Vice Chair, Surgical Strategic Initiatives for Northwell Health SystemDirector of Surgical Services and Colorectal Surgery at Huntington HospitalProfessor of Surgery at Hofstra University School of Medicine
David E. Rivadeneira, MD, MBA, FACS, FASCRS is Professor of Surgery at Hofstra University School of Medicine, currently serves as the Vice Chair, Surgical Strategic Initiatives for Northwell Health System and
Director of Surgical Services and Colorectal Surgery at Huntington Hospital in Huntington, NY.
Dr. Rivadeneira received his medical degree with honors from Howard University College of Medicine, Washington, DC and an MBA from Adelphi University, Garden City, NY. His residency in surgery was completed at New York Presbyterian Hospital – Cornell Medical Center, Department of Surgery, and Memorial Sloan Kettering Cancer Center in New York, where he served as Chief Resident. In addition, he spent two years as a NIH funded research oncology fellow at Cornell University School of Medicine. Following his residency, he completed a fellowship at the Lahey Clinic Medical Center, Department of Colon and Rectal Surgery in Burlington, MA. Prior to his current appointment, he served as Associate Professor of Surgery at State University at Stony Brook School of Medicine in Stony Brook, NY and as Director of Colorectal Surgery at St. Catherine Hospital in Smithtown, NY.
Recognized as a leader in colon & rectal surgery and for his advanced skills in minimally invasive surgery, Dr. Rivadeneira has a major interest in laparoscopic, and other minimally invasive procedures including advanced robotic procedures for the treatment of colon and rectal diseases, including cancer. He has published extensively with more than 60 peer reviewed articles and 10 book chapters and is editor of a three textbooks on minimally invasive techniques in colorectal surgery.
Rivadeneira_The Chronicles of Incision Management_2017_Volume 1_Issue 1
The cost and clinical implications of surgical site infections (SSIs) represent an enormous burden to today’s health system. As the second most common health associated infection (HAI)–behind only pneumonia— SSIs drive cost to our health system to the tune of $1.3 billion per annum and result in 1 million patient days of hospitalization in those affected.1 Furthermore, decreasing SSIs has been shown to improve outcomes as a result of decreased morbidity and increased patient satisfaction. Finally, it is worth noting that SSIs are increasingly a focus of both hospital systems and providers as there is a continued move to value-based care and compensation using established quality metrics.
Gastrointestinal surgical procedures, particularly those that encompass the colon and rectum have been reported to have a higher incidence of SSIs, reported to be as high as 45%.2, 3 Although many different recommendations and processes have been applied in order to reduce the incidence of SSIs during colon and rectal procedures, such implementation has been difficult and has yielded inconsistent results. In the following manuscript, we will describe the successful systematic implementation of a colon bundle protocol in our health system. We demonstrated a statistically significant decrease in SSIs with the application of a colon bundle protocol in patients undergoing colorectal surgery. The object of this prospective study was to compare rates of SSIs pre- and post-implementation of a dedicated colon surgery bundle in our health system.
Background
Northwell Heath is a large health system composed of 21 hospitals in the New York metropolitan and suburb areas. In 2014, one of our hospitals was found to be an outlier within our health system with a 15% incidence of SSIs post colorectal procedures. We obviously needed to improve on these findings and therefore assembled a multidisciplinary team of leaders that would champion this initiative; they compromised surgeons, anesthesiologists, nurses, infectious disease physicians, and hospital administrators, and gathered best practice guidelines and recommendations for decreasing SSIs post colorectal surgery. As the parameters or elements of the bundle were created, the interdisciplinary team established strategies for the implementation and application of the bundle elements. It was essential to provide directed education to staff and patients and their families, and help developed champions among them to help garner “buy in” from the staff and set up a system for feedback. The team developed a tool to track the compliance and data.
The Colon Bundle
Knowing very well that no one colon bundle could encompass every single element described to decrease SSIs, we concentrated on well-established protocols from the National Surgical Quality Improvement Program, Joint Commission Center for Transforming Health Care, U.S. Department of Health and Human Services, and New York State Partnership for Patients, and tailored a colon bundle that would be best accepted and implemented at our health system.
The bundle we describe includes pre-hospital and pre-, intra- and post operative measures. It should be noted that the data we present comprising the bundle does not exclusively include cases involving a ci-NPWT treatment algorithm. Our institution did not fully move to ciNPWT as part of our colon bundle strategy until 2016.
Pre-Hospital Parameters
The pre-hospital component, which often starts in the surgeon’s office, includes educating the patient and their family that their involvement in this process is extremely important. The patient needs to understand that their participation is paramount in reducing the incidence of SSIs. That is, the patient needs to “buy in” to fact that what they do or don’t do will impact their outcome. This starts with weight reduction in the obese, cessation of smoking, involvement of endocrinologists for glucose management in diabetics with elevated HgbA1c, proper mechanical bowel preparation with a polyethylene glycol solution and oral antibiotics the day before surgery, and washing at home for three days prior with chlorhexidine gluconate wash. On the day of surgery, abdominal wall hair is clipped in the holding area and not in the operating room. Patients are warmed with standard warming measures such as warm air blankets to avoid inadvertent hypothermia before the surgery.
Intra-Operative Parameters
Intra-operative skin preparation with chlorhexidine gluconate with isopropyl alcohol or iodine povacrylex is used when not contraindicated. Maintaining a core temperature above 36 degrees is recommended. Hypothermia is avoided with warm intravenous fluids, warming blankets and mattresses, and warm irrigation. Core body temperature is assessed every 15 minutes during the operation and in the recovery room. Normoglycemia is paramount. Glucose levels are checked just prior to surgery and every two hours during the surgery and maintained <200 mg/dl. An insulin management protocol is instituted if >200 mg/dl. Weight-based appropriate therapeutic levels of intravenous antimicrobial prophylaxis is given within 1 hour of incision and re-dosed when necessary. Optimal tissue oxygenation is monitored and maintained in the operation. Once the surgeon is ready to close the incisions, the entire team re-scrubs, re-gowns and re-gloves, places sterile drapes over the patient and a separate, clean, standardized fascial closure tray is used. The subcutaneous tissue and skin is washed with antibiotic irrigation and skin is stapled closed. A negative pressure wound treatment (NPWT) (PREVENATM Incision Management System) is placed over the incision, or multiple incisions, and is left on for 5-7 days. Most patients are discharged from the hospital before the 5-7 days and continue therapy at home. Negative pressure wound treatment has long been used and has been very effective in expediting open wound healing and closure. The use of closed incisional negative pressure wound therapy (ci-NPWT) has also been shown to improve post-surgical outcomes.
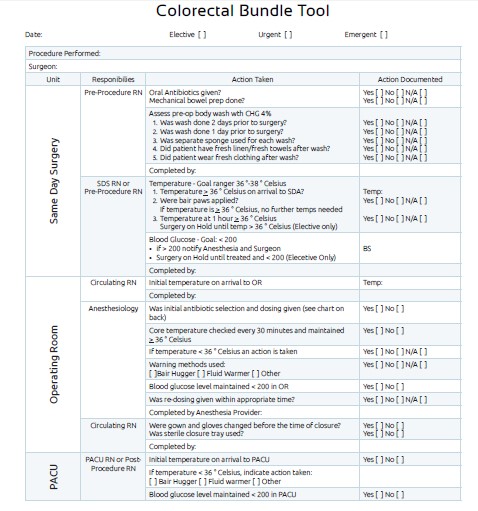
Colorectal Bundle Tool
Post-Operative Parameters
The post-operative management is a continuation of many of the pre-operative and intra-operative parameters, that is maintenance of normothermia, normoglycemia, one dose intravenous antibiotics is given post-operatively then discontinued. The use of ci-NPWT (PREVENATM Incision Management System) is applied to the closed incision for 5-7 days.
Our Results
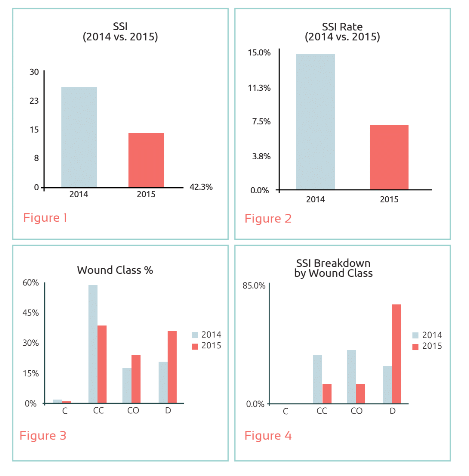
Consecutive patients who underwent a colorectal procedure at one of our hospitals between January 2015 and January 2016 were included in the colon bundle group. SSIs were identified in 11/198 patients (7%) compared to 26/175 (15%), demonstrated in Figures 1. and 2., the year prior to implementation of the colon bundle (which was the impetus for the study). Additionally, we noted a decrease in SSIs occurring in clean-contaminated and contaminated cases, demonstrated in Figures 3. and 4.
We believe that the success of this colon bundle is multifactorial in that the reduction seen in SSIs seen in those patients that underwent the colon bundle protocol benefit from many aspects. It is essential to first understand the magnitude of the problem of SSIs. No institution, no health system, no surgeon nor patient is immune to SSIs. We must all strive for the absolute lowest SSIs possible; we must strive for zero incidences. Is that possible? Maybe not, but we must strive for it. The same was said about central line infections, ventilator-associated pneumonias, and catheter-associated urinary tract infections. Many institutions have seen a zero incidence in these infections for many years. Hospitals and health systems need to be honest and review their data carefully. It is imperative to assemble a multidisciplinary team approach with “buy in” from clinical leaders and champions. These champions will need to educate each of their own separate clinical areas. They will need to demonstrate that the implementation of a colon bundle does lead to significant decreases in SSIs, and that this results in improvement in care. In addition, the patient must also be an active participant in this process. The pre-operative education in regards to weight reduction, cessation of smoking, proper mechanical bowel preparation and skin preparation and normalization of HbA1c are invaluable.
Our use of intraoperative separate closure tray with clean instruments facilitates the closure of the fascia. Extensive antibiotic irrigation of the subcutaneous tissue and skin as well as our use of ci-NPWT with PREVENATM Incision Management System is an important component of our approach to managing colon bundles and decreasing SSIs. The use of ci-NPWT has been reported extensively to reduce SSIs in multiple surgical procedures including colorectal procedures.4-7In summary, the implementation of a colon bundle protocol leads to the significant decrease in SSIs post colorectal surgery, in our experience, a decrease of close to 50%. We believe that a multidisciplinary approach is needed in order to successfully incorporate a colon bundle protocol.
References
1.de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009;37:387–397.
2.Wick EC, Vogel JD, Church JM, Remzi F, Fazio VW. Surgical site infections in a “high outlier” institution: are colorectal surgeons to blame? Dis Colon Rectum. 2009;52:374–379.
3.Anthony T, Murray BW, Sum-Ping JT, et al. Evaluating an evidence-based bundle for preventing surgical site infections: a randomized trial. Arch Surg. 2011:146:263-269.
4.Matatov T, Reddy KN, Doucet LD, Zhao CX, Zhang WW. Experience with a new negative pressure incision management system in prevention of groin wound infection in vascular surgery patients. J Vasc Surg. 2013;57:791–795.
5.Grauhan O, Navasardyan A, Hofmann M, Muller P, Stein J, Hetzer R. Prevention of poststernotomy wound infections in obese patients by negative pressure wound therapy. J Thorac Cardiovasc Surg. 2013;145:1387–1392.
6.Blackham AU, Farrah JP, McCoy TP, Schmidt BS, Shen P. Prevention of surgical site infections in high-risk patients with laparotomy incisions using negative-pressure therapy. Am J Surg. 2013;205:647–654.
7.Bonds AM, Novick TK, Dietert JB, Araghizadeh FY, Olson CH. Incisional Negative Pressure Wound Therapy Significantly Reduces Surgical Site Infection in Open Colorectal Surgery. Dis Colon Rectum 2013; 56: 1403-1408.
8.World Union of Wound Healing Societies (WUWHS) Consensus Document. Closed surgical incision management: understanding the role of NPWT. Wounds International, 2016.