N/A_Current Dialogues in Wound Management_2016_Volume 2_Issue 2
INTRODUCTION
While negative pressure wound therapy with instillation and dwell time (NPWTi-d) is used by a variety of clinicians in hospitals, those responsible for wound care (primarily nurses) are relatively uninformed regarding the clinical and technical aspects of this therapy.
To address this knowledge gap, a panel meeting of one plastic surgeon (a wound care specialist) and 11 wound care nurses with extensive NPWTi-d experience was convened in Denver on November 19–20, 2015. Panelists (all from North America) were chosen by the sponsor, Acelity, based on their level of clinical experience with NPWTi-d. During the meeting, each participant discussed literature previously provided by the sponsor (13 peer-reviewed NPTWi-d studies), reviewed their own clinical experience and shared suggestions for using NPTWi-d. Recommendations were organized, summarized, approved by the panel and published as a supplement to the April 2016 issue of Ostomy/Wound Management
This article presents a brief summary of the panel recommendations.
WOUND TYPES MOST SUITED FOR NPWTi-d
NPWTi-d is primarily suited to prepare surgical or nonsurgical wounds for delayed primary closure.
NPWTi-d may be considered as part of the wound treatment strategy (in conjunction with debridement and appropriate systemic antibiotics) if the goal is to promote cleansing or granulation.
PATIENT MANAGEMENT: CHALLENGES
Panelists identified several challenges in managing patients with NPWTi-d and provided recommendations to address each of these challenges.
) Difficulty maintaining a seal. The cyclical instillation of solutions with NPWTi-d can cause difficulties in maintaining a seal. Recommendations for this challenge can be found in Figure 1.B) Correctly using the NPWTi-d device. By including a simple checklist to be implemented at each shift, hospitals can reduce incorrect use of the NPWTi-d device (for example, turning off the device when an alarm sounds and interrupting therapy rather than troubleshooting the problem). Panelists suggested basic troubleshooting techniques such as ensuring the device is plugged in and turned on with the adapter and power cord and all other connections securely in place; having an extra empty canister at the bedside at all times; frequently checking the canister and solution bag and changing either when required; verifying that device settings are correct; and checking the dressing site to ensure the seal is maintained.C)Maintaining continuity of care across shifts. Educating all nurses in management of NPWTi-d may not be realistic. The panel shared a number of steps that can be taken to help ensure successful management across all shifts:•Education: Initial bedside training helps to establish clear understanding and expectations regarding assessment, monitoring and care. Ongoing quarterly or semi-annual training should be regularly provided to ensure clinical staff remain up to date and introduce new hires to NPWTi-d. Manufacturers’ training representatives can be used as a resource when appropriate.•Specialization: Assigning more complex tasks such as application and dressing changes to wound care nurses and less challenging tasks (canister changes) to general nurses allows each group to more easily acquire the necessary skills and carry out these tasks quickly and effectively. Similarly, ensuring that the same clinician changes dressings for a particular patient and designating specific nurses as “champions” in charge of NPWTi-d troubleshooting can help ensure patients receive high-quality continuous care.•Documentation: Consistent and thorough documentation in patients’ medical record also supports continuity of care.•Cooperation: Prescribers and wound care nurses should work together closely to ensure high-quality NPWTi-d care.D) Providing access to appropriate supplies. A resource box containing accessories needed to apply the product should be accessible to all nurses. Such a box can be especially helpful for staff who may not be familiar with NPWTi-d and its various components. The box may be kept in the OR near the
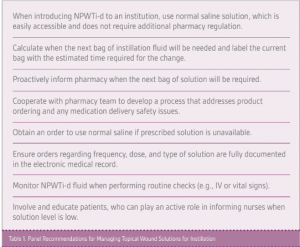
NPWTi-d device and supplies. These boxes can accompany nurses when they are checking on patients receiving NPWTi-d or need help troubleshooting problems.E) Ensuring accessibility of instillation solutions. NPWTi-d instillation solutions must be obtained through the pharmacy, which may create difficulties in accessing solutions when needed. Table 1 summarizes panel recommendations for managing solutions.F)Selecting appropriate instillation volume. For nurses new to this task, the “fill assist” mechanism on the device (which allows a nurse to monitor initial wound fill by manually starting and stopping instillation to determine the correct instill volume after the dressing is applied) can help determine the volume of solution to be instilled during each cycle. Volume may also be approximated by using the calculation suggested by the manufacturer. Another approach is to instill just enough solution to visibly saturate the foam and reduce the amount being instilled by approximately 10% to 20% if the foam becomes oversaturated.G)Minimizing pain during dressing changes. Although some evidence suggests that pain during dressing changes may be less with NPWTi-d compared to standard NPWT, dressing changes can sometimes be painful. The panel drew on its collective experience to develop several options to help address potential discomfort or pain during a dressing change:•Before initiating therapy, develop a pain management care plan with the patient. Use a pain scale for the patient to identify pain before therapy and at the end of the procedure so pain can be monitored and addressed. Ongoing assessment of what was painful (e.g., removal of the drape or foam) and addressing this with patients validates concerns and helps relieve anxiety.•Use the “dressing soak” feature on the NPWTi-d system before dressing changes, which will fill the foam with fluid and allow for easier dressing removal.•Administer oral or intravenous pain and/or anxiety medication per provider order at least 30 minutes before dressing change.•For patients who may have pain during the instillation cycle, consider setting frequency of the cycle to coordinate with the ordered pain medication schedule.•Education about what to expect during the dressing change goes a long way in pain management.
References
To obtain the full version of these recommendations, visit the Ostomy/Wound Management journal website at http://www.o-wm.com/home

