Dr. Lee Rogers is a fellowship-trained podiatrist in limb salvage. He is the medical director
of the Amputation Prevention Center at Sherman Oaks Hospital in Los Angeles.
Rogers_Current Dialogues in Wound Management_2015_Volume 1_Issue 1
ONE of the key concepts in wound healing is removing the external pressure from an ulcerated area. In order to heal the wound, one must consider the type, source, and location of the pressure.1 External pressure is essentially trauma and leads to ulceration in a variety of ways. A nail puncture would be an example of high pressure-short duration trauma. Low pressure-long duration trauma can occur with extended contact with a surface resulting in a decubitus ulcer, but the typical diabetic foot ulcer is due to moderate pressure-moderate duration trauma from repetitive stress (walking) on an insensate foot. Offloading a plantar diabetic foot ulcer reduces the pressure and strain.2 There are several effective methods of offloading, including total non-weight-bearing, as with bed rest, wheel chair or crutches. However, people with foot ulcers tend to have other issues, and reduced skin integrity and chronic bed rest can lead to other ulcers. Wheelchairs may not be convenient in the home or conducive to the patient’s lifestyle. Patients with diabetes are often obese and have proprioceptive impairment risking falls with crutches. Also, ambulating properly with crutches requires a lot of energy and cardiovascular reserves not present in those with diabetes. Other modalities for offloading include total contact casts (TCC), removable cast walkers, custom bracing and orthotics, half shoes, or rigid post-operative shoes.Recently, a multidisciplinary panel of experts convened and created consensus guidelines on offloading the diabetic foot ulcer. The panel resulted in several consensus statements; the most notable are described below.3
Vascular management, infection management and prevention, and pressure relief are essential to the healing of diabetic foot ulcers
No treatment works in isolation. While offloading is of utmost importance, vascular 4 and infection 5 must also be managed to ensure positive outcomes as they are impediments to wound healing.
For guidance on offloading the Charcot foot, the panel endorsed the Charcot foot in diabetes consensus report published in 2011.
Offloading the Charcot foot is extremely complex due to muscle tendon imbalances and dislocations or fractures.In many cases, surgery may be necessary. The International Task Force on the Charcot Foot published a consensus document in 2011 that is an excellent primer on the diagnosis and treatment of the condition, including offloading options.6
Total contact casting (TCC) is the preferred method for offloading plantar diabetic foot ulcers as it has consistently demonstrated the best healing outcomes and is a cost-effective treatment.
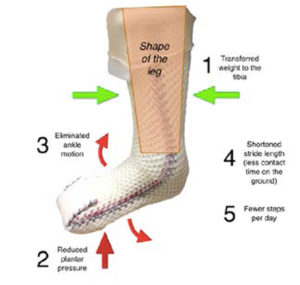
The expert panel reviewed all techniques of offloading, and the evidence clearly indicates the TCC is the best method of offloading the diabetic
foot ulcer. The TCC works in several ways (Figure 1). Based on its shape, it transfers plantar pressure to the tibia.7 It immobilizes the ankle, reducing propulsion and peak plantar pressure on the forefoot. It reduces shearing of the plantar foot skin. Finally, it is cumbersome to walk with, so it reduces the patient’s number of steps per day.8 All these factors combined reduce the plantar pressure and the strain rate. The use of TCC is supported by several quality randomized – controlled studies.9, 10; TCC also reduced the cost to heal a foot ulcer by half in a large retrospective study of data from the U.S. Wound Registry.11
There currently exists a “gap” between the evidence supporting the efficacy of diabetic foot ulcer offloading and what is actually performed in clinical practice.
Unfortunately, in spite of the best evidence, there is a large evidence-practice gap in the use of offloading andTCC for diabetic foot ulcers.12 In both the US and Europe, the best methods of offloading are often not employed. This can be because the use of TCCs is too time consuming or requires special training, but its effect is that wound healing is delayed due to ineffectual offloading.
Advanced therapeutics are unlikely to succeed in improving wound healing outcomes unless effective offloading is achieved.
There are many advanced therapeutics used to treat the diabetic foot ulcer ranging from growth factors, negative pressure wound therapy and, of course, cellular and tissue-based products. All these products have two things in common:they are expensive; and they will not succeed without good offloading.13 It is counterproductive to use an expensive piece of tissue only to have it sheared off by pressure if offloading is not assured.Thus, offloading assists these products in doing their jobs.
Summary
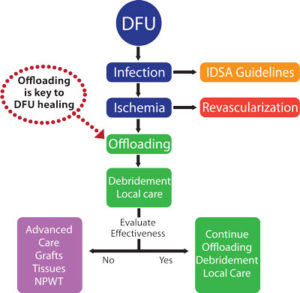
Many factors are involved in treating a diabetic foot ulcer, but offloading is one of those basic concepts that cannot be overlooked. Figure 2 is a typical evidence-based algorithm for the treatment of the diabetic foot ulcer. While offloading is paramount, other factors such as infection5 and peripheral vascular disease14 also need to be considered.15
Figure 2. Evidence-based flowchart for the treatment of diabetic foot ulcers emphasizing the component of offloading.
References
References:
1.Bus SA. Priorities in offloading the diabetic foot.Diabetes Metab Res Rev. Feb 2012;28 Suppl 1:54-59.
2.Snyder RJ, Lanier KK. Offloading difficult wounds and conditions in diabetic patient. Ostomy Wound Manage.Jan 2002;48(1):22-28, 30, 32-25.
3.Snyder RJ, Rogers LC, Frykberg RG. The management of diabetic foot ulcers through optimal offloading. Building consensus guidelines and practical recommendations to improve outcomes. J Am Podiatr Med Assoc. Nov/Dec 2014, in press.
4.Gibbons GW, Shaw PM. Diabetic vascular disease: characteristics of vascular disease unique to the diabetic patient. Semin Vasc Surg. Jun 2012;25(2):89-92.
5. Lipsky BA, Berendt AR, Cornia PB, et al. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. Jun 2012;54(12):e132-173.
6.Rogers LC, Frykberg RG, Armstrong DG, et al. The Charcot foot in diabetes. Diabetes Care. Sep 2011;34(9):2123-2129.
7. Wertsch JJ, Frank LW, Zhu H, et al. Plantar pressures with total contact casting. J Rehabil Res Dev. Oct 1995;32(3):205-209.
8.Jimenez A. Total contact casting. (Update 2003): The Podiatry Institute; 2003:282-287
9.
Nabuurs-Franssen MH, Sleegers R, Huijberts MS, et al. Total contact casting of the diabetic foot in daily practice: a prospective follow-up study. Diabetes Care.Feb 2005;28(2):243-247.
10. Katz IA, Harlan A, Miranda-Palma B, et al. A Randomized Trial of Two Irremovable Offloading Devices in the Management of Neuropathic Diabetic Foot Ulcers. Diabetes Care. 2005;28:555-559.
11.Fife CE, Carter MJ, Walker D. Why is it so hard to do the right thing in wound care? Wound Repair Regen. Mar-Apr 2010;18(2):154-158.
12.Wu SC, Jensen JL, Weber AK, Robinson DE, Armstrong DG. Use of pressure offloading devices in diabetic foot ulcers: do we practice what we preach? Diabetes Care. Nov 2008;31(11):2118-2119.
13.Kashefsky H, Marston W. Total contact casting combined with human fibroblast-derived dermal tissue in 15 DFU patients. J Wound Care. May 2012;21(5):236, 238, 240,242-233.
14.Schaper NC, Andros G, Apelqvist J, et al. Diagnosis and treatment of peripheral arterial disease in diabetic patients with a foot ulcer. A progress report of the International Working Group on the Diabetic Foot. Diabetes Metab Res Rev. Feb 2012;28 Suppl 1:218-224.
15.Snyder RJ, Kirsner RS, Warriner RA 3rd, et al. Consensus recommendations on advancing the standard of care for treating neuropathic foot ulcers in patients with diabetes. Ostomy Wound Manage. Apr 2010;56(4Suppl):S1-24.