Dr. Allen Gabriel is a member of the American Society of Plastic Surgeons, and in 2001, Dr. Gabriel was chosen by the prestigious Loma Linda University to join the Integrated Plastic Surgery Residency Program. While at Loma Linda University, he volunteered on a medical mission to Ethiopia with Operation Good Samaritan. In addition, he served on several leadership committees and was the chief resident prior to completing his residency. In 2007, Dr. Gabriel was selected by world-renowned plastic surgeon Dr. G. Patrick Maxwell to enter a Breast and Aesthetic Surgery Fellowship in conjunction with Baptist Hospital in Nashville, Tennessee. Completion of this program provided him with advanced training in breast and aesthetic surgery.
Dr. Gabriel was one of the few medical students in the country to have received the prestigious Humanism in Medicine Award. This award lead to the creation of the University of Nevada’s Humanism in Medicine Honor Society, of which Dr. Gabriel is still an active member. During medical school, he was involved with both clinical and basic science research, earning several research awards and publications prior to graduating. Dr. Gabriel is board certified in plastic surgery and has been invited to speak nationally and internationally on breast and aesthetic surgery.
Gabriel_The Chronicles of Incision Management_2017_Volume 1_Issue 1
Allen Gabriel MD, FACS1;
Steven R. Sigalove, MD, FACS2; G. Patrick Maxwell, MD31PeaceHealth Medical Group, Vancouver, WA 2DuPage Medical Group, Glen Ellyn, IL3Department of Plastic Surgery, Loma Linda University Medical Center, Loma Linda, CA
Previously published:
Gabriel A, Sigalove SR, Maxwell GP. Initial experience using closed incision negative pressure therapy after immediate postmastectomy breast reconstruction. Plast Reconstr Surg Glob Open. 2016;4(7):e819. Doi:10.1097/GOX.0000000000000803
Introduction
Immediate postmastectomy reconstruction as part of 2-stage expander/implant breast reconstruction provides better aesthetic outcomes1 and psychological benefits for patients2 but is associated with high complication rates. Seroma formation, infection, dehiscence, and tissue necrosis are possible problems after immediate reconstruction.
Favorable results have been reported using the PREVENA™ Incision Management System over various incision types.5 We investigated outcomes of applying the PREVENA™ Incision Management System with a customizable dressing over closed incisions on 13 patients (25 breasts) who received immediate postmastectomy reconstruction.
Technique
Thirteen patients (mean age 44.8 years ± 9.7 years; mean body mass index; 29.2 ± 7.2 kg/m2, 25 breasts) received immediate postmastectomy breast reconstruction as part of 2-stage expander/implant breast reconstruction. Four patients had comorbidities, obesity (n=3), diabetes (n=1), and preoperative chemotherapy (n=2). Nipple-sparing (n=14), reduction-pattern (n=6), or skin-sparing (n=5) mastectomies were performed based on each patient’s oncological and reconstructive treatment goals. All postmastectomy incisions were closed using absorbable sutures, and managed with the PREVENA™ CUSTOMIZABLE™ Dressing − 90cm and PREVENA™ 125 Therapy Unit applied in the sterile field of the operating room. Both the customizable dressing and therapy unit were designed for placement up to 7 days. Surgical drains were used and were routed under the skin beyond the PREVENA™ CUSTOMIZABLE™ Dressing and functioned independently of the PREVENA™ Incision Management System. Although, previous concern about removing drains during therapy led to early PREVENA™ Therapy discontinuation, we have since become comfortable removing drains during PREVENA™ System use. After treatment, the dressings were carefully removed and a skin adhesive closure (Steri-Strip™ Skin Closure, 3M™, St. Paul, MN) was applied over each incision.
Overall mean PREVENA™ System duration was 4.3 days (range, 3-5). Mean drain placement was 8.2 days (range, 6-12) compared to our estimate of 12-14 days of drain placement (based on personal experience before PREVENA™ System availability). By the 3-month follow-up, 96% (24/25 breasts) achieved healing and remained closed. Superficial dehiscence occurred on 3 breasts (12%). These patients were obese with other risk factors (e.g., diabetes mellitus, preoperative chemotherapy, axillary dissection). All superficial dehiscences resolved without surgical closure. Flap necrosis occurred on 1 breast (4%) in the reduction-pattern group, in a morbidly obese patient with type 2 diabetes which required surgical revision. A delayed hematoma developed on postoperative day 13 in 1 breast in nipple-sparing group, which resolved.
Representative Case
A 27-year-old female with history of obesity, preoperative chemotherapy, and left breast axillary dissection (Figure 1A) underwent reduction-pattern mastectomy on both breasts. After immediate breast reconstruction, PREVENA™ Incision Management System with PREVENA™ CUSTOMIZABLE™ Dressing was applied over the entire incision (Figure 1B). Superficial dehiscence in the left breast resolved with local wound care. Both incisions were intact at 4 weeks and remained intact at 2 months post mastectomy. The patient underwent breast reconstruction with good results at 12 months post reconstructive surgery (Figure 1C).
Benefits of PREVENA™ Incision Management System
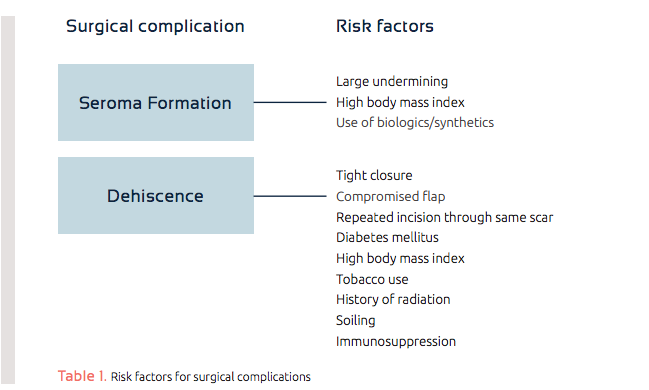
Based on published literature and/or personal experience, we identified risk factors associated with seroma formation, dehiscence, and delayed healing (Table 1). Patients with 1 or more factors received treatment with the PREVENA™ Incision Management System to facilitate management of their incisions.
We applied PREVENA™ Incision Management System with a PREVENA™ CUSTOMIZABLE™ Dressing to the entire incision immediately post breast reconstruction in order to draw wound edges together, protect the incision from contamination, and help remove fluid. We speculated that the negative pressure delivered by the PREVENA™ 125 Therapy Unit might reduce dead space. In a study of wounds with dead-space created on the backs of pigs, PREVENA™ Therapy-treated incisions had significantly reduced drainage compared to gauze-treated incisions.6 Two comparative clinical studies of postoperative hip incisions reported reduced seroma development7and volume,8 respectively, in ciNPT-treated incisions. Larger studies are needed to research implications for breast reconstruction.
Based on initial experience, PREVENA™ Incision Management System with PREVENA™ CUSTOMIZABLE™ Dressings could be a viable option over closed incisions following immediate postmastectomy reconstruction as part of 2-stage expander/implant breast reconstruction.
References
1.Kroll SS, Coffey JA, Jr., Winn RJ, et al. A comparison of factors affecting aesthetic outcomes of TRAM flap breast reconstructions. Plast Reconstr Surg. 1995;96:860-864.
2.Miller MJ, Rock CS, Robb GL. Aesthetic breast reconstruction using a combination of free transverse rectus abdominis musculocutaneous flaps and breast implants. Ann Plast Surg. 1996;37:258-264.
3.Sullivan SR, Fletcher DR, Isom CD, et al. True incidence of all complications following immediate and delayed breast reconstruction. Plast Reconstr Surg. 2008;122:19-28.
4.Alderman AK, Wilkins EG, Kim HM, et al. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2002;109:2265-2274.
5.Semsarzadeh NN, Tadisina KK, Maddox J, et al. Closed Incision Negative-Pressure Therapy Is Associated with Decreased Surgical-Site Infections: A Meta-Analysis. Plast Reconstr Surg. 2015;136:592-602.
6.Suh H, Lee A-Y, Park EJ, Hong JP. Negative Pressure Wound Therapy on Closed Surgical Wounds With Dead Space: Animal Study Using a Swine Model. Annals of Plastic Surgery. 2016;76(6):717-722.
7.Pachowsky M, Gusinde J, Klein A, et al. Negative pressure wound therapy to prevent seromas and treat surgical incisions after total hip arthroplasty. Int Orthop. 2012;36:719-722.
8.Pauser J, Nordmeyer M, Biber R, et al. Incisional negative pressure wound therapy after hemiarthroplasty for femoral neck fractures – reduction of wound complications. Int Wound J. 2014:Aug 14; Epub ahead of print.