
Thalia Attinger is a family nurse practitioner, board certified by the American Nurses Credentialing Center. She obtained her Bachelor of Arts as well as Bachelor in Science and Master of Science dergrees from Georgetown University in Washington, DC. Prior to joining the Center for Wound Healing and Hyperbaric Medicine, where she serves as an in-patient nurse practitioner focusing on the perioperative, post-operative and wound care management, she spent over five years working in the Medical Intensive Care Unit at MGUH.
Attinger_Current Dialogues in Wound Management_2019_Special Spring Edition
INTRODUCTION
As a surgical service, our team traditionally turns to surgical debridement to remove thick exudate. However, with a patient population plagued by ever-worsening morbidity and mortality, surgical intervention is not always possible or even appropriate. Negative pressure wound therapy (NPWT) with instillation and dwell time (NPWTi-d) has been shown to help cleanse the wound bed and prepare the tissue for closure.1,2 The advent of the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing with NPWTi-d provides clinicians with options for patients who may not be surgical candidates by assisting with wound cleansing through the removal of thick exudate and infectious materials. Often these wounds are found over points of pressure, which can create some challenges in both proper application and maintenance of the NPWTi-d dressing. We aim to provide you with some common pitfalls and suggestions to avoid these challenges.
WHEN TO USE V.A.C. VERAFLO CLEANSE CHOICE™ DRESSING
When choosing an intervention, not only must the wound always be considered but also the patient as a whole. For the purpose of this discussion, we will solely focus on wounds over points of pressure, though all of these techniques can be applied to wounds in a variety of locations. We have found that there are 2 subsets of patients who are prime candidates for developing pressure ulcers and as well as being suboptimal surgical candidates: intensive care unit (ICU) patients and decompensated chronically ill patients. ICU patients often spend prolonged periods of time bedbound or chairbound with limited movement and may have an added insult due to the addition of vasopressor medications. These conditions set them up for skin breakdown. In the critically ill patient, as medical instability increases, blood flow to the extremities and the sacrum decreases, causing the wound to become more and more tenuous without safe surgical options, whilst the decompensated chronically ill patient’s activity status can vary greatly. More often than not, these patients seem to lead rather sedentary lives due to a variety of reasons including heart failure, obesity, diabetic wounds, and limb loss. There are also those who suffer from chronic immobility such as those who are wheelchair-bound or bedbound. This patient population is plagued with multiple comorbidities in conjunction with the added risk of inadequate nutritional status making them poor surgical candidates and their capacity to heal even more tenuous. Cardiac and respiratory instability can make an additional trip to the operating room less than ideal. It is in this patient population for whom we find V.A.C. VERAFLO CLEANSE CHOICE™ Dressing to be particularly valuable.
 Figure 1. Sacral ulcer prior to therapy.
Figure 1. Sacral ulcer prior to therapy.
DRESSING POINTS OF PRESSURE
From the shape of the wound bed, the periwound tissue, as well as the high incidence of friction and moisture, a host of challenges arise when dealing with wounds over points of pressure. One challenge is to avoid creating new points of pressure in the process of applying the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing. We will set out to tackle each of these issues and how best to handle them to maximize the chances of achieving a tight and durable seal.
Wound Bed: One of the biggest challenges when placing NPWT over points of pressure is the wound bed itself. These uneven wound beds often have bony prominences that lead to curvatures of differing depths. To achieve optimal outcomes with the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing, our experience has shown the wound contact layer must lie flat against the wound bed. Figure 1 shows such a wound prior to V.A.C. VERAFLO™ Therapy. As seen in Figure 2, a lift in the base layer of foam
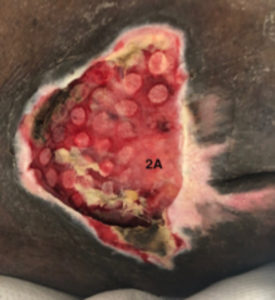 Figure 2. At first dressing change, note area 2A lacks foam imprint.
Figure 2. At first dressing change, note area 2A lacks foam imprint.
led to uneven disruption of slough. Noting the lack of foam indentations and inadequate removal of slough in the lower left-hand portion of the wound bed (marked 2A within Figure 2), the foam’s shape and size were corrected to ensure a proper fit. The difference is clear at the next dressing change (see Figure 3) where there is more uniform granulation tissue throughout the wound bed. To prevent the same mistake from happening, measure the wound bed carefully to ensure that the contact layer is not cut too large because if it cannot fit easily into the wound bed, it will tent. Ideally, the contact layer should be cut in one piece, but if the wound shape is creating a challenge, it may be necessary to cut additional pieces to cover the entire wound bed with a flush layer of contact foam. If the wound requires multiple pieces of foam, ensure there is foam-to-foam contact to allow for an even distribution of fluid and negative pressure. This is especially true over a bony prominence such as a protruding trochanter, knee, or heel. Once there is a properly fitting base layer, we recommend that it is covered with enough of the cover layer foam to put pressure on the contact layer foam, to keep it flush with the wound bed. The top cover layer of foam should at least come up to the level of the periwound skin to ensure adequate padding.
Proper Seal: A proper seal is the key to any good dressing application. However, when it comes to wounds in areas of pressure, there is the added complication of friction and moisture along with the frequent poor periwound skin quality. When dealing with sacral wounds, it is likely that poor quality periwound skin will be encountered in addition to folds and crevices that are prone to moisture. For bony prominences, there will be difficult angles that don’t lend themselves to laying down a nice flat sheet of drape. In both cases, there are a few key steps to take to improve the quality of their seal. As with all V.A.C.® Therapy utilization, ensuring that the periwound skin is clean, dry, and well prepped is crucial. Begin by cleaning the periwound area and removing any loose tissue. Ensure the wound is dried well before using a skin preparation agent. Allowing the skin preparation to dry completely is absolutely imperative. For large wounds, using additional barrier sprays (often used in ostomy care) can also be beneficial. Lining the perimeter of the wound with a hydrocolloid or ostomy barrier ring is invaluable when creating a tight seal in these tricky areas. Once the hydrocolloid or barrier is placed, use strips of V.A.C.® Drape to create a border around the wound (i.e., windowpane the wound edges). This will not only protect the periwound skin, but it will also help to provide a better seal.
 Figure 3. At second dressing change, wound bed after foam corrections made.
Figure 3. At second dressing change, wound bed after foam corrections made.
Friction and Moisture: These areas are also highly prone to friction and moisture and can cause the V.A.C.® Drape to roll and loosen. We have seen this compromise the integrity of the seal. For those wounds on pressure points of the extremities, covering the V.A.C.® Dressing with cast padding or AMD gauze dressing and elastic bandage wraps will help to protect the integrity of the dressing as patients move about. Using offloading devices and strategically placed pillows can also help to protect the wound and the V.A.C.® Dressing. For those wounds on the torso, consider fecal and urinary containment devices (either internal or external pouching) to protect the dressing from incontinence issues. For the obese patient with folds near the dressing, using a product such as InterDry® (Coloplast, Minneapolis, MN) to wick moisture away from the body can be extremely helpful. No matter where the wound is, it is imperative that the integrity of the dressing be checked frequently to identify dressing compromise as early as possible.
Bridging: When treating a wound on a pressure point, it is of the utmost importance that care is taken to place the V.A.C. VERAT.R.A.C.™ Pad in a location that will not create a new pressure point. Proper bridging can be time consuming but is well worth it. For wounds on dorsal surfaces (in particular neck/spine, sacral, and heel wounds), it behooves the wound care team to create a bridge to the ventral side and place the V.A.C. VERAT.R.A.C.™ Pad on an offloaded area. First, line the intact skin with V.A.C.® Drape where it is planned to place the bridging foam to create a protective barrier. Next, ensure that the V.A.C. VERAFLO CLEANSE CHOICE™ contact layer foam, cover layer foam, and the bridge foam are all in tight contact prior to sealing with V.A.C.® Drape. Place the V.A.C. VERAT.R.A.C.™ pad on the ventral side of the patient with the tubing positioned to drain away from the patient as this will help to prevent any obstruction in the tubing.
MULTIDISCIPLINARY APPROACH
As with anything in medicine, the best result comes when a multidisciplinary team works together. Floor nurses are the first line of defense; our institution asks nurses to check the V.A.C.® Dressing and therapy settings every shift, at a minimum. Ideally, the dressing is checked during each assessment so early signs of leakage or destruction of dressing integrity can be identified. Ideally, patients are placed on units that are staffed by nurses well trained in V.A.C.® Therapy and feel comfortable reinforcing dressings or troubleshooting alarms until a member of the surgical team can make an assessment. Additionally, our team relies greatly on the wound ostomy and continence nurses (WOCN) to help come up with creative new ways to tackle hard-to-place dressings. Not only do these nurses have an arsenal of skin preparation techniques and barrier sprays, powders, and rings to help create an optimal seal, they are also able to advise as to the best offloading devices such a specialty beds, boots, foam wedges, etc.
Not to be discounted are the patients and their families and making them active participants in the patient’s care is beneficial in a multitude of ways. For the V.A.C. Ulta™ Therapy unit itself, making them aware of the different alarms and possible problems is key. For any pump that has been “off” or alarming for over 2 hours, it can be helpful to completely remove and reapply the dressing. If patients begin to notice a weakness in the dressing or leaking, they can alert the nursing staff and the problem can be tended to prior to the dressing going down completely. Patient education on offloading and positioning can also be of great value when trying to avoid excess friction.
SETTINGS AND TOPICAL SOLUTIONS
Once there is a tight seal, the next step is to decide on a topical solution and settings. In general, a 20-minute dwell time and 2 hours with -125 mmHg negative pressure is our standard of care. This time frame was chosen due to the fact that polyhexanide plus 0.1% betaine was shown to be more effective at 20 minutes than at 6 minutes.1 We have since applied the time frame to other types of topical solutions. When it comes to topical instillation solution, our team has found that normal saline 0.9% was just as, if not more, effective when used with NPWTi-d than polyhexanide + betaine.2 As a result, our team generally uses normal saline as its first-line agent. For wounds with Pseudomonas, we often opt for acetic acid 1% solution. For those wounds with residual devitalized tissue or severe infection, Dakin’s (dilute sodium hypochlorite) quarter strength solution has been our instill agent of choice.
Finally, one must settle on an instill volume. It is important not to overfill and choose too large a volume or there will be leaks. That said, one must take into consideration the length of bridge and not just the wound bed itself or the opposite problem will result of too little, thereby causing the solution to never reach the wound bed. Using the “fill assist” feature, the provider can start and stop instillation to determine the appropriate amount of volume for each specific wound. Remember this volume may change as the wound heals or if the bridge length is changed. Always reassess the instill volumes when a new dressing is applied.
DISCUSSION
Based on our experience, the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing has unique properties that may provide an option for the cleansing of wounds that may contain infectious material or nonviable tissue. For wounds found on pressure points, achieving an adequate fit, tight seal, and avoiding the creation of new points of pressure can be a challenge.
When changing the dressing, look at the wound bed and assess for areas that did not achieve as much granulation as others. Make corrections to the size and shape of the dressing contact layer accordingly. Utilize the clinical expertise in the institution. The WOCN can help identify additional materials that often will create a better seal and find innovative ways to help offload pressure. Remember that when treating a pressure ulcer, one must take care not to create new points of pressure with the negative pressure dressing. Always check tubing and clip placement to help preserve skin integrity. When placed correctly, the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing can potentially have a remarkable effect on wound healing.
References
1.Kim PJ, Attinger CE, Steinberg JS, et al. The impact of negative-pressure wound therapy with instillation compared with standard negative-pressure wound therapy: a retrospective, historical, cohort, controlled study. Plast Reconstr Surg. 2014;133(3):709-716. doi: 10.1097/01.prs.0000438060.46290.7a.
2. Kim PJ, Attinger CE, Oliver N, et al. Comparison of outcomes for normal saline and an antiseptic solution for negative-pressure wound therapy with instillation. Plast Reconstr Surg. 2015;136(5):657e-664e.

