VP, Managed Care, MCO National AccountsKC
Chouteau_Discharge Planning and Transitional Care_2018_Volume 1_Issue 1
KCI, an Acelity company, is a global health care company headquartered in San Antonio, TX. With a focus on wound care and patient healing, KCI provides a number of products to the marketplace designed to advance the practice of wound care while delivering significant patient support and system-wide economic benefit. This article highlights the drivers of costs in wound care, the processes associated with insurance authorization for patients transitioning from an acute hospital stay to a post-acute healing environment, and the importance of the patient experience across the continuum of care as it relates to the use of Negative Pressure Wound Therapy (NPWT) in the post-acute setting.
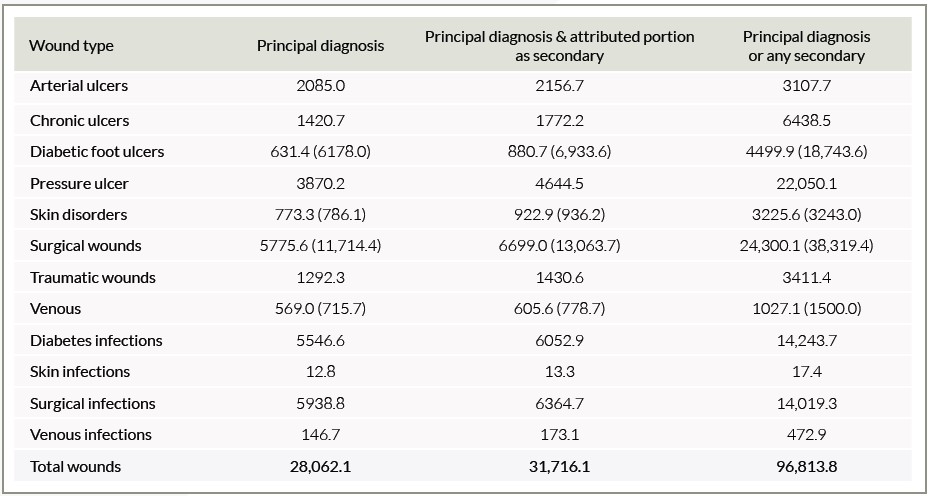
Healthcare in the U.S. market consumes over $3 trillion in spending every year. A recent report suggests that nearly 15% of Medicare beneficiaries (8.2 million) had at least one type of wound or infection (not pneumonia).1Surgical infections were the largest prevalence category (4.0%), followed by diabetic infections (3.4%).1 Total Medicare spending estimates for all wound types ranged from $28.1 to $96.8 billion.1 (See Table 1)
With such a significant outlay associated with this segment of medicine, it comes as no surprise that spending in relation to wound healing is carefully managed by both governmental and commercial payors. It is difficult to determine what portion of the payment is attributable to each of the patient’s conditions and whether the wound was the primary diagnosis or the secondary diagnosis. For example, a wound associated with the underlying comorbidity of diabetes would incur costs associated with the patient’s care for diabetes as well as any ancillary costs associated with complicating factors of the primary diagnosis, such as diabetic foot ulcers.1 There is a multitude of reasons for this high cost including a lack of standardization in the practice of wound care, environmental
conditions that can limit or promote healing at home, and the co-morbid complexity of most wound care patients in general.
As we address the costs associated with wound care, it is important to note that the term is widely used to describe a wide range of products, points of care, and provider types. Everything from bandages to hyperbarics, and anywhere from intensive care units (ICUs) to the patient’s living room can be associated with wound care spending. Yet we often find ourselves unable to identify the costs of healing for any given patient across diverse care settings and product classes utilized. The result is a disjointed view of the economic impact on the “system” for any single patient experience, which often leads to a lack of investment in wound care best practices, product selection, and patient awareness.
While there are a number of cost savings or avoidance strategies that the healthcare system cannot yet track, there is one clear measure: readmission. When a patient’s post-acute healing cycle results in sub-optimal outcomes, they are likely to end up being readmitted into the hospital. It is the goal of both treating providers and payors alike to reduce the costs associated with avoidable spending, and like it or not, dollars spent within the hospital setting are easy to identify.
What does it take to minimize the chances of unnecessary spending and costs to hospitals for wound care patients? Or, phrased somewhat differently, are there effective risk mitigation strategies that produce positive, sustainable, repeatable, and scalable results for a unique, often high-risk, patient cohort? As demographics continue to shift, this is a question now being posed by both health systems and insurance companies alike.
The fact that the shared interests of the stakeholders in this discussion overlap may be a surprise to many who view the insurance–provider relationship as fundamentally adversarial. However, now more than ever, as our health care system is evolving and financial risk is being assumed by more and more providers, patient outcomes are becoming the prevailing metrics that drive profitability for both parties, rather than tit-for-tat practices that balance quantity billing and aggressive denials.
Similar to many hospital-based practices and protocols, insurance companies employ probability-based logic in how they design authorization protocols. Although imperfect at times for both parties, the underlying methods, when implemented and appropriately deployed, yield desired results at the population level. For many insurance companies, clinical judgment is employed to span the gap between population-level wound care protocols and the needs of specific patients. This may include assigning a separate case manager for patients with complex care needs, enrolling patients in disease management programs, implementing care coordination services, developing care plans, and in some cases, interpreting health plan policy in a patient-specific manner based on wound-type, etiology, and healing conditions.Generally speaking, the goal of a health plan authorization team is to ensure that wound care patients have access to the right products and the right providers in the right setting at the right time. For most payors, the information needed to drive this decision process is supplied by a discharging hospital, and then correlated, entered, and evaluated by a manufacturer before being submitted to a health insurance company.
Just like hospitals and physician offices, KCI files insurance paperwork as a courtesy to patients, and just like hospitals and physician offices, KCI recognizes the patient as having the ultimate fiduciary responsibility for paying medical bills. Given the length of time KCI has been providing NPWT to the marketplace, many health plans have adopted components of KCI’s internal evaluation process in the design of their own authorization protocols. Typically, these components are combined with written policy guidance from groups like Milliman, InterQual, and C.M.S. to form the backbone of their NPWT policy. It is the goal of KCI to be as thorough as necessary in obtaining the medical information required by a patient’s insurance company. The more complete the authorization request, the more effectively we can act to protect the patient from balance-billing associated with non-coverage.
When a manufacturer is less diligent in obtaining information required by insurance, they can be seen as being more accommodating to a requesting hospital. However, the manufacturer is often transferring the risk of insurance non-payment directly to the patient. The less information collected, the higher the chance that the insurance company will not authorize the use of the requested product and the patient will receive a bill. While it may be more straightforward from a paperwork perspective to simply send a patient a bill, practices such as these may result in patients not receiving necessary care, thereby creating less than ideal clinical outcomes in the post-acute environment and landing the patient right back in the hospital.
In order to offer patients the most financial protection possible, KCI employs over 800 professionals at our San Antonio campus that are dedicated solely to the order, review, authorization and payor billing processes. The services provided represent investments made by KCI on a daily basis to assist our patients and their insurance companies in ensuring that V.A.C.® Therapy continues to be available to patients in need.
For our acute hospital partners, KCI continues to invest in the resources necessary to make it easier to address the needs of both hospital discharge planners and payor authorization teams. The overlap in interest is that both hospitals and payors want to see patients seamlessly transition from hospital to home quickly and efficiently once the decision to discharge has been made. To this end, KCI maintains a staff of professionals across the country who are focused solely on assisting in the patient discharge and the transition process.
KCI’s position as the leading marketplace partner to thousands of hospitals, providers, and payors for NPWT demands that we continue to evolve at a rapid pace. As we have grown in this regard, our focus on patient experience has emerged as a leading driver of optimal outcomes, benefitting all stakeholders.
Patient experience encompasses many aspects of care including service, education, coordination, ease of use, engagement, and providing compassionate resources. While each of our patients may experience wound healing in an individual manner, all can benefit from an improved experience. Investment areas for KCI include additional personnel who are dedicated to easing and expediting the transition process for both patients and their family members. An additional investment area for KCI includes the development of technological capabilities that enable us to better meet existing gaps in post-acute wound care delivery. By developing patient-facing digital health platforms in conjunction with NPWT devices that provide remote therapy monitoring in the home setting, these capabilities extend KCI resources and expertise wherever they are needed.
A focus on patient experience also demands that we provide solutions at a “patient ecosystem level,” wherein we act to positively impact, not only patients, but also others who play a role in forming the totality of the patient experience across the continuum. An example of this has been the creation and deployment of the KCI iON HEALING™ smart phone application for use in both the acute and post-acute arenas. Through iON HEALING™ Mobile App, V.A.C.® Therapy orders can be placed, supply levels maintained, and telephone consultations conducted, all from the palm of a clinician’s hand.
The investment in these efforts, and many more, represent the responsibility KCI feels towards patients, providers, and payors as we all work together to improve our healthcare system. For any questions or additional comments, please visit KCI’s website at www.acelity.com, or call our customer support line 24 hours a day, seven days a week at (800) 275-4524.
References
Nussbaum SR, Carter MJ, Fife CE, et al. An Economic Evaluation of the Impact, Cost, and Medicare Policy Implications of Chronic Nonhealing Wounds. Value in Health. 2018;21(1):27-32. doi:10.1016/j.jval.2017.07.007.