee, Chairs the Provincial Ostomy committee, and is an expert speaker at national and international events. Most recently, volunteer activities have taken her to Argentina where she worked to provide wound education. Ms Hill is a paid consultant for 3M.
Hill_Current-Dialogues-in-Wound-Management_2023_Article-3
Negative pressure wound therapy (NPWT) has traditionally been applied using an adhesive acrylic drape to cover a foam dressing and the peri-wound skin. Use of the adhesive acrylic drape results in a tight seal; however, application of the drape can be cumbersome, and the drape cannot be re-positioned after placement. This can lead to increased time, cost, and material waste. Further, incorrect removal of acrylate adhesives may result in medical adhesive related skin injury, which can harm surrounding skin and cause pain and discomfort for patients.1,2
As an alternative to the traditional acrylate drape, a low-tack hybrid acrylate – silicone adhesive drape was recently developed to help overcome disadvantages of the acrylate adhesive drape, while maintaining a good seal. The drape has an acrylic adhesive coating and a perforated silicone layer. Our facility began using this new hybrid NPWT drape as a first-line drape option, especially in difficult-to-fit anatomical locations, in part, due to its repositionability at initial placement.3 The objective of the current study was to demonstrate the efficiency of the new hybrid drape used in conjunction with NPWT in two complex wound cases.
Methods
3M™ V.A.C.® Granufoam™ Dressing was cut to size and applied to the wound or over skin grafts. In the event of usage over a skin graft, 3M™ Adaptic™ Non-Adhering Dressing was placed prior to positioning the foam dressing. 3MTM V.A.C. DermatacTM Drape was trimmed to cover the dressing with an additional 5-7 cm border to cover intact peri-wound skin and placed over the V.A.C.® Granufoam™ Dressing. The V.A.C. Dermatac Drape was repositioned as necessary upon dressing application, and any wrinkles or creases in the drape were smoothed to prevent air leaks. Dressings were changed every 2-3 days. Continuous negative pressure (3M™ V.A.C.® Therapy) was initiated at -125 mmHg.
Results
V.A.C. Dermatac Drape was utilized in two complex wound cases: deep abdominal wound close to an ostomy and upper arm abscess after a failed fixation (Table 1, Figures 1-2).
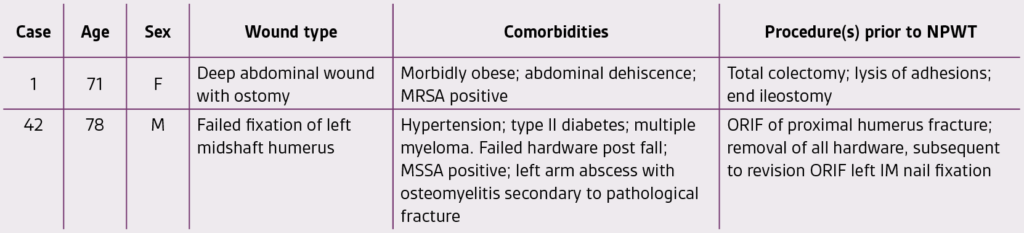
NPWT= negative pressure wound therapy; MRSA = Methicillin-resistant Staphylococcus aureus; FTSG= full-thickness skin graft; STSG = split-thickness skin graft; MSSA = Methicillin-sensitive Staphylococcus aureus; ORIF = open reduction internal fixation; IM = intramedullary; DFU = diabetic foot ulcer

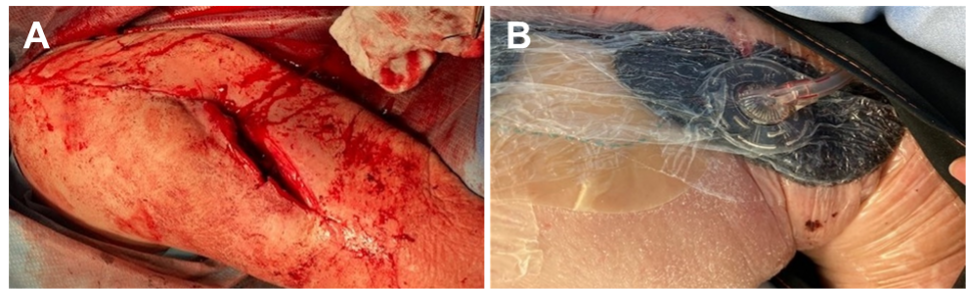
In all cases, a negative pressure seal was maintained between dressing changes and during drape removal, no evidence of epidermal stripping was observed.
Conclusions
In our experience, dressing application and removal were simplified with use of V.A.C. Dermatac Drape versus the standard drape. At dressing changes, both patients experienced improved comfort due to easier removal of the V.A.C. Dermatac Drape.
References
- Fumarola S, Allaway R, Callaghan R, et al. Overlooked and underestimated: medical adhesive-related skin injuries. J Wound Care. 2020;29(Sup3c):S1-S24. doi:10.12968/jowc.2020.29.Sup3c.S1
- Collier M. Minimising pain and medical adhesive related skin injuries in vulnerable patients. Br J Nurs. 2019;28(15):S26-S32. doi:10.12968/bjon.2019.28.15.S26
- Fernandez LG, Matthews MR, Benton C, et al. Use of a novel silicone-acrylic drape with negative pressure wound therapy in anatomically challenging wounds. Int Wound J. 2020;doi:10.1111/iwj.13471
NOTE: Specific indications, contraindications, warnings, precautions and safety information exist for these products and therapies, some of which may be Rx only. Please consult a clinician and product instructions for use prior to application.
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
Patient data and images courtesy of Rosemary Hill, BSN, CWOCN, WOCC (C).
©2022 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. Used under license in Canada.

