Dr. Dardano’s career began in Utica, New York. He completed his undergraduate studies in Syracuse, New York, and traveled to South Florida to attend medical school. Dr. Dardano studied general surgery at Sinai Hospital of Wayne State University in Detroit and completed five years of training which resulted in his board certification by the American Board of Surgery. He has been active both clinically and academically and has performed over 1,300 plastic surgery procedures during his training, and is the author and co-author of several papers and textbook chapters. He has presented his work at the prestigious Plastic Surgery Research Council, as well as the American College of Surgeons, and the American Society of Aesthetic Plastic Surgeons. He has also lectured internationally.

Dr. Klapper is a graduate of the NYU Institute of Reconstructive Plastic Surgery. After practicing on Manhattan’s 5th Ave, he joined the teaching faculty of Florida Atlantic University. He has authored numerous clinical papers winning National and International awards for his research in cutting edge wound care techniques. He is the founding member of the Palm Beach County Wound Society and the plastic surgeon for the Level 1 trauma team at Delray Medical Center.
Dr. Moradian is completing his last year in General Surgery at Larkin Community and Palm Springs Hospital where he serves as the Chief Surgical Resident. Throughout his years of training, he placed an emphasis on research and presenting at numerous conferences. During his residency, he has published and presented in over 15 areas of surgery spanning from plastic to general surgery. Dr. Moradian enjoys golfing, diving, running with his dog Tyson, snowboarding, and spending time with his loved ones.
Dardano, Klapper and Moradian_Current Dialogues in Wound Management_2018_Volume 4_Issue 2
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
ABSTRACT
PURPOSE: To develop a tissue salvage technique to reconstruct acute wounds in patients with associated comorbidities that designated them as patients at high risk for complications in the operating room (OR). Additionally, such wounds upon presentation did not afford tissue for salvage.
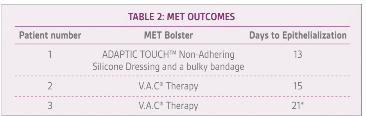
METHODS: Three acute full thickness wounds in series were treated at a Level 1 trauma center. Wounds varied in size and complexity (10 cm2 to 150 cm2) and patients aged 88 to 96 years old, each with complex medical histories designating them at high-risk for complications during general anesthesia. MET grafts were harvested sharply with scissors from the wound edge, minced into small islands of skin with scissors and manually placed onto the wound bed. Grafts were bolstered with either ADAPTIC TOUCH™ Non-Adhering Silicone Dressing and secondary bandage or V.A.C.® Therapy.
RESULTS: All wounds showed full (100%) closure with epithelialization. No failures or infections. Healing time to closure: 10-15 days dependent on size of initial wound.
CONCLUSION: The Minced Edge Transposition (MET) graft is an easy to master, low cost, bedside technique for the wound care surgeon. MET has become our primary technique to expedite wound closure in patients presenting with unsalvageable tissue and high operative risk secondary to comorbidities.
INTRODUCTION
Aggressive management to accelerate wound epithelialization is especially important in the geriatric trauma patient. Such patients may be at higher risk for the operating room secondary to their associated comorbidities and at higher risk for complications the longer they are hospitalized. Tissue salvage techniques are an especially important tool for accelerated wound management in this population.
Typically, large open wounds are debrided and the wound bed prepared for a skin graft, tissue flap or managed to heal secondarily. Despite the tried-and-true nature of these techniques, it ignores the morbidity and impact on the quality of life for elderly patients who are particularly susceptible to stressors.
Out of the necessity for speedy wound resolution in the geriatric population, we developed an acute technique which can be performed at the bedside upon presentation, and which we have learned can be used on patients with multiple comorbidities. The technique is the evolution of our Minced Expansion Graft (MEG), which is a tissue salvage technique introduced for partial thickness skin tears salvaging the patient’s own tissue with avoidance of a donor site. The technique introduced here involves the excision, mincing, and transposition of a sliver of wound edge as individual micro grafts into the wound. We call this technique the Minced Edge Transposition (MET) graft. Like the MEG, the MET technique has accelerated healing times and lowered the vertical healthcare treatment cost.
MATERIALS AND METHODS
In this pilot series, three acute full thickness wounds were treated at a Level I trauma center. Each wound varied in size and complexity (10 cm2to 150 cm2). The patients aged from 88 to 96 years old, each with complex medical histories allotting for high risk for general anesthesia (Table 1). American Society of Anesthesiologist Physical Status Classification Scores (ASA Scores) ranged from III, IV, V and E 1. Individual patient medical comorbidities included atrial fibrillation, anticoagulation medication use, traumatic brain injury, long bone injuries, respiratory failure, as well as intra-abdominal injuries. All traumatic wounds treated were low to moderate impact soft tissue trauma with minimal contamination. Exclusion criteria
 Step 1: After Debridement, Full Thickness 2-3mm Sliver of Skin is Harvested from one Edge of the Wound
Step 1: After Debridement, Full Thickness 2-3mm Sliver of Skin is Harvested from one Edge of the Wound Step 2: Tissue is Minced with Scissors to Smallest Achievable Units (we refer to these units as Micro-Grafts)
Step 2: Tissue is Minced with Scissors to Smallest Achievable Units (we refer to these units as Micro-Grafts)
 Step 3: Micro-Grafts of Tissue are Placed Evenly about the Wound Bed
Step 3: Micro-Grafts of Tissue are Placed Evenly about the Wound Bed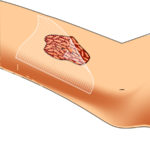 Step 4: An Interface Dressing is Placed and Left untouched for One Week (ADAPTIC TOUCH™ NonAdherent Silicone Dressing [Systagenix, an ACELITY Company, Gargrave, UK] covered with either secondary occlusive dressings, 4×4 Gauze, rolled gauze and selfAdherent Wrap or bolstered with V.A.C.® Therapy
Step 4: An Interface Dressing is Placed and Left untouched for One Week (ADAPTIC TOUCH™ NonAdherent Silicone Dressing [Systagenix, an ACELITY Company, Gargrave, UK] covered with either secondary occlusive dressings, 4×4 Gauze, rolled gauze and selfAdherent Wrap or bolstered with V.A.C.® Therapy
Figure 1: MET Graft Technique
included high-impact grossly contaminated wounds. In each case, the patient underwent MET Grafting [Fig 1]. Of the 3 patients included in the series, case reports are provided to further explore the applicability and usefulness of this technique for the wound care surgeon.
CASE REPORT 1
A 96-year-old female status-post fall from a chair on rivaroxaban secondary to an extensive cardiac history along with advanced dementia was referred to our service with a 5×12 cm acute open wound (Fig. 2) that occurred three days earlier. The edges of the wound could not be approximated; therefore, informed consent was obtained for the patient to undergo MET grafting. After debridement and undergoing the steps of MET grafting (Fig. 3), using the ADAPTIC TOUCH™ Non-Adhering Silicone Dressing and a secondary bandage on day 13 she had nearly 100% epithelialization with inter-mixed areas of scabbing (Fig. 4).
 Figure 2: 5×12 cm acute open wound on initial presentation
Figure 2: 5×12 cm acute open wound on initial presentation Figure 3: 2.5 mm strip of skin harvested from one edge and minced at bedside. These micro grafts, were transposed to the wound bed and evenly dispersed
Figure 3: 2.5 mm strip of skin harvested from one edge and minced at bedside. These micro grafts, were transposed to the wound bed and evenly dispersed
CASE REPORT 2
The plastic surgery service received a consult for an 88-year-old female on warfarin secondary to a history of atrial fibrillation after suffering a subdural hematoma requiring subsequent intubation secondary to respiratory failure. The patient had comorbidities of chronic kidney disease and diabetes mellitus type II. The wound measured approximately 4x9cm (Fig. 5) and the patient was deemed too high-risk for the operating room. She underwent MET grafting with application of V.A.C.® Therapy (Fig. 6) and at approximately the 6-week mark post grafting had 100% epithelialization (Fig. 7)
 Figure 5: The 4x9cm acute open wound on initial presentation
Figure 5: The 4x9cm acute open wound on initial presentation Figure 6: 2mm sliver of skin harvested and minced into micro grafts and applied to the wound bed
Figure 6: 2mm sliver of skin harvested and minced into micro grafts and applied to the wound bed
CASE REPORT 3
A 92-year-old male on warfarin for atrial fibrillation was traumatized by a storm shutter falling on his head and left upper extremity. The patient is a dialysis patient with chronic kidney disease. He suffered an intracranial injury and an avulsion to the left forearm wound which measured 15x10cm (Fig. 8). This patient was not cleared for the operating room. He underwent MET grafting with application of V.A.C.® Therapy in the trauma bay (Fig. 9). On day 7 (Fig.10) excellent take of the grafts was observed. At day 21 the wounds showed 100% epithelialization (Fig. 11). The patient may have closed earlier but surgeon’s follow-up was at 21 days.
 Figure 7: At ~6 weeks post grafting, the wound was 100% epithelialized
Figure 7: At ~6 weeks post grafting, the wound was 100% epithelialized
RESULTS
All three patients in the case series achieved 100% closure (Table 2). Of note, 1 of the 3 patients developed hybrid wound healing of epithelialization with small areas of scab eschar between the micro grafts, which for the purposes of this pilot study we consider biologic closure. In this one case of scabbing, the tissue went on to epithelialize. Additionally, there were no failures or infections. Time to closure was approximately 13-21 days depending on the original size of the wound and grafts.
DISCUSSION
Physiologically, older patients exhibit an age-related delay in re-epithelialization, collagen synthesis, and angiogenesis 2- 6.There is a decrease in the size and response of fibroblasts in the geriatric population with a decreased response to growth factors and other chemokines. Such change in fibroblast function delays healing times
Unlike partial thickness wounds, full thickness wounds epithelialize from their edges8. For the geriatric patient, large wounds that heal secondarily can be a prolonged ordeal fraught with morbidity and diminished quality of life.MET Grafts have specific advantages:
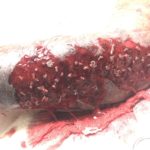 Figure 10: On post procedure day 7, islands of skin in wound was observed
Figure 10: On post procedure day 7, islands of skin in wound was observed Figure 11: Complete epithelialization by day 21
Figure 11: Complete epithelialization by day 21
1.The increased surface area in contact with the wound bed helps improve plasmatic imbibition which ultimately increases survival of each individual graft.
2.Sub-graft collections are avoided as wound excretions seep around rather than get trapped underneath the small islands of grafted tissue. Such collections would result in the demise of the graft.
3.Partial failure of one individual micro-graft does not affect survival of the remaining grafts. Each graft acts as its own entity dependent on nutrient extraction from the underlying wound bed.
4.Due to the small size of the island grafts they are less impacted by the shearing forces that would normally cause failure in meshed or sheet grafts. Because of this, the MET graft does not require traditional bolstering.
5.Due to the small size, epidermal-dermal surface orientation does not impact epithelialization
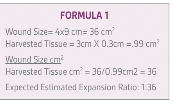
Postal stamping technique described on burn wounds by Meeks and his colleagues have demonstrated expansion ratios of approximately 1:9 with claims today of up to 1:10013-15. The MET technique has successfully allowed expansion ratios of up to 1:36 [Formula 1].
CONCLUSION
The population over 65 years of age is the fastest growing population in the United States16. Having a complete repertoire for the treating surgeon when faced with acute open wounds in this population is key in an era where emphasis on quality care and cost co-exist. The use of devices in other grafting techniques can cost thousands of dollars17-18 and when compared to the MET techniquethe most expensive item is arguably the suture removal kit or dressing interface.
In the authors’ work with acute wounds in the geriatric population, the MEG technique evolved into the MET graft. This evolution allows efficacious care to our critically wounded with soft tissue restoration while avoiding operative morbidity. The speed of healing improves quality of life and decreases the comorbidities of prolonged recovery. The technique and its shortened recovery have the added benefit of vertical healthcare savings. Moving forward, a cost-base analysis must be undertaken to fully appreciate the savings that can be gained, as well as a multicenter clinical study to repeat our results.
From our work, MET grafting is a technique that accelerates epithelialization and is widely used in our trauma program in all ages. In our experience, the MET graft is an easy technique for all specialties of wound care to perform and has the potential to deliver positive outcomes. We believe it will be a valuable addition to the armamentarium for all surgeons.
References
1.ASA House of Delegates. “ASA Physical Status Classification System.” American Society of Anesthesiologists. 15 Oct. 2014. Web. 18 Mar. 2017.
2.Gosain, A. & DiPietro, L. Aging and Wound Healing. World J. Surg. (2004) 28: 321.
3.Swift, Mari E., Hynda K. Kleinman, and Luisa A. DiPietro. “Impaired wound repair and delayed angiogenesis in aged mice.” Laboratory investigation; a journal of technical methods and pathology 79.12 (1999): 1479-1487.
4.West, Michael D. “The cellular and molecular biology of skin aging.” Archives of dermatology 130.1 (1994): 87-95.
5.Bruce, Sarah A., and Scott F. Deamond. “Longitudinal study of in vivo wound repair and in vitro cellular senescence of dermal fibroblasts.” Experimental gerontology 26.1 (1991): 17-27.
6.Butcher, Earl O., and Jules Klingsberg. “Age, gonadectomy, and wound healing in the palatal mucosa of the rat.” Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 16.4 (1963): 484-493.
7.Plisko, Andy, and Barbara A. Gilchrest. “Growth factor responsiveness of cultured human fibroblasts declines with age.” Journal of gerontology 38.5 (1983): 513-518.
8.Surgery: Basic Science and Clinical Evidence, 2e, chapter 10. Wounds: Biology, Pathology, and Management
9.Zuhaili, Baraa et al. “Meshed Skin Grafts Placed Upside down Can ‘take’ If Desiccation Is Prevented.” Plastic and reconstructive surgery 125.3 (2010): 855- 865. PMC. Web. 18 Mar. 2017.
10.Van Den Bogaerdt, A. J., Ulrich, M. M. W., Van Galen, M. J. M., Reijnen, L., Verkerk, M., Pieper, J., amme, E. N. and Middelkoop, E. (2004), Upside- down transfer of porcine keratinocytes from a porous, synthetic dressing to experimental full-thickness wounds. Wound Repair and Regeneration, 12: 225- 234.
11.Svensjo T, Pomahac B, Yao F, Slama J, Wasif N, Eriksson E. Autologous skin transplantation: comparison of minced skin to other techniques. J Surg Res. 2002 Mar; 103(l):19-29.
12.Hackl F, Bergmann J, Granter SR, et al. Epidermal regeneration by micrograft transplantation with immediate 100-fold expansion. Plast Reconstr Surg. 2012;129(3):443e-52e.
13.Hackl F, Kiwanuka E, Philip J, Gerner P, Aflaki P, Diaz-Siso JR et al. Moist dressing coverage supports proliferation and migration of transplanted skin micrografts in full-thickness porcine wounds. Burns 2014;40:274-80.
14.Kreis RW, Mackie DP, Vloemans AW, Hermans RP, Hoekstra MJ. Widely expanded postage stamp skin grafts using a modified Meek technique in combination with an allograft overlay. Burns 1993;19:142-5.
15.Raff T, Hartmann B, Wagner H, Germann G. Experience with the modified Meek technique. Acta Chir Plast 1996;38:142-629.
16.U.S. Census Bureau. Census 2000. U.S. Census Bureau, Washington, DC, 2000
17.Munster AM, Smith-Meek M, Sharkey P. The effect of early surgical intervention on mortality and cost-effectiveness in burn care, 1978-91. Burns 1994;20:61-4
18.Kadam, Dinesh. “Novel Expansion Techniques for Skin Grafts.” Indian Journal of Plastic Surgery : Official Publication of the Association of Plastic Surgeons of India 49.1 (2016): 5-15. PMC. Web. 18 Mar. 2017.