
Dr. Jayesh Shah is the President of South Texas Wound Associates, PA, San Antonio, Texas, where he provides clinical wound care services in San Antonio and the surrounding communities. He is also the President of TIMEO2 Healing Concepts, LLC, in San Antonio, Texas, which provides consulting and education services in wound care and hyperbaric medicine both nationally and internationally. His degrees include an MBBS from M. S. University, India, and an MD in Internal Medicine from St. Luke’s Roosevelt Hospital, Columbia University, New York. He is board certified in internal medicine, undersea and hyperbaric medicine, certified in wound management, hyperbaric medicine, past chair of the American College of Clinical Wound Specialists and past vice president of the American College of Hyperbaric Medicine. He has been the recipient of the enterpreuner of the year award by the Alamo Asia Chamber of Commerce (2016); the Paul James Sheffield Education Award for Lifetime Dedication to Education in the field of Undersea and Hyperbaric Medicine (2014); the Jefferson C. Davis Memorial Award for Excellence in Clinical Hyperbaric Medicine (2007 and 2011); the Carolyn Sue Award (2009); the Young Scientist/Medical Doctor Award (2008); the Community Service and Leadership Award by Alamo Asian American Chamber of Commerce (2008). He has published 3 books: Wound Care Certification Study Guide in 2011 with its second edition in 2016, and Textbook of Clinical Wound Medicine: A Evidence Based Approach in 2017. He has authored over 40 chapters on various wound topics in 4 books in addition to 30+ scientific articles on wound care and hyperbaric medicine. As an assistant editor of the Journal of the American College of Clinical Wound Specialists, he regularly writes a column on certification exam in wound care.
Shah_Current Dialogues in Wound Management_2018_Volume 4_Issue 4
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
INTRODUCTION
Chronic pressure injuries (PIs) continue to be a significant healthcare problem throughout the world.1,2 They are common in elderly patients and individuals with a spinal cord injury.3Contributing factors for the development of PIs are both intrinsic and extrinsic. Examples of intrinsic factors are the co-morbidities of a patient such as congestive heart failure, end-stage renal disease on dialysis, hypotension, chronic obstructive pulmonary disease, limited mobility due to arthritis, patient’s age, patient’s functional status, incontinence, and nutritional status. Examples of extrinsic factors are friction, sheer, moisture, and pressure.3 After a patient develops a stage 4 PI, it is hard to manage in an outpatient facility because it requires a lot of coordination of care. Most patients with stage 4 PIs are treated in various settings. This article will illustrate the challenges and benefits of each setting in treating a chronic PI.
 Figure 1. Unstageable PI at presentation. Wound size was 7 cm x 9 cm x 3.5 cm with 100% necrotic tissue.
Figure 1. Unstageable PI at presentation. Wound size was 7 cm x 9 cm x 3.5 cm with 100% necrotic tissue.
CHALLENGES IN MANAGING PI PATIENT IN VARIOUS SETTINGS AND NEED FOR A CONTINUUM OF CARE
CASE STUDY
A 48-year-old female with a spinal cord injury subsequent to a motor vehicle accident developed quadriplegia C1-C4 a year ago. The patient had a history of incontinence, refused a colostomy, and was on a foley catheter for urinary incontinence. The patient developed a PI in the hospital while receiving treatment for her spinal cord injury and was completely bedbound and dependent on the nursing staff and family for all activities of daily living except that she was able to eat on her own. The patient’s nutrition assessment showed mild-to-moderate malnutrition with an albumin count of 3.1 g/dL and prealbumin of 19 g/dL. The patient was first seen at a wound healing center after referral from home health. Upon presentation, she had a sacral PI of 7 cm x 9 cm x 3.5 cm with 100% necrotic tissue (Figure 1). She was admitted to hospital with intravenous antibiotics and underwent surgical debridement. The patient was discharged home after 21 days in the hospital with oral antibiotics as her magnetic resonance imaging (MRI) and pathology reports were negative for osteomyelitis. The patient did not qualify for acute long-term care (LTC) or skilled nursing facility care due to her insurance status. The patient was sent home with a plan for 40 days of negative pressure wound therapy using the ACTIV.A.C.™ Therapy System.
 Figure 2. Wound after 47 days of negative pressure therapy. Wound size was 4.6 cm x 6 cm x 1.1 cm and covered 70% with healthy granulation tissue.
Figure 2. Wound after 47 days of negative pressure therapy. Wound size was 4.6 cm x 6 cm x 1.1 cm and covered 70% with healthy granulation tissue.
After using the ACTIV.A.C.™ System, (47 dayspost-presentation), the patient’s PI had improved with 70% of the wound covered with healthy granulation tissue (Figure 2) and the ACTIV.A.C.™ System was discontinued. The patient was started on 0.125% Dakin’s solution.
At the second follow-up visit (77 days post-presentation), the patient’s air mattress was not working, and her wound worsened increasing in size (3.7 cm x 4.9 cm x 1.4 cm), displaying increasing necrotic tissue and purulent drainage. The wound required another surgical debridement (Figure 3). The patient was continued on the ACTIV.A.C.™ System for 1 week after which she was referred to plastic surgery for myocutaneous flap closure. The patient was given antibiotics while in the hospital and was then discharged back home but continued having problems with the air mattress and the off-loading device.
 Figure 3. Wound 77 days post-presentation. Wound regressed and showed signs of infection after offloading device failed. Wound size was 3.5 cm x 4.9 cm x 1.4 cm with increasing necrotic tissue and purulent drainage.
Figure 3. Wound 77 days post-presentation. Wound regressed and showed signs of infection after offloading device failed. Wound size was 3.5 cm x 4.9 cm x 1.4 cm with increasing necrotic tissue and purulent drainage.
Ten days following surgical closure, the patient presented with flap failure and infection (Figure 4). The patient was then readmitted to the hospital for partial closure and debridement 1 day after readmission (Figure 5). The decision was made to heal the wound by secondary intention as the patient was unable to turn independently on her own. The patient was continued on the ACTIV.A.C.™ System for 3 weeks (Figure 6). Once the re-epithelialization was observed, the ACTIV.A.C.™ System was discontinued (Figure 7). Treatment was switched to silver alginate dressings for 3 weeks. The wound was completely healed 209 days after initial presentation (Figure 8).
This case study delineates that patients with a stage 4 PI with limited mobility need multidisciplinary care in the right setting including incontinence care, nutrition assessment, and off-loading. A home setting for this patient would not be adequate or appropriate as this setting would increase the overall time to heal the wound. If such patients receive approval to stay in an acute LTC facility, then it may significantly decrease the healing time. With the present focus on cost containment, most insurance carriers try to send such patients to a low-cost setting instead of the right setting for care. There are some advantages and challenges with each care setting for treating patients with a chronic PI, a few of which are discussed below.
 Figure 4. Wound 10 days after surgical closure. Wound showed flap failure and infection. Wound size was 5.5 cm x 8 cm x 3.5 cm.
Figure 4. Wound 10 days after surgical closure. Wound showed flap failure and infection. Wound size was 5.5 cm x 8 cm x 3.5 cm.
ADVANTAGES AND CHALLENGES FOR TREATING CHRONIC PIs IN VARIOUS CARE SETTINGS
1.Outpatient wound clinic with home health in a home setting
Advantages
1.The patient can be seen and treated by a skilled multidisciplinary team.
2.It provides an opportunity for bedside debridement.
3.The patient can be treated with negative pressure therapy with the help of home health.
4.The outpatient clinic can coordinate care with home health for ongoing care.
5.IV antibiotics can be arranged at home if needed, but there is usually a delay due to time taken for insurance approval.
 Figure 5. Wound following surgical debridement and partial closure (1 day after readmission). Wound size was 2.5 cm x 3 cm x 1.5 cm.
Figure 5. Wound following surgical debridement and partial closure (1 day after readmission). Wound size was 2.5 cm x 3 cm x 1.5 cm.
Challenges
1.It is difficult to provide and supervise adequate off-loading.
2.Current insurance guidelines do not allow for the most appropriate off-loading bed at home.
3.Nutrition management is challenging.
4.Taking care of an incontinent patient can be challenging as it requires around-the-clock attention.
5.Transportation can be an issue when the patient has to be brought to the wound clinic as ambulance transportation may not be approved by the insurance carrier, and if a patient is transported in a wheelchair, it can lead to worsening of the PI.
6.Limited psychosocial services are available.
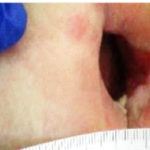 Figure 6. Wound 21 days after partial closure. Wound size was 2 cm x 3.5 cm x 1.5 cm. ACTIV.A.C.™ System was reinitiated for 3 weeks.
Figure 6. Wound 21 days after partial closure. Wound size was 2 cm x 3.5 cm x 1.5 cm. ACTIV.A.C.™ System was reinitiated for 3 weeks.
2. Hospital
Advantages
1.Patients can be seen and treated by a multidisciplinary team.
2.Patients can be treated with negative pressure therapy and with advanced wound dressings.
3.Patients can be treated with IV antibiotics.
4.Off-loading beds are available.
5.Nutrition management can be handled adequately.
6.Incontinence care can be handled adequately.
7.Expert consultations from various specialties can be obtained immediately.
8.Psychosocial services are available.
Challenges
1.Hospitals have a limited length of stay.
2.Thirty-day readmissions may give a bad “quality” score to the hospital.
3.Discharge planning in the right setting may be limited to what is approved by insurance.
 Figure 7. Wound size was 0.2 cm x 0.4 cm x 0.3 cm. ACTIV.A.C.™ System was discontinued and treatment switched to silver alginate dressings.
Figure 7. Wound size was 0.2 cm x 0.4 cm x 0.3 cm. ACTIV.A.C.™ System was discontinued and treatment switched to silver alginate dressings.
3. Acute long-term care home (LTCH)
LTCHs are unique because patients are admitted based on length of stay rather than diagnosis or intensity of care. On average, the length of stay for patients admitted to an LTCH is more than 25 days. The types of patients treated in an LTCH are usually medically complex requiring ongoing nursing, extensive rehabilitation, and medical therapies that cannot be delivered in an outpatient setting.
Advantages
1.Patients can be seen and treated by a multidisciplinary team.
2.Patients can be treated with negative pressure therapy and with advanced wound dressings.
3.Patients can be treated with IV antibiotics.
4.Off-loading beds are available.
5.Nutrition management can be handled adequately.
6.Incontinence care can be handled adequately.
7.Expert consultations from various specialties may be available.
8.Psychosocial services are available.
Challenges
1.Given the stringent admission criteria, some patients may not qualify to be discharged in this setting.
2.Many insurances feel that similar care can be given in a skilled nursing facility (SNF) so they do not approve discharge to an acute LTC facility.
3.For surgical debridement or flaps, patients have to be readmitted to the hospital.
4.There may be limited availability of specialists/consultants.
4. Skilled Nursing Facility (SNF)
Patients who are discharged to an SNF have lower acuity needs compared with those discharged to an LTCH; however, patients require a skilled level of care for their co-morbidities, rehabilitation, complex wound management, and psychosocial services. Nursing homes have become skilled providers of wound care and are engaged in an advanced level of care.5 Many nursing homes are certified as skilled nursing facilities and have access to a skilled wound care team that can help with complex wound patients.
Advantages
1.Patients can be seen and treated by a multidisciplinary team.
2.Patients can be treated with negative pressure therapy and advanced wound dressings.
3.Patients can be treated with IV antibiotics.
4.Off-loading beds are available.
5.Nutrition management can be handled adequately.
6.Incontinence care can be handled adequately.
7.Psychosocial services are available.
 Figure 8. Wound fully healed 209 days post initial presentation.
Figure 8. Wound fully healed 209 days post initial presentation.
Challenges
1.For surgical debridement or flaps, patients have to be readmitted to the hospital.
2.Expert consultations from various specialties may not be available, and the patient will have to be transported for those appointments.
3.Nurse-to-patient ratio is high making it difficult to provide care for complex wound problems in certain SNFs.
CONCLUSION
Many chronic PI patients suffer from multiple co-morbidities, which is enough to impede wound healing. Some of the factors that impede wound healing are modifiable while some are not. The modifiable chronic conditions are usually complicated by the patient’s psychological, social, financial, or familial circumstances. For example, the patient in this case study would have benefited from acute long-term care or a skilled nursing facility, if acute LTC was not possible. Access to an LTCH and an SNF can be an important tool for the treatment of a complicated PI. A wound care team that practices at all levels of the continuum of care in settings such as a hospital, acute LTC, SNF, wound centers, and home settings can provide much needed continuity of care with better outcomes.
References
1.Reddy M, Gill SS, Rochon PA. Preventing pressure ulcers: a systemic review. JAMA. 2006:296(8):974-984.
2.Lyder CH. Pressure ulcer prevention and management. JAMA. 2003;289(2):223-226.
3.Garcia A. Pressure ulcers. In: Shah JB, Sheffield PJ, Fife CE, eds. Textbook of Chronic Wound Care. 1st ed. North Palm Beach, FL: Best Publishing; 2018:295-314.
4.Johnson D, Wise J, Zendehrouch P. Wound care in the Acute Long-Term Care Hospital. In: Shah JB, Sheffield PJ, Fife CE, eds. Textbook of Chronic Wound Care. 1st ed. North Palm Beach, FL: Best Publishing; 2018:583-592.
5.Ramsey C. Wound care in the Nursing Home Setting. In: Shah JB, Sheffield PJ, Fife CE, eds. Textbook of Chronic Wound Care. 1st ed. North Palm Beach, FL: Best Publishing; 2018:593-605.

