
Dr. Robert Klein completed podiatric medical school in Chicago at the Rosalind Franklin University of Medicine and Science, Scholl College of Podiatric Medicine. Dr. Klein continued his surgical training as the Chief Resident at Michigan Health Center in Detroit. He is a Clinical Assistant Professor in the Department of Surgery at the University of South Carolina School of Medicine (USCSOM) Greenville and specializes in wound care, limb preservation, and Dr. Klein is a consultant for 3M.
Klein_Current Dialogues in Wound Management_2021_Article_1
Diabetic foot wounds are a serious complication of diabetes. Patients with diabetes have a 15% to 20% lifetime risk of developing a diabetic foot ulcer (DFU), and these ulcerations lead to more than 80,000 amputations per year in the United States.1-5 The risk for amputation increases as the DFU worsens; nearly 84% of patients who undergo lower limb amputation due to diabetes also had a DFU present prior to the amputation.6 Diabetic foot ulcerations develop from a variety of risk factors as denoted in Table 1, which is a partial list of the more common risk factors.

Classification Systems for Diabetic Foot Ulcerations
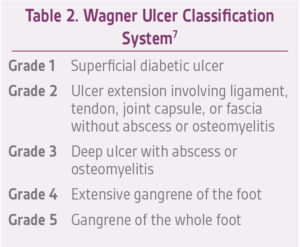
There are several classification systems for diabetic foot ulcerations including the Wagner Classification System, the University of Texas Diabetic Wound Classification System, Site, Ischemia, Neuropathy, Bacterial Infection, and Depth (SINBAD) classification, Wound, Ischemia, and foot Infection (WIfI), and the International Working Group on the Diabetic Foot (IWGDF) Classification System. DFUs are typically classified by the depth of the wound and the presence of infection. Our center uses the Wagner Classification System for diabetic foot ulcerations (Table 2).
Neuropathy
Peripheral neuropathy is one of the major causes for the development of diabetic foot wounds.8 Peripheral neuropathy can manifest itself as sensory neuropathy, motor neuropathy, and autonomic neuropathy. With sensory loss the patient, many times, is unaware when skin breakdown is beginning to develop or has already occurred. Calluses can develop under bony prominences which can lead to a hemorrhagic keratosis and eventual ulceration (Figure 1).

Motor neuropathy affects the intrinsic muscles in the foot which can lead to deformity, including hammertoe deformities and prominent metatarsal heads, which in turn can cause diabetic foot ulceration. Autonomic neuropathy causes dry, cracked skin, as well as decreased sweating of the skin, making the patient vulnerable to skin breakdown and possibly infection.9 The neurologic status of patients with DFUs should be checked using the Semmes-Weinstein monofilament test to determine if the patient has lost their protective sensation.
Peripheral Arterial Disease
Peripheral arterial disease (PAD) is narrowing, stenosis, and/or occlusion of the lower limb arteries. PAD is a major contributing factor to the development of DFUs. Tissue loss can develop from ischemia because of large vessel disease or small vessel disease, especially the smaller arterial vessels below the knee.5,10 Signs and symptoms of PAD include pain when walking or resting, tight, shiny skin, thickened and brittle toenails, lack of hair growth on the foot or leg, skin that feels cool to the touch, pallor on elevation, and dependent rubor. DFUs in the presence of PAD can lead to lower limb amputation, especially when significant tissue loss and infection has occurred (Figure 2). A non-invasive arterial duplex with ankle brachial index and toe pressures is recommended for patients with DFUs with non-palpable distal pulses, and/or in DFUs that fail to heal with conventional wound care. Patients with abnormal non-invasive arterial studies should be referred to a vascular surgeon for further evaluation and possible vascular intervention.

Foot deformity
Motor neuropathy causes atrophy of the intrinsic foot muscles and muscle imbalance. Common deformities seen in the diabetic foot include hammertoe deformities, claw toe deformities, prominent metatarsal heads, plantar fat pad atrophy, pes cavus (high arch), Charcot foot deformity, and equinus (limited upward bending motion of the ankle joint).11-13 These structural deformities can lead to abnormal mechanical pressures and skin breakdown. Typical areas where DFUs develop include the plantar aspect of the forefoot underneath the metatarsal heads, the dorsal proximal interphalangeal and distal interphalangeal joints of the toes, and the plantar midfoot (Figure 3).

Poorly controlled diabetes mellitus and Impaired healing
Hyperglycemia leads to poor wound healing potential. High blood glucose levels impair white blood cell function. White blood cells play a critical role in the immune system; thus, when white blood cells are not functioning correctly in the presence of poorly controlled diabetes, the patient is more prone to infection and the inability to heal wounds. Impaired wound healing can lead to additional complications from DFUs including cellulitis and osteomyelitis.14,15
Osteomyelitis
The longer a DFU remains open, the higher the risk for the patient to develop osteomyelitis. Osteomyelitis can be a devastating complication that can lead to debridement of bone and/or amputation. Clinicians should have a high suspicion for osteomyelitis in DFUs that probe to bone (Figure 4). Tests to aid in the diagnosis of osteomyelitis include plain film x-rays, computerized tomography (CT), nuclear medicine, magnetic resonance imaging (MRI), and inflammatory markers including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). The author recommends a baseline x-ray in patients that present with a DFU, and advanced imaging as needed for those wounds that fail to respond to conventional wound care or extend to deeper structures, including a positive probe to bone.

Real World Approach to Managing Diabetic Foot Ulcerations
The primary goal in the management of DFUs is to close the wound as quickly as possible and to prevent amputation. Wound care should include debridement, offloading, treating any underlying infection and/or inflammation, management of wound exudate, and promoting the advancement of wound edges.16,17
Debridement of the wound may entail autolytic, enzymatic, and/or surgical debridement.18 Offloading is an essential component to the management of DFUs and total contact casting remains the gold standard. Controlled ankle motion (CAM) walkers should be considered in patients where total contact casting is not an option, as well as the use of wheelchairs, walkers, and modified shoes.19
Advanced wound care dressings can aid in wound healing. The use of PROMOGRAN PRISMA™ Matrix Wound Dressing (Systagenix Wound Management Ltd., Gargrave, UK) has been shown to be very effective in managing diabetic foot ulcerations (Figure 5a).20 The use of negative pressure wound therapy (NPWT, V.A.C.® Therapy or SNAP™ Therapy System, depending on wound size, Figure 5b and 5c) may promote wound healing by managing excess wound exudate.

Conclusion
Diabetic foot wounds are a serious complication of diabetes that can lead to amputation. The causes of DFUs are multifactorial and understanding the pathophysiology and etiology of diabetic foot wounds is essential to treating these complex wounds.
References
1. Armstrong DG, Lavery LA. Diabetic foot ulcers: prevention, diagnosis and classification. Am Fam Physician. 1998;57(6):1325-1332, 1337-1328.
2. Bowering CK. Diabetic foot ulcers. Pathophysiology, assessment, and therapy. Canadian Fam Physician. 2001;47:1007-1016.
3. Schaper NC, Apelqvist J, Bakker K. The international consensus and practical guidelines on the management and prevention of the diabetic foot. Curr Diab Rep. 2003;3(6):475-479.
4. Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Pogach LM. Preventive foot care in diabetes. Diabetes Care. 2004;27(Suppl 1):S63-S64.
5. Jeffcoate WJ, Harding KG. Diabetic foot ulcers. Lancet. 2003;361(9368):1545-1551.
6. Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation. Basis for prevention. Diabetes Care. 1990;13(5):513-521.
7. Oyibo SO, Jude EB, Tarawneh I, Nguyen HC, Harkless LB, Boulton AJ. A comparison of two diabetic foot ulcer classification systems: the Wagner and the University of Texas wound classification systems. Diabetes Care. 2001;24(1):84-88.
8. Boulton AJ. The diabetic foot: grand overview, epidemiology and pathogenesis. Diabetes Metab Res Rev. 2008;24(Suppl 1):S3-6.
9. Sumpio BE. Contemporary evaluation and management of the diabetic foot. Scientifica (Cairo). 2012;2012:435487.
10. Akbari CM, LoGerfo FW. Microvascular changes in the diabetic foot. In: Veves A, Giurini JM, LoGerfo FW, eds. The Diabetic Foot. 1st ed. Totowa, NJ: Humana Press; 2002:99-112.
11. Bus SA, Maas M, Michels RP, Levi M. Role of intrinsic muscle atrophy in the etiology of claw toe deformity in diabetic neuropathy may not be as straightforward as widely believed. Diabetes Care. 2009;32(6):1063-1067.
12. van Schie CH, Vermigli C, Carrington AL, Boulton A. Muscle weakness and foot deformities in diabetes: relationship to neuropathy and foot ulceration in caucasian diabetic men. Diabetes Care. 2004;27(7):1668-1673.
13. Heitzman J. Foot care for patients with diabetes. Top Geriatr Rehabil. 2010;26(3):250-263.
14. Wild T, Rahbarnia A, Kellner M, Sobotka L, Eberlein T. Basics in nutrition and wound healing. Nutrition. 2010;26(9):862-866.
15. Sharp A, Clark J. Diabetes and its effects on wound healing. Nurs Stand. 2011;25(45):41-47.
16. Schultz GS, Sibbald RG, Falanga V, et al. Wound bed preparation: a systematic approach to wound management. Wound Repair Regen. 2003;11 Suppl 1:S1-28.
17. Chadwick P, Edmonds M, McCardle J, Armstrong D. Best Practice Guidelines: Wound management in diabetic foot ulcers. Wounds Int. 2013:1-23.
18. Lebrun E, Tomic-Canic M, Kirsner RS. The role of surgical debridement in healing of diabetic foot ulcers. Wound Repair Regen. 2010;18(5):433-438.
19. Snyder RJ, Hanft JR. Diabetic foot ulcers – effects on quality of life, costs, and mortality and the role of standard wound care and advanced-care therapies in healing: a review. Ostomy Wound Manage. 2009;55(11):28-38.
20. Gottrup F, Cullen BM, Karlsmark T, Bischoff-Mikkelsen M, Nisbet L, Gibson MC. Randomized controlled trial on collagen/oxidized regenerated cellulose/silver treatment. Wound Repair Regen. 2013;21(2):216-225.
21. Blume PA, Walters J, Payne W, Ayala J, Lantis J. Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: a multicenter randomized controlled trial. Diabetes Care. 2008;31(4):631-636.
Patient photos courtesy of Robert J. Klein, DPM, FACFAS, CWS
NOTE: Specific indications, contraindications, warnings, precautions and safety information exist for these products and therapies. Please consult a clinician and product instructions for use prior to application. Rx only.
© 2021 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. PRA-PM-US-02888 (01/21).
