Dr. Rachael Williams is a board certified general surgeon who is an Associate Medical Director with the Grossman Burn Center. She received her medical degree from Boston University School of Medicine and attended the Johns Hopkins Bloomberg School of Public health. She completed her general surgery residency at Eastern Virginia Medical School followed by burn and surgical critical care fellowships at Emory University and Grady Memorial Hospital. During her postgraduate training years she won three best oral presentation awards at annual meetings of the Southern Regional Burn Conference. She has published in the Journal of the American College of Surgeons, the Journal of Burn Care and Research, and the American Surgeon. Dr. Williams is a consultant for 3M.
Williams_Current Dialogues in Wound Management_2020_Article_16
Introduction
Morel-Lavallée lesions are rare post-traumatic internal de-gloving injuries first described by Dr. Maurice Morel-Lavallée in 1853. They most commonly occur in obese patients after blunt trauma in the lower extremity along the greater trochanter or proximal thigh.1 Frequently, there is a delay in diagnosis leading to chronic lesions, necrosis, and resultant wound infections.2 These features lend clinical challenges to the management and closure of these wounds. Here, we describe a case of a full-thickness burn and chronic Morel-Lavallée lesion with Pseudomonas aeruginosa infection successfully managed with V.A.C. VERAFLO™ Therapy and the VERAFLO CLEANSE CHOICE™ Dressing, systemic antibiotics, and debridement. This case report highlights the use of V.A.C. VERAFLO™ Therapy to cleanse the wound bed allowing for prompt closure of a large wound.
Case Report
A 22-year-old female sustained a 3% total body surface area full-thickness burn and Morel-Lavallée injury to the right thigh after contact with a hot car muffler and blunt trauma. Her past medical history was notable for tetrahydrocannabinol use and morbid obesity with a body-mass index of 40 kg/m2. She was pinned between two cars with the hot muffler in direct contact with her right lower extremity. The patient was initially treated at an outside hospital where imaging demonstrated no acute fracture in the right lower extremity. She presented to our outpatient clinic 1 month after her injury with an eschar concerning for a full-thickness burn of her right lower extremity and cellulitis (Figure 1).

Repeat radiographic imaging of her injury demonstrated subcutaneous soft tissue swelling and she was admitted to the hospital to perform an excision of the full-thickness burn. During the procedure, it was noted that the patient had a large hematoma and necrotic fat consistent with a chronic Morel-Lavallée lesion. The hematoma was evacuated, and the necrotic fat was widely excised leaving a defect that measured 30 x 20 x 5-cm3 (Figure 2).

The intraoperative wound cultures were positive for Pseudomonas aeruginosa. In addition to serial surgical debridement, and intravenous antibiotic therapy, the decision was made to use V.A.C. VERAFLO™ Therapy with the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing to assist in the management and cleansing of the wound (Figures 3 and 4).


V.A.C. VERAFLO™ Therapy was initiated with 25 cc of 0.25% strength Dakin’s solution with 10 minutes of dwell time, followed by 3.5 hours of negative pressure wound therapy at -125 mmHg. Dressings were changed every 3 days and closure of the wound using a split-thickness autograft was achieved once healthy granulation tissue was observed in the wound bed (Figure 5).
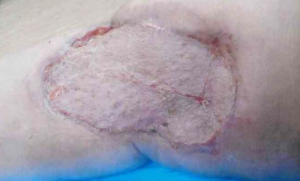
The graft has good color match with the surrounding skin and the patient has full range of motion of her right lower extremity and no hypertrophic scarring three months post-surgery.
Discussion
Overall, Morel-Lavallée lesions are rare, but surgeons should maintain a high index of suspicion for chronic Morel-Lavallée when obese patients present with a history of blunt trauma and full-thickness burns are present even in the absence of long bone fractures. Despite the patient’s delay in presentation and resultant P. aeruginosa infection, successful closure was achieved with the use of intravenous antibiotics, V.A.C. VERAFLO™ Therapy with V.A.C. VERAFLO CLEANSE CHOICE™ Dressing and split-thickness autografting. The overall time to closure of the wound was 3 weeks and no dermal substitutes were required prior to autograft placement. Overall, the patient had optimal cosmetic and functional outcomes.
Patient data and photos courtesy of Rachael Williams, MD.
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
NOTE: Specific indications, contraindications, warnings, precautions and safety information may exist for these products. Please consult a healthcare provider and product instructions for use prior to application. Rx only.
References
- Bomela LN, Basson H, Motsitsi NS. Morel-Lavallee lesion: A review. SA Orthopaedic Journal 2008;7(2):34-41.
- Kim CH, Choi WY, Son KM, Cheon JS. Surgical treatment of a delayed diagnosed Morel-Lavallee lesion: A case report. J Wound Manag Res 2017;13(2):62-64.
© 2020 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. PRA-PM-US-02615 (07/20).

