
Kara Couch is a family nurse practitioner and Certified Wound Specialist, who has been working in wound care for the past 12 years. As a nurse scientist, she is an investigator on several clinical trials related to wound healing. Kara also serves as a member of the Guidelines Committee for the Association for the Advancement of Wound Care and has authored or co-authored numerous articles and chapters on wound healing. She also lectures nationally on wound care and wound healing topics.
Couch_Current Dialogues in Wound Management_2016_Volume 2_Issue 1
The wars in Iraq and Afghanistan lasted from 2001-2014. Hundreds of thousands of service men and women were deployed in these efforts. Unfortunately, thousands of troops were also injured in the line of duty. Between 2001-2015, there were 1,645 amputees and over 5,200 troops total with physical injuries.1The surge in the final years of the Afghanistan War was particularly violent, with many troops sustaining multiple amputations as well as many other grievous wounds. They required immediate, coordinated and comprehensive care that began on the battlefield, and often their recovery took years at a specialized facility before they were able to return home. Over 75% of the combat injuries were caused by a blast mechanism. Usually in Afghanistan, this was an improvised explosive device (IED) or unknown landmine left from the earlier wars in the 1980s between Afghanistan and the Soviet Union.
IN THEATER- LEVELS I-III
At the moment of injury, troops were treated by medics in the field (Level 1) and then at various levels of care within the military system. Within the first hour of injury, they were then transferred to a Forward Surgical Team (FST), which was embedded close to where the battles occurred. The FST was Level II. There the patients had their initial trauma assessment, damage control resuscitation and stabilization. Within 12-24 hours of arriving at the FST, they were then transferred by Tactical Medevac to the Level III area of care. The Level III was a larger hospital compound within the country known as a Combat Support Hospital. The CSH that was the epicenter for Afghanistan was in Bagram Air Field where NATO and a multi-national group of troops resided (American and British primarily). The patient was again assessed and stabilized at the CSH before being transferred out of theater (the war zone) to Germany and Landstuhl Regional Medical Center (LRMC). Landstuhl is the Level IV center.
Typical times between the moment of injury to arriving at Landstuhl were 24-72 hours. Along the way, the patients had at least one surgical procedure to clean their wounds, if not more, and had been stabilized by the extraordinary efforts in the field. As a point of comparison, troops injured in World War II had a 70.7% chance of survivability. Troops in the Korean War had a 78.2%, while Vietnam had a 76% chance of survivability. Troops injured in Iraq and Afghanistan had a >90% survivability, (see Figure 1) which is remarkable given the extent of their injuries.
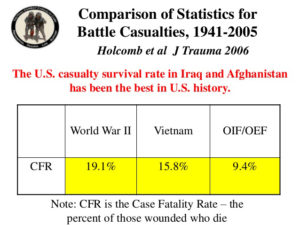 Figure 1. Comparison of Statistics for Battle Casualties, 1941-2005
Figure 1. Comparison of Statistics for Battle Casualties, 1941-2005
Many inner cities have a higher rate of mortality than the military trauma system, and those valuable lessons have been taught here in the United States. An example of where those lessons were invaluable was in the Boston Marathon bombing in 2013. One would hope that that was an isolated incident, but given the current state of our global affairs, it is unlikely.
GERMANY- LEVEL IV
The true multidisciplinary team approach springs into action once the patients arrive in Germany. The goal is again to assess, treat, stabilize and transfer home to the final level of care (V) in the US. There are three major Centers of Excellence where troops are transferred for care: Walter Reed National Military Medical Center (WRNNMC) in Bethesda, MD; San Antonio Military Medical Center in San Antonio TX; and Naval Medical Center San Diego in CA. Troops were transferred to be close to their units and their families, as well as based on their injury patterns. The burn center is located in Texas, so those patients were usually sent there, for example.
Patients arrived in the US for care anywhere from 48 hours post injury to 1 week. There are a series of weekly coordinated video-teleconferences (VTC) between Levels III-V which update each team as to the status of the patients and where they were likely to transfer based on needs and facility status. Such an effort is critical, but also remarkable given then time differences involved. Afghanistan is 9 hours ahead of the East Coast of the US, and California is 3 hours behind, so it is striking that all centers were online simultaneously. Medevacs from Germany arrived in the US at least 3 days a week with Andrews Air Base in Maryland as the destination and point of transfer. At times, patients would stay briefly at WRNNMC before leaving for Texas or CA as a final destination (see Figure 2).
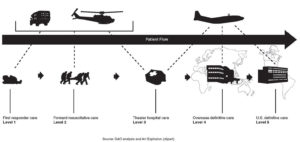 Figure 2. Schematic of patient flow from first responder care to U.S. definitive care
Figure 2. Schematic of patient flow from first responder care to U.S. definitive care
STATESIDE- LEVEL V
Once the patients arrived at WRNNMC, they were taken onto the trauma service and had a complete head to toe assessment by multiple teams (trauma surgery, orthopedics, plastics, ENT etc.) Typically they went to the operating room the day after arrival for evaluation of their wounds and to begin the next phases of treatment, whether it was to cover a massive soft tissue defect or to revise an amputation, which had already been done. One of the huge challenges that occurred in the trauma theater was determining if a limb could be salvaged or not. There was every effort made to salvage as much as possible; however, most patients became amputees immediately at the time of injury from the blast. The skill of the doctors, nurses and support staff who were deployed to treat the wounded is unparalleled.
At Walter Reed, there were multiple groups of specialized teams both inpatient and outpatient who worked on the patients independently and also cooperatively together to devise the plan of care and rehabilitation. Multidisciplinary team inpatient trauma rounds took place twice weekly, usually the day after a Medevac arrived with a new group of injured. Trauma rounds were run by the trauma service; but here is a small list of people/teams who attended:
– Trauma Surgery
– Orthopedic Surgery
– Physical Medicine and Rehabilitation
– Wound Team
– Psychiatric Consult Liaison Service
– Nutrition- Social Work
– Nursing representatives from each unit
– Representatives from the Army, Navy, Marines and Air Force from the various squads
– Inpatient Occupational and Physical Therapy
– Speech Language Therapy
– Veterans Affairs
– Administration
– The Medevac Office
– Family Liaisons
– Warrior Clinic
This list is not exhaustive, but it illustrates how many people were needed to coordinate care properly. Approximately 40 people were in each meeting, and all patients on the trauma service were discussed. The trauma team members led the rounds, but anyone who attended was able to voice a concern or an issue that needed addressing. In the interest of time, if a particular service member was especially complex, the appropriate teams stayed after to discuss the issues together.
The majority of the patients did not have an easy treatment course as the injuries were not only physical with fresh amputations and massive soft tissue injuries, but they also had Traumatic Brain Injuries (TBI), other brain injuries in additionto the psychological trauma of what happened to them to treat. Frequently, the most challenging issue was a logistical/military one or the coordination of moving family members from their home to the bedside and then with the patient if they went to an acute rehab center. This is why it was necessary to have members of the military battalions (each patient was assigned once they came stateside) as well as the VA and social work present.
From the multidisciplinary team rounds, there were also weekly rounds by other teams both inpatient and outpatient. The amputee rounds were comprised of the attending ortho trauma surgeon, wound care, PM&R, PT, OT and the prosthetists. The TBI team was comprised of neurology, psychiatry, psychology, PT, OT, social work, case managers and other specialists. All teams were in constant communication with each other and the formal structure was key. Additionally, each patient had to undergo a set of consults upon arrival to ensure there were no hidden issues. Each patient was seen by dental, wound care, TBI and other specialties for screening. Wound care was added in the later years of the war after a series of pressure ulcers on the sacrum, as well as the occiput, were noted from the long duration of travel between countries on gurneys. By coordinating care between locations, as well as with the flight nurses, that issue was extremely rare towards the end of the war and certainly the severity was much decreased.
LESSONS LEARNED
IThe complex care received by the troops was a testament to the system that was placed to provide multi-disciplinary complete care. Several points can be made for other teams who wish to emulate a similar approach.
1.Know who the primary team is and who is communicating the messages. Traumatic injuries affect not only the patient, but also the family members and care givers who arrive to take care of their loved ones. Emotions and stress levels run high, and mixed messages often had deleterious effects on keeping the focus on the recovery of the patient, They also made a very challenging working environment for the staff members.
2.If there was an issue noted by a specialty team, direct contact needed to be made with the primary team. Again, mixed messages or issues lost to follow up created a lot of problems to resolve in a less than easy manner.
3.Include the inpatient nursing staff in the treatment plans for the patient. For the outpatients, each was assigned a nurse case manager to coordinate care, and they needed updates as well.
4.Comprehensive personalized compassionate care can be provided by a multitude of specialty teams who all bring their expertise to solve pieces of a larger problem. As long as everyone is working towards the same overall goals, the system and the teamwork will achieve great outcomes for their patients.
References
1. Fischer, H. (Aug 7, 2015) A Guide to U.S. Military Casualty Statistics: Operation Freedom’s Sentinel, Operation Inherent Resolve, Operation New Dawn, Operation Iraqi Freedom, and Operation Enduring Freedom. Congressional Research Service 7-5700 www.crs.gov RS22452.
2. Goldberg, MS. December 2014. Updated Death and Injury Rates of U.S. Military Personnel During the Conflicts in Iraq and Afghanistan. Working Paper 2014-08. Working Paper Series Congressional Budget Office Washington, DC. www.cbo.gov

