Amy Law joined Acelity eleven years ago, and has held various roles in Marketing, IT and Operations. She currently leads Global Health Economics Outcomes Research, Reimbursement and Government Affairs. Her team is focused on real world evidence development to help secure market access and reimbursement for Acelity’s portfolio. She also works actively with partners in DC to secure policies that foster innovation and quality patient outcomes in wound care. Prior to joining Acelity, she was a management consultant, leading engagements in South Korea, Germany, Australia, and the US. Amy holds a degree in Economics from the London School of Economics and an MBA from Harvard Business School.

Leah Griffin is a biostatistician and outcomes researcher with expertise in global healthcare, health economics, and outcomes research. She is a published author and an experienced health and industry expert with over 16 years of thought leadership and hands-on experience in clinical and economic analyses. At the start of her career, she spent 11 years as a biostatistician at Wake Forest University Baptist Medical Center, where she developed expert knowledge in conducting and administering randomized controlled trials and clinical outcomes research. Leah has been with KCI for 5 years where she has focused on the expansion of the body of supporting clinical and economic evidence. Leah commands comprehensive knowledge and expertise in research design, study development and analysis methodology.
Law and Griffin_Current Dialogues in Wound Management_2019_Volume 5_Issue 2
ABSTRACT
BACKGROUND
Complications in the healing of acute wounds may yield challenges to wound management and impact healthcare cost-containment. This study presents a comparative-effectiveness study to evaluate the value proposition of 2 collagen-containing wound dressings: PROMOGRAN PRISMA™ Matrix and a bovine collagen extracellular matrix (ECM) in matched cohorts of patients undergoing treatment for surgical or traumatic wounds.
METHODS
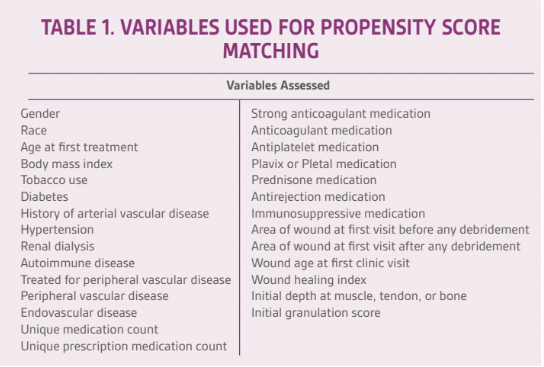
Data extracted from the US Wound Registry identified patients with surgical or traumatic wounds treated with either dressing and included patients with complete data records (n = 6044). Twenty-nine variables including age, BMI, tobacco use, and diabetes were considered in propensity score matching to develop a case-matched cohort of 664 patients (n = 332 patients/product group). Two-sample t-tests were used for continuous variables, and Chi-Square or Fisher’s exact test was used for categorical
RESULTS
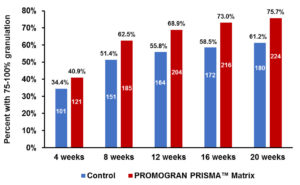
A significantly higher percentage of the PROMOGRAN PRISMA™ Matrix reached 75%-100% granulation with zero depth as compared to the ECM group (83.5% vs. 67.0%, p<0.0001). The PROMOGRAN PRISMA™ Matrix group had significantly higher numbers of wounds reaching 75%-100% granulation at 8 weeks (p=0.0063), 12 weeks (p=0.0010), 16 weeks (p=0.0002) and 20 weeks (p=0.0002). There was no difference in the number of dressing applications between the two cohorts. However, the duration of dressing use was significantly longer in the PROMOGRAN PRISMA™ Matrix group (12.8 days vs. 8.9 days, p=0.0210), and there were more days between dressing changes (3.5 days v. 2.3 days, p=0.0012).
CONCLUSIONS
PROMOGRAN PRISMA™ Matrix appears to offer afford improved healing rates and reduced time to granulation relative to bovine collagen ECM dressings in high-risk patients with surgical or traumatic wounds.
INTRODUCTION
The popularity of collagen for wound healing and cosmetic surgeries is fueling forecasted market compound annual growth rate of 5.23% through 2023.1 As collagen dressing use increases, evaluation of real-world evidence to assess differences between products can benefit healthcare providers. This study evaluated the value of two collagen-containing wound dressings: PROMOGRAN PRISMA™ Matrix and bovine collagen extracellular matrix (ECM, PURACOL® Microscaffold™ Collagen Wound Dressing, Medline Industries, Inc., Northfield, IL) in matched cohorts of patients undergoing treatment for acute and surgical wounds.
METHODS
An electronic healthcare database (United States Wound Registry or [USWR]) was used to identify acute and surgical wounds with complete data records who received either bovine collagen ECM (control) or PROMOGRAN PRISMA™ Matrix (ORC). Propensity score matching across 29 variables was performed to construct a case-matched cohort (Table 1).2A logistic regression model was used to model treatment (ORC or control) as the outcome with 29 variables included in the model. The predicted values from the logistic regression model were the propensity scores. Nearest neighbor matching was used to find 1:1 matches between the PROMOGRAN PRISMA™ Matrix and control cohorts. The subsequent matched cohorts were then compared. Two-sample t-tests were used for continuous variables, and Chi-Square or Fisher’s exact test was used for categorical variables to compare PROMOGRAN PRISMA™ Matrix and bovine collagen ECM post-matching.
RESULTS
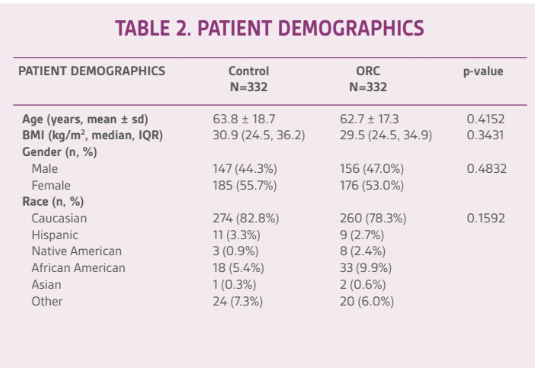
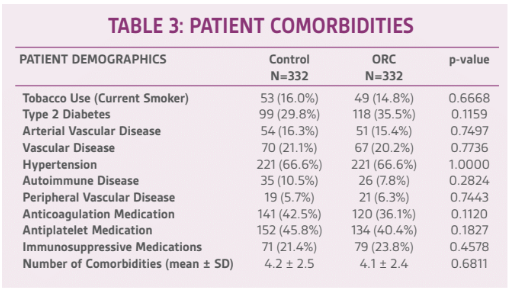
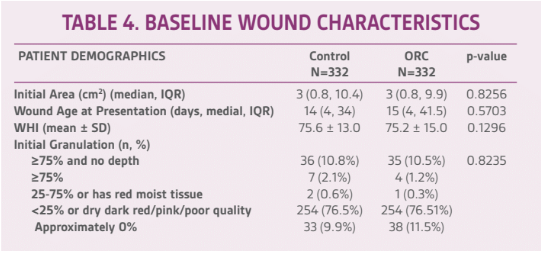
Patient demographics and baseline wound characteristics were similar between the control and ORC groups (Tables 2-4). Patients included in this study had an average of >4 comorbidities including diabetes (30%) and hypertension (66%). Wounds were a median size of 3 cm2 and approximately two weeks old at the time of presentation. Length of follow-up was up to 16 weeks, and included initial clinic visit to final clinic visit. There were no significant differences in length of follow-up between the two cohorts with median (IQR) of 58.5 days (28.5, 126) for PROMOGRAN PRISMA™ Matrix and 55.0 (28-122) for control (p=0.2505).
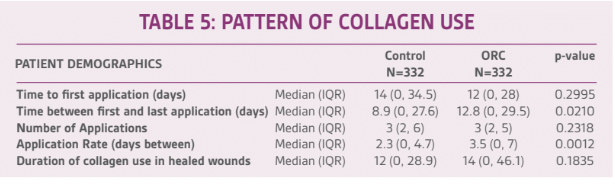
The patterns of collagen use are reported in Table 5. PROMOGRAN PRISMA™ Matrix was used for a significantly longer duration (time between first and last dressing application) than the control dressing (12.8 days vs. 8.9 days, p=0.021). There was also a significant difference in the application rate (days between collagen applications) with ORC applied every 3.5 days, and ECM changed every 2.3 days (p=0.0012). There were no significant differences in the time to the first collagen application, number of applications, or duration of collagen use in patients with healed wounds.
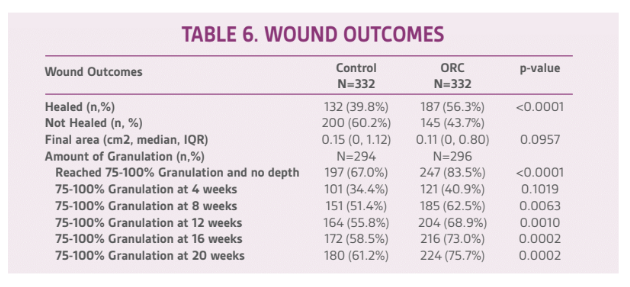
When evaluated as healed or not healed at last clinic visit as the outcome of interest, there was a significant difference between the cohorts with 56.3% of ORC wounds healed versus 39.8% of control wounds healed (p<0.0001) (Table 6). The final area of the wound was smaller in the ORC group 0.11cm2) than the control group (0.15cm2, although this did not reach significance (p=0.0957). A significantly higher percentage of wounds in the ORC group reached 75%-100% granulation with zero depth compared to the control group (83.5% vs. 67.0%, p<0.0001). Additionally, statistically significant differences were found in the percentage of wounds reaching 75%-100% granulation at 8 weeks (p=0.0063), 12 weeks (p=0.0010), 16 weeks (p=0.0002) and 20 weeks (p=0.0002), with higher percentages recorded in the ORC group (Figure 1).
DISCUSSION
While much of the literature is focused on the use of collagen dressings to jump-start stalled or chronic wounds, they can also play a key role in healing surgical wounds (including deep surgical debridement or amputation of a formerly chronic wound) and traumatic wounds, particularly for patients where multiple comorbidities are present and the risk of wound breakdown is higher. In this patient population, these factors likely influenced the practitioner’s decision to use collagen.
Although the study results suggest the majority of patients achieve 75-100% granulation by eight weeks, the relatively low percentage of patients designated as healed at the time of last clinic visit supports discussions about the low real-world healing rates of highly compromised patients.3 This finding may also support the argument that complete wound closure may not always be an appropriate endpoint in clinical studies and brings forward the relevance of other options such as patient-centered endpoints and alternate clinical endpoints aimed at wound volume reduction over time.4 Overall, this comparative effectiveness study found that PROMOGRAN PRISMA™ Matrix appears to afford improved healing rates and reduced time to granulation relative to the bovine collagen ECM control dressing in high-risk patients with surgical and traumatic wounds.
References
1.The collagen market is estimated at USD 3.5 billion in 2018 and projected to grow at a CAGR of 5.2%, to reach USD 4.6 billion by 2023. Web site. http://www.prnewswire.com. Accessed April 12, 2019.
2.D’Agostino R. Tutorial in biostatistics propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Statist Med. 1998; 17:2265-2281.
3.Fife CE, Eckert KA, Carter MJ. Publicly reported wound healing rates: the fantasy and the reality. Adv Wound Care (new Rochelle). 2018;7(3):77-94.
4.Driver VR, Gould LJ, Dotson P, et al. Evidence supporting wound care end points relevant to clinical practice and patients’ lives. Part 2. Literature survey. Wound Rep Reg. 2019;27(1):80-89.