Mary Anne is a certified wound nurse that works for an abdominal reconstruction service at a level I trauma center in St. Paul Minnesota. She has been a nurse for 30 yrs and worked in trauma and surgical ICU and was a flight nurse, but her real passion has been identified, caring for the patient with abdominal wounds and enteric fistula! She is a mother of four and a new grandmother, she lives in small town with her husband Andy, kids and her dog Casey Brown.

Dr. Dries is trained in electrical and biomedical engineering before completing medical school at the University of Chicago. Dr. Dries subsequently trained in General Surgery with added qualifications in Critical Care. He has been at Regions Hospital in St. Paul and the University of Minnesota since 1999. Current research interests are inflammatory changes in the lung as mediated by mechanical ventilation, physiology of mechanical ventilation in the setting of critical illness and resuscitation of the critically ill patient. Dr. Dries has worked for the past several years in development of the CARS Program at Regions Hospital for patients with fistulas and complex abdominal problems. Dr. Dries is the Division Medical Director for Surgical Care for HealthPartners Medical Group and Chief of Surgery at Regions Hospital, the Level I Adult and Pediatric Trauma and Burn Center in St. Paul. He is also Professor of Surgery & Anesthesiology, Clinical Adjunct Professor of Emergency Medicine and the John F. Perry, Jr. Chair of Trauma Surgery at the University of Minnesota.
Obst and Dries_Current Dialogues in Wound Management_2017_Volume 3_Issue 3
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
Where should wound care start? Evaluating the chart, or assessing the patient? How much should you know about a patient to best treat a wound?
Our Complex Abdominal Reconstruction Service (CARS) team treats patients with extreme abdominal wounds and underlying structural defects including the open abdomen, massive loss of domain, and enteric fistulas. Our team provides holistic care to this complex population during the months needed to prepare for definitive surgical repair. We assess the patient and evaluate the medical history to prepare for multiple aspects of wound care including dressing selection, nicotine cessation, abdominal wall support, physical strengthening, and nutrition. One role of the wound care nurse on the team is to maximize healing during this pre-surgical period. Our CARS program typically results in a successful repair of the abdomen, but team members from multiple disciplines are required for success – the most important team member is the patient!
LOCAL WOUND BED EVALUATION
Wound bed evaluation requires further study! A common standard is to monitor wound size by length, width and depth to identify trends in wound contraction and healing. Examination of the wound bed and adjacent skin are equally as important; however, this essential data is often not documented or communicated. The wound bed and adjacent skin health are key indicators for the wound healing process. In the acute care setting the wound is also evaluated by the team for tissue response to treatment and dressing selection. Holistic patient health becomes a key factor in success.
DRESSING SELECTION AND MANAGEMENT
Critical evaluation of the wound bed and the structures beneath the wound bed should drive dressing selection. Gauze dressing therapy is the historical standard of practice in the acute wound care and gauze dressings are certainly still in use. Technical advances in dressings have given wound care practitioners many alternatives, including foams, films, hydrocolloids, and alginates. A Cochrane Database review by Vermeulen et al.1 concluded that foam dressings appear to be preferable to gauze for pain reduction, patient satisfaction and required nursing time for wound care. In many cases composite dressings or a hybrid of dressing therapies within the same patient’s wound bed will yield the best results. Critical thinking at the bedside with a full understanding of the patient’s holistic health and structures beneath the wound bed are necessary for safe dressing decisions.
NICOTINE CESSATION
It is well documented that nicotine and carbon monoxide exposure affect blood flow to the wound, platelet behavior, and the overall wound healing effectiveness.2 An aggressive nicotine cessation program with weekly urine testing for nicotine has been successful in our outpatient patient population. Our program focuses on weekly test result feedback to the patient and primary provider engagement. We have also found tools like CeDAR app (Carolina Equation for Determining Associated Risks) predict the risks and financial costs of wound related problems following complex hernia repair. The CeDAR app is easy to use and quickly identifies modifiable risk factors that the patient can address to help improve outcome such as nicotine cessation. The app encourages compliance by showing patients their risk for wound problems after surgery.
ABDOMINAL WALL SUPPORT
Support garments that are designed to relieve tension which distracts wound margins will increase patient comfort and assist the healing process. A support garment will decrease lateral stressors and protect the wound and the underlying structures from external injury. Offloading of lateral and downward strainis needed to optimize the healing process.
 Figure 1:A support garment reduced this patient’s abdominal wall tension and allowed a 10-year chronic wound to heal
Figure 1:A support garment reduced this patient’s abdominal wall tension and allowed a 10-year chronic wound to heal
NUTRITION
Clinicians agree that patients with optimal nutrition have better wound healing. However, the means to evaluate nutritional status is not well defined.3 The team approach is mandatory for assessing nutritional status. A wound care provider’s assessment of wound size and composition complemented by dietician evaluation will provide high-risk patients with solid recommendations. Engaging the surgeon and internal medicine provider will assist in patient compliance. Each practice area can bring their knowledge to bear on the patient’s fluid and caloric/protein needs and vitamin and mineral supplementation.
NUTRITION: WHERE DO YOU START?
Laboratory testing including electrolytes, pre-albumin, hemoglobin A1c, C-reactive protein, and a complete blood count can give you a good starting point. Food logs and body weight mass index with a comparison to the ideal body weight of the patient are utilized by registered dieticians to evaluate specific nutrient requirements. Changes from ideal body weight help drive nutritional supplementation including fluids, energy or caloric needs, protein, and electrolytes. Generally, patient nourishment challenges fall into three groups; the healthy patient, malnourished/ overweight and malnourished/underweight. Registered dieticians use a formulaic approach to calculate the needed grams of protein and supplements that should be taken within a 24-hour period. Understanding safe supplementation of electrolytes and vitamins with methods of delivery is the expertise of the nutritionist.
Malnourished or under nourished patients will have healing inadequacies. Our CARS team goal is to establish and maintain oral nutrition during the healing process, however our team does utilize multiple of methods of nutrition delivery. For example, a patient may be on parental nutrition until appropriate enteral nutrition can be implemented via nasojejunal tube or via a percutaneous gastric tube. The decision on tube type depends on the patient condition and ability to take oral supplements. Several days of cross over nutrition delivery between routes of administration may occur. Meeting nutritional requirements while making a steady transition from parental nutrition to enteral nutrition and finally oral nutrition is our goal.
CASE STUDY: WOUND MANAGEMENT FROM THE INSIDE OUT
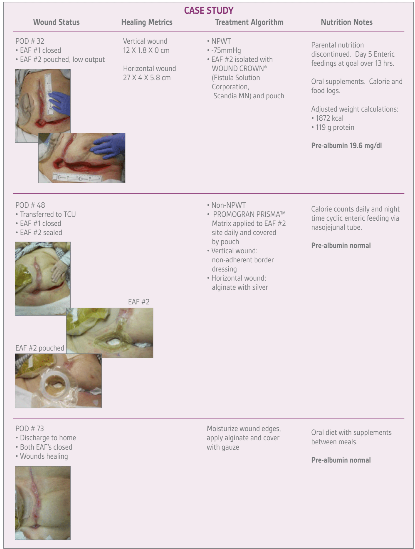
This case study shows the relationship between improved nutrition and wound healing as the patient transitions from parental nutrition to enteral nutrition to oral nutrition. Although no single metric is an ideal indicator for global nutritional health, pre-albumin measurement is useful for monitoring trends in nutritional improvement or failures in an established patient. This case study is an example of both external wound healing and internal healing that happen after surgery.
A 73-year-old female patient had elective ventral hernia repair with retrorectus mesh and bilateral transverses abdominis release. One week later a small bowel enterotomy was noted on an abdominal CT scan. An exploratory laparotomy, small bowel resection, and explantation of abdominal wall mesh initiated the wound care sequence that follows. Pre-albumin levels are color coded red, yellow, and green at each point in time to indicate nutritional concern.
NUTRITION: PATIENT PARTICIPATION
Wound progression in this patient is an excellent example of a patient with poor nutrition and a declining wound whose wound healing processes responded well to improved nutrition. In situations like this, wound healing will be minimal until nutrition can be improved. To reduce risk of wound regression post-discharge, establish a food log as part of the patient’s routine as early as possible. This practice should be established before the patient returns home.
CONCLUSION
Wound care preparation should include evaluation of both the patient and the chart. This comprehensive approach will assist preparation of a successful wound care plan tailored to the patient’s specific needs. Complex abdominal wounds require an individualized approach that comprehends all aspects of wound care including dressing selection, nicotine cessation, abdominal wall support, physical strengthening, and nutrition. Patience and patient participation during the months needed to prepare for final surgical repairs are necessary for the best outcomes. We always tell our patients that they are the most important player on the team, because “The only person on the team who is at every dressing change, is you!”
References
1.Vermeulen H, Ubbink D, Goossens A, Vor R, Legemate D. Dressings and topical agents for surgical wounds healing by secondary intention. Cochrane Database Syst Rev 2004; (2):CD003554.
2. Sorensen, LT. Wound Healing and Infection in Surgery: The Pathophysiological Impact of Smoking, Smoking Cessation, and Nicotine Replacement Therapy: A Systematic Review. Ann Surg 2012; 255:1069-1079.
3. Thompson, C. Nutrients and Wound Healing: Still Searching for the Magic Bullet. Nutr Clin Pract 2005; 20:331-347.
4. Stechmiller, JK. Understanding the Role of Nutrition and Wound Healing. Nutr Clin Pract 2010; 25:61-68.