Valerie has over 40 years of experience in wound care as a clinician, educator, researcher, and administrator of wound care programs. She helped develop and teaches the NPWTi-d (VAC Veraflo) class in Long Beach, CA. She currently is a nurse consultant for a Wound Care & Hyperbaric Program in Long Beach, CA and for KCI An Acelity Company.
Messina_Current Dialogues in Wound Management_2019_Special Spring Edition
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
The use of negative pressure wound therapy with instillation (NPWTi-d, V.A.C. VERAFLO™ Therapy, KCI, an ACELITY company, San Antonio, TX) is growing for patients with complex wounds of varying etiologies and has become the preferred technology for hospitalized wound care patients in my center. If patients are candidates for NPWT, they will most likely receive V.A.C. VERAFLO™ Therapy. Concurrently, early mobility is promoted for hospitalized patients, including those patients with wounds treated with NPWTi-d. As noted in the article by Cain, “Nurse-facilitated early mobility has been reported to reduce incidence of delirium, improve muscle strength, increase independent functional status after discharge, and improve overall quality of life. ”1 Other opportunities to integrate patients’ mobility activities include passive range of motion exercises, dangling legs at the bedside, or sitting/standing at the bedside.1 These mobility activities can often be accomplished on patients with NPWTi-d dressings in place.
Mobilizing and ambulating the patient is an interprofessional responsibility including the physician who orders the mobility status, as well as nurses, and physical and occupational therapists who facilitate ambulation. The wound care nurse has the unique distinction of being the expert on training the patient and staff on the preferred procedure for placement of the dressings, and for adjusting the settings of the V.A.C. VERAFLO™ Therapy System prior to ambulation or mobility of the patient. Our clinical experience has shown that NPWTi-d can be utilized on ambulatory patients. The following techniques for success will hopefully lessen the fear of the dreaded “leaking dressing” or dislodgement of the dressing and help to facilitate early mobility and ambulation for patients.
CASE INTRODUCTION
A young adult male was admitted with a crush injury post-motorcycle accident resulting in a complex wound of the lower extremity. His physical therapy regimen included ambulating around the wound care unit twice daily, and his wound care regimen included application of NPWTi-d to the leg wound to assist with wound cleansing.
What will you do with the therapy/dressing kit that will help to overcome the challenge of keeping the V.A.C. VERAFLO™ Dressing intact during ambulation and mobility and why?
First, prepare the periwound adequately by drying the skin, then apply 3M Cavilon™ Skin Prep (3M, St. Paul, MN) and allow it to get sticky. After this has been done, you may windowpane the periwound with the drape provided in the dressing kit and place (do not pack) the foam into the wound. It is important to take adequate time during the initial drape placement and apply the drape as uniformly as possible, minimizing the amount of wrinkles, folds, or kinks. Place the adhesive side over the foam and apply the V.A.C.® Advanced Drape to cover the foam and intact skin, ensuring that the V.A.C.® Advanced Drape covers at least a 3-5 cm border of intact periwound tissue. Consider gently rubbing the skin preparation over any wrinkles or folds to seal any microleaks that may compromise the seal. Make sure to select an adequate volume of fluid to instill and avoid overfilling as that may increase the risk of leakage. Minimize leaks in anatomical areas where movement is common, like joints or the perineum, by applying the drape in a chevron pattern to provide flexibility.
What ancillary supplies/support will/could you use to overcome the challenge of keeping the V.A.C. VERAFLO™ Dressing intact during ambulation and mobility, and why?
If the dressing kit does not include enough drape to extend on the skin the recommended 3-5 cm beyond the foam, an additional drape may be needed. The addition of a hydrocolloid ring or strip around the wound is helpful to prevent leakage of fluid, especially where skin folds, deep crevices, or ridges are present.
How does plan of care play a role in your action plan?
The placement of the dressing and the V.A.C. VERAT.R.A.C.™ Pad is an important step in order to let gravity work to completely remove the instillation fluid prior to ambulating the patient. You may also consider the V.A.C. VERAT.R.A.C. DUO™ Tube Set to help manage the dwell and removal of fluid. Adjusting the leak alarm to the “high” setting helps to prevent an alarm signal when the dressing is intact. This can be done prior to initial placement of NPWTi-d on the patient.
At the time the patient is to be mobilized or ambulated, make sure that the device is in the “negative pressure mode.” If it is on soak/instill mode, either reschedule the ambulation time, or adjust the mode to remove the instill fluid and place the device in the negative pressure mode. Attaching a note to the machine to alert any staff of this requirement may be helpful. Once the patient is returned to bed, the settings should be returned to the appropriate cycle. It is important to assess the dressing and V.A.C. ULTA™ Therapy System for any leaks or dislodgement, and repair as required post ambulation.
The location of the wound with V.A.C. VERAFLO™ Therapy also affects the needs of the dressing application and plans for mobility. For example, on the upper extremities, applying the dressing to allow for mobility for eating, and other activities of daily living, need to be addressed. On the trunk, application to prevent dislodging during mobility in and out of bed is a concern. For lower extremities, the concern is making sure the dressing and tubing do not present a trip hazard or safety risk for falling or dislodging the dressing by pulling on the tubing. Making sure additional equipment is available is also necessary, such as a sling for a hand wound, or an IV pole or walker to place the pump on for all patients ambulating.
What therapy settings will you use?
i. Does the topical wound solution choice influence these?
I have found the use of Dakin’s antimicrobial irrigation solution may require additional care to prevent leakage at the wound’s edge in order to minimize damage to the periwound skin.
ii. Does the dressing that has been chosen influence your selected settings?
I have found that the use of the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing may require placement of a hydrocolloid strip or ring to help avoid leakage as the foam is less flexible and more prone to leakage at the wound’s edge and where skin folds, deep crevices, or ridges are present. This can help minimize the potential for periwound skin maceration and irritation.
Is there anything you can/should share with the floor nurses, patients, or the patient’s family members, or is there anything you can/should ask of them?
Patient and family education includes ensuring that the patient, who is an independent ambulator, asks for assistance when preparing to ambulate or mobilize in or around the bed. The nurses and physical therapists are trained to make sure the system’s setting is on “negative pressure” mode and the instill fluid has been removed when ambulating, to help decrease the risk of leakage. Attaching the V.A.C. ULTA™ Therapy System to a pole or walker that can be rolled safely with the patient may be needed. Ensure tubing and the power cord are secured to prevent a trip hazard and so as not to interfere with ambulation.
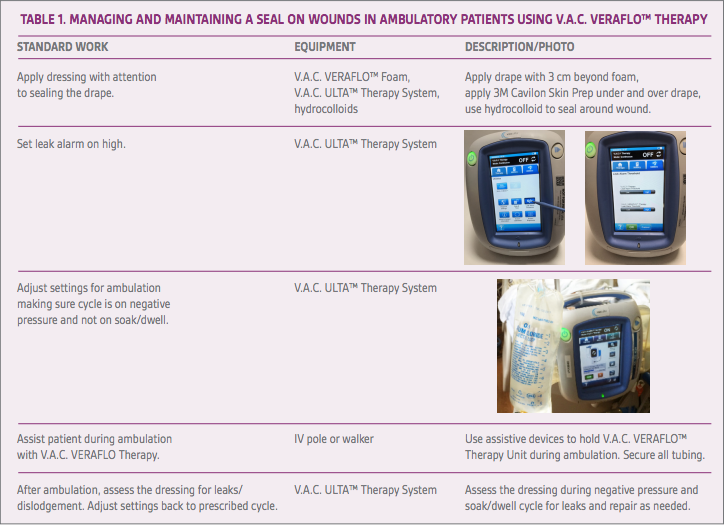
Our experience with using NPWTi-d has shown that leakage and dislodging of the dressing during mobility in or out of bed, or ambulation, can often be minimized or prevented with proper dressing placement, utilizing additional hydrocolloid strips, and making sure the NPWTi-d is in the negative pressure mode during ambulation (see Table 1). Our experience has also shown that education and training for patients and staff are key for successful outcomes using this therapy.
References
Cain C. No time for early mobility? Am J Crit Care. 2018;27(3):204. doi: 10.4037/ajcc2018441.